Treating Bladder Cancer That Progresses Or Recurs
If cancer continues to grow during treatment or comes back after treatment , treatment options will depend on where and how much the cancer has spread, what treatments have already been used, and the patient’s overall health and desire for more treatment. Its important to understand the goal of any further treatment if its to try to cure the cancer, to slow its growth, or to help relieve symptoms as well as the likely benefits and risks.
For instance, non-invasive bladder cancer often comes back in the bladder. The new cancer may be found either in the same place as the original cancer or in other parts of the bladder. These tumors are often treated the same way as the first tumor. But if the cancer keeps coming back, a cystectomy may be needed. For some non-invasive tumors that keep growing even with BCG treatment, and where a cystectomy is not an option, immunotherapy with pembrolizumab might be recommended.
Cancers that recur in distant parts of the body can be harder to remove with surgery, so other treatments, such as chemotherapy, immunotherapy, targeted therapy, or radiation therapy, might be needed. For more on dealing with a recurrence, see Understanding Recurrence.
What Is The Difference Between High Grade And Low Grade Bladder Cancer
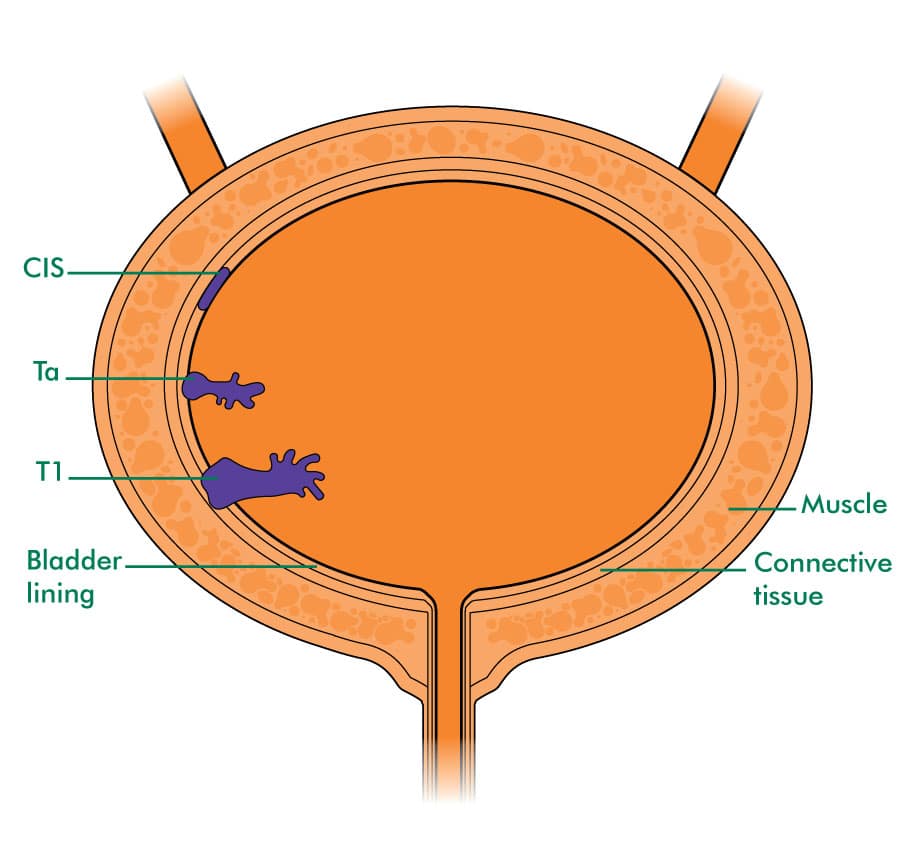
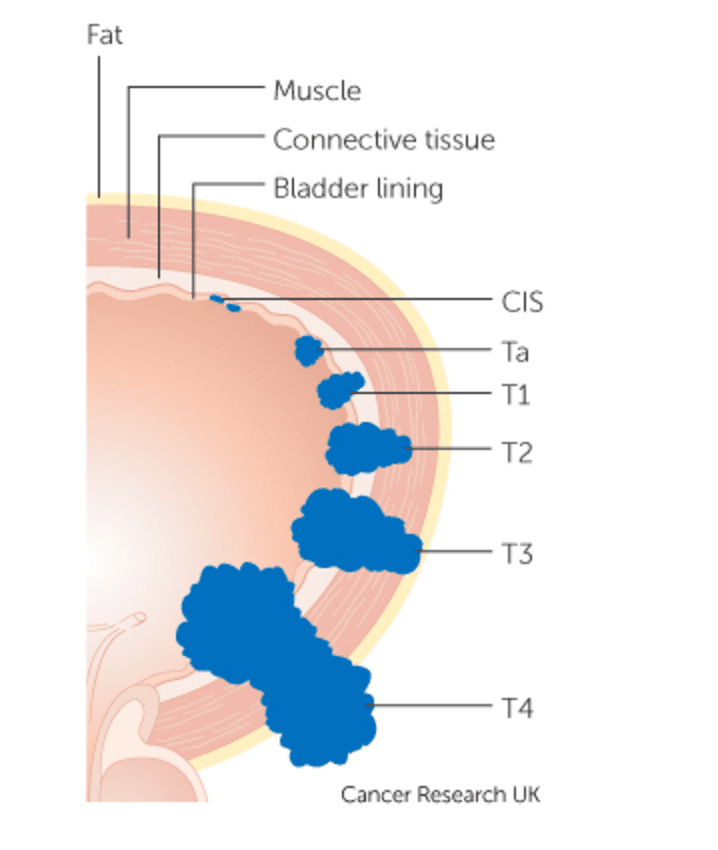
Low grade and high grade bladder cancer 1 Low-grade bladder cancer means the cancer has not invaded the muscles around the bladder . People rarely die from this type of bladder cancer, it often recurs after treatment. 2 High-grade bladder cancer also often recurs and has a higher chance of spreading to other parts of the body. Almost all deaths from bladder cancer result this type so it is treated more aggressively.
Computed Tomography Urography And Intravenousurography
Computed tomography urography is used to detect papillary tumours inthe urinary tract, indicated by filling defects and/or hydronephrosis .
