The Stages Of Prolapse
The states of prolapse range from 0 to 4 . Stage 4 occurs when the organ involved is actually protruding out of the vaginal opening, and this does require surgical intervention. However, grades 1 through grade 3 can often be treated with a combination of physical therapy and supportive devices. The primary focus of physical therapy for these patients is often addressing the causative factors that lead to prolapse and supporting the weakened vaginal wall.
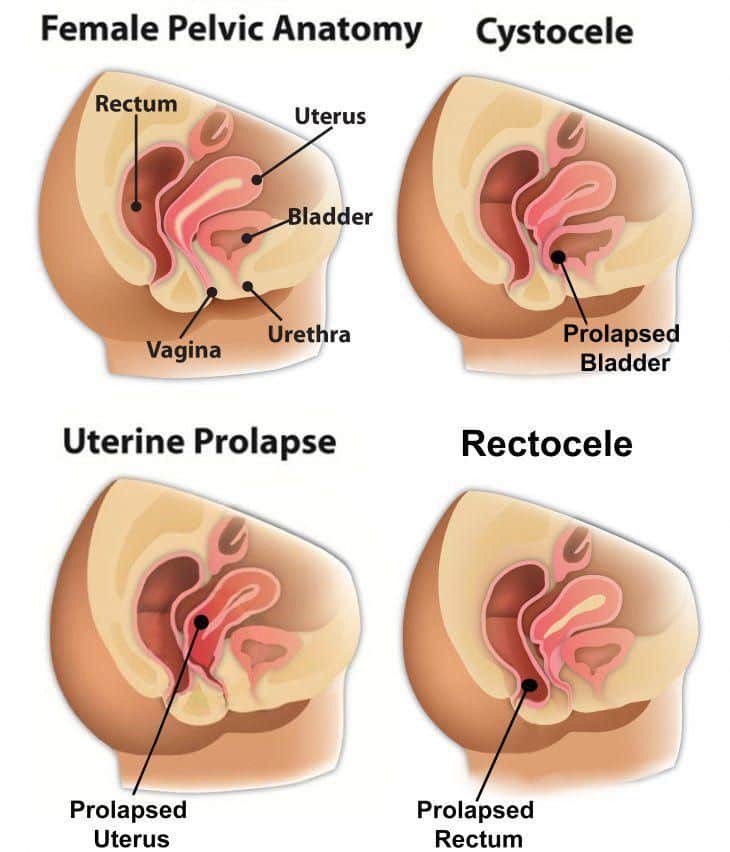
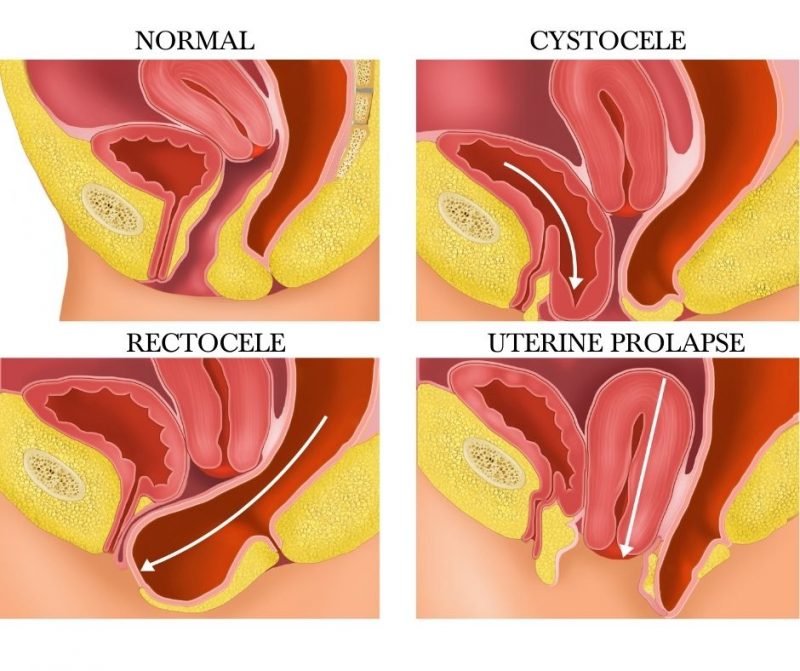
What Is A Prolapsed Bladder
Pelvic organ prolapse is a surprisingly common condition. In fact, its estimated that about half of women over 50 have some level of prolapse. The pelvic floor is a web of muscles and tissues that supports your pelvic organs, including the bladder, bowel, and uterus. When these muscles and tissues become weakened or damaged, one or more of these pelvic organs can drop or collapse, causing uncomfortable symptoms.