Intravenous urography is an alternative if CT isnot available , but particularly in muscle-invasivetumours of the bladder and in UTUCs, CT urography provides more information .
The necessity to perform a baseline CT urography once abladder tumour has been detected is questionable due to the low incidence of significantfindings obtained . The incidence of UTUCs is low, but increases to 7.5% in tumours located in the trigone . The risk of UTUC during follow-up increases in patients with multiple- andhigh-risk tumours .
Also Check: Over The Counter Bladder Medication
Read Also: Women’s Bladder Control Medication
Who Treats Bladder Cancer
Based on your treatment options, you might have different types of doctors on your treatment team. These doctors could include:
- Urologists: surgeons who specialize in treating diseases of the urinary system and male reproductive system
- Radiation oncologists: doctors who treat cancer with radiation therapy
- Medical oncologists: doctors who treat cancer with medicines such as chemotherapy and immunotherapy
You might have many other specialists on your treatment team as well, including physician assistants, nurse practitioners, nurses, nutrition specialists, social workers, and other health professionals.
Intravesical Bcg Therapy For High
If patients with high-grade T1 disease have a low risk of progression, bladder sparing management should be considered. BCG instillation into bladder is the gold standard for conservative treatment for high-grade T1 disease. The therapeutic effect of BCG in high-grade T1 has already been established by several meta-analysis studies . However, we have to keep in mind that patients die upon progression to MIBC, not upon recurrence, and that the effectiveness of BCG at preventing progression was not as great as its effectiveness at preventing recurrence. In addition, BCG therapy may be associated with severe side effects with local or systemic symptoms. For that reason, the ability to predict the response to treatment before BCG instillation would be an invaluable tool in the selection of appropriate therapeutic modalities.