While any of the organs listed above can drop, the most common type of prolapse is a dropped bladder, also known as a cystocele.
How Common Is A Cystocele
A cystocele is common. Experts estimate that nearly half of women who have given birth have some degree of pelvic organ prolapse.1 However, many other women with the condition do not have symptoms or do not seek care from a health care professional. As a result, the condition is underdiagnosed, and it is not known exactly how many women are affected by cystoceles.
Also Check: What Causes Women’s Bladder Leakage
Exercises To Avoid With Prolapse
This is a very important list to generate for yourself, and it will look different from person to person.
From a clinical perspective:
- Ive seen women who can go to their CrossFit workout and their prolapse feels amazing afterwards.
- Ive also seen women who could go for a run if they were feeling symptomatic and it would help to resolve all their symptoms.
- On the other hand, Ive seen women where running or heavy lifting contributed to their prolapse and made it feel worse.
- Ive given out squats as treatment to help improve prolapse symptoms.
- Ive also taken squats out of someones lifting plan because they werent able to manage pressure well.
- Some women have a hard time sitting at work all day, and thats what makes their prolapse worse.
- Others can go for a run, but going to a spin class or for a swim makes them feel worse.
As you can see, safe is hard to define because its all in you do something, not you do.
I also find that just trying to live life can be much harder than exercise. Usually women are very mindful of pressure during their workout, but getting the stroller into the trunk or picking up a kid throwing a tantrum compromises their pelvic floor.
Let me give you an example of my list of things to avoid that made MY prolapse worse in the beginning.
As Pop Worsens You May Notice:
- The feeling of “sitting on a ball”
- Difficulty starting to urinate or a weak or spraying stream of urine
- Urinary frequency or the sensation that you are unable to empty the bladder well
- Lower back discomfort
- Urinary leakage with intercourse. Though unusual, severe prolapse can block the flow of urine and cause recurrent urinary tract infections or even kidney damage.
Read Also: Unable To Hold Bladder Female
How To Prevent Pelvic Organ Prolapse
“Women should lose weight if they’re overweight. They should stop smoking because it can lead to repetitive coughing,” Dr. Wakamatsu says. “And they should protect their pelvic floor by pulling in their lower abdominal muscles and tightening their pelvic floor muscles when they lift heavy objects.”
What Are The Risk Factors And Causes Of Bladder Prolapse
Childbirth is the most common cause of a prolapsed bladder. The childbirth delivery process is stressful on the vaginal tissues and muscles, which support a womans bladder.
Straining: Lifting heavy objects, straining during bowel movements, having a long-term condition that involves coughing, or having long-term constipation may damage the muscles of the pelvic floor.
Recommended Reading: Antibiotics For Bladder Infection While Pregnant
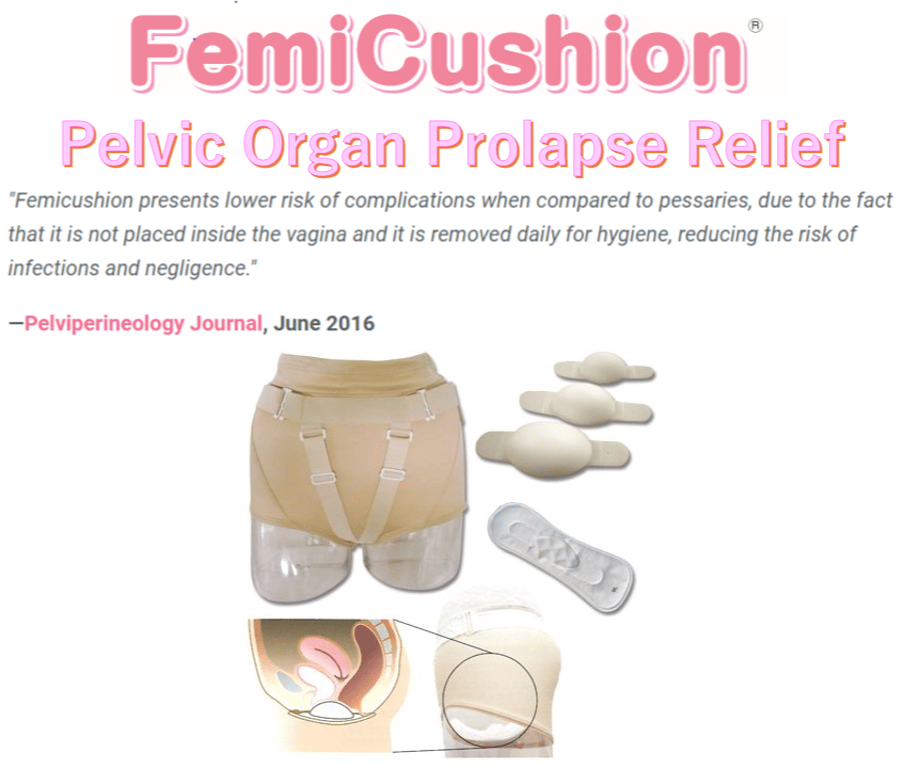
How Effective Are Pessaries
Well-fitting pessaries can support the pelvic organs in a way that reduces bladder and bowel problems or even makes them go away completely. They dont fix prolapses. But women dont always find a suitable pessary that is effective enough.