You May Like: Surgery For Prolapsed Uterus And Bladder
Treatment Of Stage I Bladder Cancer
In This Section
TUR with fulguration followed by an immediate postoperative instillation of intravesical chemotherapy
TUR and fulguration are the most common and conservative forms of management. Careful surveillance of subsequent bladder tumor progression is important. Because most bladder cancers recur after TUR, one immediate intravesical instillation of chemotherapy after TUR is widely used. Numerous randomized, controlled trials have evaluated this practice, and a meta-analysis of seven trials reported that a single intravesical treatment with chemotherapy reduced the odds of recurrence by 39% .
TUR with fulguration
Staging a bladder cancer via TUR is based on the extent of invasion. To assess whether cancer has invaded the muscle, muscularis propria must be present in the resected tissue. While a repeat TUR is generally considered mandatory for T1 and high-grade noninvasive bladder cancers if no muscularis propria is present in the resected tissue from the first TUR, many experts recommend that a second TUR be routinely performed within 2 to 6 weeks of the first TUR to confirm staging and achieve a more complete resection. The rationale for this derives from numerous findings, including the following:
Evidence :
Evidence :
Evidence :
Evidence :
Evidence :
Evidence :
Individual Treatment Strategy In Primary Orrecurrent Tumours After Turb Without Previous Bcg Intravesical Immunotherapy
The type of further therapy after TURB should be based on the risk groupsshown in Section 6.3 and Table 6.1. The stratification and treatment recommendations arebased on the risk of disease progression. In particular in intermediate-risk tumours, the2006 EORTC scoring model may be used to determine a patientsindividual risk of disease recurrence as the basis to decide further treatment on.
Any decisions should reflect the following principles :
- Patients in the low-risk group have a negligible risk of disease progression. The singlepost-operative instillation of chemotherapy reduces the risk of recurrence and isconsidered as sufficient treatment in these patients.
- Patients in the intermediate-risk group have a low risk of disease progression . In these patientsone-year full-dose BCG treatment , or instillations of chemotherapy for amaximum of one year, is recommended. The final choice should reflect the individualpatients risk of recurrence and progression as well as the efficacy and sideeffects of each treatment modality.
- Patients in the high-risk group have a high risk of disease progression . In these patientsfull-dose intravesical BCG for one to three years , is indicated. The additional beneficial effectof the second and third years of maintenance should be weighed against its added costs,side-effects and problems connected with BCG shortage.
Figure 7.1: Treatment strategy in primary or recurrent tumourwithout previous BCG*
Recommended Reading: Does Botox Help Overactive Bladder
Treatment For Bladder Cancer In Raleigh And Wake Forest
If you or someone you love has bladder cancer, know that a full recovery is possible. Modern medicine and new treatments have made surviving bladder cancer the new norm. Make sure to research these treatments and think about which one is right for you. Then, talk to your doctor about your plan to beat this cancer and discuss your options. Taking care of your body is essential, so make sure to take the time you need to heal.
If you or someone you love has bladder cancer, contact us today. Our highly experienced oncology team can help you understand your treatment options.
What Are The Complications
At this stage, treatment will likely involve removing your bladder.
Without treatment, or if treatment fails, stage 3 bladder cancer can progress to invade distant tissues and organs.
When theres no sign of cancer, youre in a state of remission. Even if youve finished treatment, youll need plenty of follow-up care. Your doctor will provide a plan for recovery, which may include:
- information about late or long-term side effects
- diet, exercise, and self-care recommendations
- schedule for regular checkups
- schedule for bladder cancer tests and screening tests for other types of cancer
- information about signs of recurrence
Also Check: Bladder Cancer Spread To Liver
Developing A Treatment Plan
In cancer care, different types of doctors often work together to create a patients overall treatment plan that combines different types of treatments. This is called a multidisciplinary team. This team is usually led by a urologist, a doctor who specializes in the genitourinary tract, or a urologic oncologist, a doctor who specializes in treating cancers of the genitourinary tract. Cancer care teams include a variety of other health care professionals, such as physician assistants, nurse practitioners, oncology nurses, social workers, pharmacists, counselors, dietitians, and others.
Treatment options and recommendations depend on several factors, including:
-
The type, stage, and grade of bladder cancer
-
Possible side effects
-
The patients preferences and overall health
Your care plan also includes treatment for symptoms and side effects, an important part of cancer care.