The use of a pessary is considered if, for instance, a woman wishes to avoid or delay surgery. About half of all women who use a pessary get by with it so well that they use it for several years or more. Pessaries can also be a good idea if pelvic floor exercises dont help enough on their own.
Safe Exercise With Prolapsed Bladder
Many everyday exercises can increase pressure on your pelvic floor and worsen your bladder prolapse symptoms or even contribute to repeat prolapse after already having had prolapse surgery. You need to make sure that you are fully informed about the exercises that are suitable for you if you are living with a prolapse.
1. Fitness exercises that reduce pressure on the pelvic floor
Fitness exercise should be low impact to reduce pressure on the pelvic floor. This means choosing exercises keeping one foot at least on the ground with exercise. This is quite different to high impact exercise such as running or jumping where both feet are off the ground. Low impact exercises include:
2. Strength training and abdominal exercises
Many everyday strength training and abdominal exercises have the potential to increase the downward pressure on the pelvic floor. These are some exercises to avoid with a bladder prolapse:
- Intense abdominal strength exercises and abdominal exercise machines which have the effect of increasing pressure on the pelvic floor
- Specific strength exercises such as leg press and wide leg squats that increase pressure on the pelvic floor and prolapse
- Heavy lifting and straining when lifting weights
- Breath holding when lifting weights-breathe out with the effort of lifting, pushing or pulling
- Plus sit on a ball or a bench for all your strength exercises wherever possible to support your pelvic floor
Also Check: Unable To Control Bowels And Bladder
Women Still Unaware Of Treatment Options
Unfortunately, many women dont know such treatments exist. And its not uncommon for women to tell Dr. Kawasaki theyve been experiencing discomfort for up to seven years.
A lot of times they dont mention it to a doctor because they think its a part of aging or the normal thing that happens after you have babies, Dr. Kawasaki said.
Uterine Prolapse: Causes Symptoms Diagnosis & Treatment
If you have a mild case of uterine prolapse, you may not have any obvious symptoms. However, as the uterus slips further out of position, it can place pressure on other pelvic organsâsuch as the bladder or bowelâand cause symptoms like: A feeling of heaviness or pressure in the pelvis. Pain in the pelvis, abdomen or lower back.
Recommended Reading: Icd 10 Code For Neurogenic Bladder
When To Seek Help
If you are concerned you may have a prolapsed bladder and are experiencing troublesome symptoms, see your doctor. You can also visit a physiotherapist who is trained to help you with pelvic floor exercises. If you are experiencing urinary incontinence associated with a prolapse, a continence nurse adviser may help.
How To Diagnose And Treat A Prolapsed Bladder
This article was medically reviewed by Lacy Windham, MD. Dr. Windham is a board certified Obstetrician & Gynecologist in Tennessee. She attended medical school at the University of Tennessee Health Science Center in Memphis and completed her residency at the Eastern Virginia Medical School in 2010, where she was awarded the Most Outstanding Resident in Maternal Fetal Medicine, Most Outstanding Resident in Oncology, and Most Outstanding Resident Overall.There are 12 references cited in this article, which can be found at the bottom of the page.wikiHow marks an article as reader-approved once it receives enough positive feedback. In this case, 96% of readers who voted found the article helpful, earning it our reader-approved status. This article has been viewed 131,694 times.