The first treatment a person is given for advanced urothelial cancer is called first-line therapy. If that treatment stops working, then a person receives second-line therapy. In some situations, third-line therapy may also be available.
Adjuvant systemic therapy is treatment that is given after radical surgery has been completed. In bladder cancer, adjuvant therapy is usually cisplatin-based chemotherapy or treatment in a clinical trial. Neoadjuvant therapy is treatment that is given before surgery, such as cisplatin-based chemotherapy.
Treatments by type and stage of bladder cancer:
Signs And Symptoms Of Bladder Cancer
Sometimes bladder cancer doesnt have many symptoms. Signs or symptoms can include:
- blood in your urine
- pain or burning when passing urine
- not being able to pass urine when you need to.
Not everyone with these symptoms has bladder cancer. If you have any of these symptoms or are worried, always see your doctor.
You May Like: Can I Have A Bladder Infection Without Burning
Is A Second Tur Recommended
If patients are diagnosed with high-grade T1, a second TUR is strongly recommended regardless of the presence of muscle in specimens because of the possibility of understating due to incomplete resection . It provides more accurate pathological staging information, since persistent tumor in second TUR specimens can be detected in 33%-55% of patients . Even when muscle is seen in the initial TUR specimen, muscle invasion by urothelial cancer in the second TUR specimen can be detected in up to 10% of specimens . In addition, a second TUR promotes cancer control. In a randomized controlled study, a second TUR decreased the recurrence rate compared to a single TUR . Further, residual tumor in the second TUR specimen is associated with poor prognosis. Of 92 patients with residual T1 cancer in second TURs, 75 progressed to muscle invasion within 5 years compared to 49 of 260 who had no or non-T1 tumor detected on restaging TUR . The second TUR is recommended within 2 to 6 weeks after the initial resection. Because of the high incidence of carcinoma in situ in the prostatic urethra or duct, biopsy from the prostatic urethra is recommended if tumor is located on the trigone or bladder neck .
Risk Adjusted Surveillance And Follow
Guideline Statement 32
32. After completion of the initial evaluation and treatment of a patient with NMIBC, a clinician should perform the first surveillance cystoscopy within three to four months.
Discussion
The natural history of NMIBC is often characterized by recurrence, even for solitary, small, low-grade papillary tumors. At the time of first evaluation and treatment, none of the existent risk stratification tools or urinary biomarkers is sufficiently sensitive and specific to predict which patient will have an early tumor recurrence. Therefore, the only reliable way to know in a particular patient whether they are at risk for early recurrence is by cystoscopic visualization of the urothelium at a relatively early interval after the first treatment/resection. In addition, visualization at a relatively early interval allows the treating urologist to verify that the initial resection was complete. The Panel, therefore, felt that the first repeat cystoscopic evaluation should occur three to four months after the initial treatment and evaluation, regardless of the patientâs overall risk.
Guideline Statement 33
33. For a low-risk patient whose first surveillance cystoscopy is negative for tumor, a clinician should perform subsequent surveillance cystoscopy six to nine months later, and then annually thereafter surveillance after five years in the absence of recurrence should be based on shared-decision making between the patient and clinician.
Discussion
Discussion
You May Like: What To Take For Bladder Control
Whats The Treatment For Stage 3 Bladder Cancer
The standard treatment for stage 3 bladder cancer is surgery, usually in combination with other therapies.
Be sure to discuss your treatment goals with your doctor. Assess all the potential benefits and risks of each therapy. Some treatments aim for a cure. Others work to slow progression or relieve symptoms. The recommended treatment may depend on your overall health.
If cancer continues to progress or comes back during treatment, you may have to reconsider your options.
Living With Advanced Cancer
Advanced cancer usually means cancer that is unlikely to be cured. Some people can live for many months or years with advanced cancer. During this time palliative care services can help.
Most people continue to have treatment for advanced cancer as part of palliative care, as it helps manage the cancer and improve their day-to-day lives. Many people think that palliative care is for people who are dying but palliative care is for any stage of advanced cancer. There are doctors, nurses and other people who specialise in palliative care.