Experts say that your bladder may fall from it’s normal position in your pelvis if your pelvic floor becomes too weak or there’s too much pressure on it.XTrustworthy SourceMayo ClinicEducational website from one of the world’s leading hospitalsGo to source When this happens, your bladder presses on your vaginal wall, which is called a prolapsed bladder. Research suggests that as many as 50% of women have some form of bladder prolapse after pregnancy, so it’s a fairly common problem.XTrustworthy SourceHarvard Medical SchoolHarvard Medical School’s Educational Site for the PublicGo to source If you’re worried you have a prolapsed bladder, talk to your doctor because you have a range of treatment options.
Don’t Miss: How To Cope With Overactive Bladder
What Type Of Doctor Should I See For Pelvic Prolapse
Your doctor may recommend a specialist with certification in Female Pelvic Medicine and Reproductive Surgery , such as a gynecologist, a urologist or a urogynecologist, also known as a urogyn. A urogynecologist is a medical doctor who has completed a residency in obstetrics and gynecology or urology.
What Are The Complications Of A Cystocele
A cystocele may put pressure on or lead to a kink in the urethra and cause urinary retention, a condition in which you are unable to empty all the urine from your bladder. In rare cases, a cystocele may result in a kink in the ureters and cause urine to build up in the kidney, which can lead to kidney damage.
Read Also: Bladder Control Products By Mail
Risk Factors For Bladder Prolapse
Risk factors for bladder prolapse include anything that puts pressure on the pelvic floor and affects its function, such as:
- pregnancy and childbirth
- regularly straining on the toilet to pass bowel motions or empty the bladder
- being overweight
- chronic cough secondary to smokers cough or chronic lung diseases
- repetitive lifting of children or heavy weights at work or in the gym, or any exercises where there is excessive downward pressure on the pelvic floor
- pelvic or gynaecological surgery
- strong family history
- connective tissue disease, in which the tissues in the body are not able to hold the weight of the organs
What Is Uterine Prolapse
Uterine prolapse is a fallen down uterus or womb slipped out of position. It happens when the uterus loses the strong supports that hold it in place inside your pelvis.
This illustrates the importance of developing strong and healthy pelvic floor muscles with safe exercises if youve been diagnosed with a uterine prolapse or have had prolapse repair surgery.
Also Check: Can Endometriosis Cause Bladder Problems
Prolapse Surgery Success Rate
In some cases, some new bowel or bladder symptoms develop after prolapse surgery, which may require further treatment in the future, including further surgery. Some women develop incontinence after prolapse surgery and some have problems emptying their bladder and need to use a catheter afterwards. This problem usually gets better with time. There is a small risk of venous thrombosis with any pelvic surgery. To reduce this risk you will be given an injection every day and some anti-embolic stockings to wear.
What Clinical Studies For A Cystocele Are Looking For Participants
You can view a filtered list of clinical studies on cystoceles that are open and recruiting at www.ClinicalTrials.gov. You can expand or narrow the list to include clinical studies from industry, universities, and individuals however, the National Institutes of Health does not review these studies and cannot ensure they are safe. Always talk with your health care provider before you participate in a clinical study.
Don’t Miss: What Is Urinary Bladder Cancer
What Are Bladder Prolapse Symptoms
- Pain or discomfort in the pelvis
- Difficulty urinating
- A feeling that the bladder is not empty immediately after urinating
- Stress urinary incontinence – leakage caused by sneezing, coughing, and or physical exertion like running, jumping, or lifting weights.
- More frequent bladder infections
- Some women may not even experience or notice symptoms of a mild bladder prolapse.
How Is Vaginal Prolapse Treated
Vaginal prolapse treatment can vary depending on the severity of your prolapse. In some cases, your healthcare provider may want to just watch it over time to make sure it doesnt get worse.
There are nonsurgical and surgical treatment options for vaginal prolapses. There are a few things your healthcare provider will take into account when forming a treatment plan. These can include:
- Your general health and if you have any other serious medical conditions.
- The severity of your prolapse.
- If you want to have children in the future.
- If you want to have penetrative sex in the future.
Its important to have an open and honest conversation with your healthcare provider about these topics. Talk to your healthcare provider about any questions or concerns you have regarding these treatments.