Treatment may include chemotherapy, radiation therapy or another type of treatment. It can help in these ways:
- slow down how fast the cancer is growing
- shrink the cancer
- help you to live more comfortably by managing symptoms, like pain.
Treatment depends on:
- how far it has spread
- your general health
You May Like: Is Cranberry Juice Good For Bladder Cancer
Treatment For Advanced Bladder Cancer
If bladder cancer has spread to other parts of the body, it is known as advanced or metastatic bladder cancer. You may be offered one or a combination of the following treatments to help control the cancer and ease symptoms:
- systemic chemotherapy
- radiation therapy.
Immunotherapy uses the bodys own immune system to fight cancer. BCG is a type of immunotherapy treatment that has been used for many years to treat non-muscle-invasive bladder cancer.
A new group of immunotherapy drugs called checkpoint inhibitors work by helping the immune system to recognise and attack the cancer. A checkpoint immunotherapy drug called pembrolizumab is now available in Australia for some people with urothelial cancer that has spread beyond the bladder. The drug is given directly into a vein through a drip, and the treatment may be repeated every 2 to 4 weeks for up to 2 years.
Other types of checkpoint immunotherapy drugs may become available soon.
What Are The Side Effects Of Chemo
The side effects of chemo depend on the type and dose of drugs given and how long they are taken. When chemo and radiation are given at the same time, side effects tend to be worse. Common side effects of chemo include: 1 Nausea and vomiting 2 Loss of appetite 3 Hair loss 4 Mouth sores 5 Diarrhea 6 Constipation 7 Increased risk of infections 8 Easy bleeding or bruising, even after minor cuts or injuries 9 Fatigue
Also Check: Medicine To Help Empty Bladder
There Are Different Types Of Treatment For Patients With Bladder Cancer
Different types of treatment are available for patients with bladder cancer. Some treatments are standard , and some are being tested in clinical trials. A treatment clinical trial is a research study meant to help improve current treatments or obtain information on new treatments for patients with cancer. When clinical trials show that a new treatment is better than the standard treatment, the new treatment may become the standard treatment. Patients may want to think about taking part in a clinical trial. Some clinical trials are open only to patients who have not started treatment.
Thinking About Taking Part In A Clinical Trial
Clinical trials are carefully controlled research studies that are done to get a closer look at promising new treatments or procedures. Clinical trials are one way to get state-of-the art cancer treatment. In some cases they may be the only way to get access to newer treatments. They are also the best way for doctors to learn better methods to treat cancer. Still, they’re not right for everyone.
If you would like to learn more about clinical trials that might be right for you, start by asking your doctor if your clinic or hospital conducts clinical trials.
You May Like: Can Bladder Infection Clear Up On Its Own
What Are The Different Types Of Bladder Cancer
Another grading system sometimes used for early bladder cancer. This divides bladder cancers into 4 groups: 1 urothelial papilloma means it is a non cancerous tumour 2 papillary urothelial neoplasm of low malignant potential means it is a very slow growing tumour that is unlikely to spread 3 low grade papillary urothelial carcinoma is a slow growing cancer that is unlikely to spread 4 high grade papillary urothelial carcinoma is a quicker growing cancer that is more likely to spread
What Is High Grade Urothelial Carcinoma
What Is High-Grade Urothelial Carcinoma? High-grade urothelial carcinoma is a type of bladder cancer that has a high risk of becoming aggressive and progressing, as stated by the John Hopkins University Department of Pathology. It is more likely to recur in the bladder, invade the muscle wall or spread to other parts of
Read Also: What Does Myrbetriq Do For The Bladder
Treatment Of Recurrent Bladder Cancer
For information about the treatments listed below, see the Treatment Option Overview section.
Treatment of recurrentbladder cancer depends on previous treatmentand where the cancer has recurred. Treatment for recurrent bladder cancer mayinclude the following:
- Radiation therapy as palliative therapy to relieve symptoms and improve quality of life.
- A clinical trial of a new treatment.
Use our clinical trial search to find NCI-supported cancer clinical trials that are accepting patients. You can search for trials based on the type of cancer, the age of the patient, and where the trials are being done. General information about clinical trials is also available.