Nonsurgical treatments are typically used as a first option and work best with minimal or mild prolapses. Specific treatment options can include:
For more severe cases, surgery to correct vaginal prolapse can be an option. These options include:
You May Like: Interstitial Cystitis Or Overactive Bladder
When Should You Have Surgery For Prolapse
Consider surgery if the prolapse is causing pain, if you are having problems with your bladder and bowels, or if the prolapse is making it hard for you to do activities you enjoy. An organ can prolapse again after surgery. Surgery in one part of your pelvis can make a prolapse in another part worse.
What Not To Do At The Gym
1. Drinking excessive amounts of water.
This crazy idea that the more water you drink the better is a load of clever marketing bunkum. There is no evidence that drinking more water that what our thirst dictates has any health benefits. In fact, excessive fluid intake can do the opposite it can put strain on the heart and, in extreme cases, lead to hyponatremia , risking seizures and even death.
Overfilling your bladder is not a good idea for the long term either if you regularly overfill it, the continual stretching of the balloon-like bladder muscle causes it to lose its elasticity, and eventually, its ability to empty properly. Thirst is the best guide as to how much you should drink.
2. Doing aerobic exercises when your pelvic floor muscles arent strong enough.
If you leak when you jog, skip or play sport, youre not alone. Studies consistently show about 30 percent of women have the same problem. But just because its common, doesnt mean its normal or OK.
Bladder leakage is due to the lax supports of your bladder and weak pelvic floor muscles. If they arent strong enough to withstand the pressures of high impact exercise, they need to be strengthened, just like any other muscles in the body.
You can get your pelvic floor muscles into better shape by doing pelvic floor exercises every day.
3. Doing resistance or core strength exercises that cause you to strain down.
4. Being constipated.
Dont Miss: Bcg Tx For Bladder Cancer
Also Check: Bcg Tx For Bladder Cancer
Tests For Bladder Prolapse
Tests that may be carried out to confirm or reject a diagnosis of bladder prolapse, depending on your symptoms, are:
- pelvic ultrasound to exclude any masses or cysts putting pressure on the bladder
- urodynamics a test of bladder function and to assess different types of incontinence
- a bladder scan to measure residual urine urine left in the bladder after emptying
- a midstream urine test to exclude urinary tract infection
- magnetic resonance imaging in some cases.
Lifestyle And Home Remedies
Kegel exercises are exercises you can do at home to strengthen your pelvic floor muscles. A strengthened pelvic floor provides better support for your pelvic organs and relief from symptoms associated with anterior prolapse.
To perform Kegel exercises, follow these steps:
- Tighten your pelvic floor muscles the muscles you use to stop urinating.
- Hold the contraction for five seconds, and then relax for five seconds.
- Work up to holding the contraction for 10 seconds at a time.
- Do three sets of 10 repetitions of the exercises each day.
Ask your doctor for instructions on how to properly perform a Kegel, and for feedback on whether you’re using the right muscles. Once you’ve learned the proper method, you can do Kegel exercises discreetly just about anytime, whether you’re sitting at your desk or relaxing on the couch.
To help keep an anterior prolapse from progressing, you can also try these lifestyle modifications:
- Treat and prevent constipation. High-fiber foods can help.
- Avoid heavy lifting, and lift correctly. When lifting, use your legs instead of your waist or back.
- Control coughing. Get treatment for a chronic cough or bronchitis, and don’t smoke.
- Manage your weight. Talk to your doctor to determine your ideal weight and get advice on weight-loss strategies, if you need them.
Recommended Reading: Can You Buy Bladder Infection Medicine Over The Counter
Pelvic Organ Prolapse Is Common
With regard to pelvic organ prolapse, Dr. Mahajan says its very common and often does not require treatment. About 40 percent of women ages 50 to 79 have some form of prolapse, according to the Womens Health Initiative.
The causes of pelvic organ prolapse are complex. Its often influenced by genetics, race, aging, pregnancy, smoking and obesity.
Some women may need surgery if prolapse blocks urination or causes discomfort. But if it doesnt bother you, we just watch it, Dr. Mahajan says.
Talk To Your Doctor If You Have Questions
If youre not sure what type of incontinence you have, its a good idea to talk to your doctor.
If they dont have the type of leakage that would be helped by bladder supports if they have urge leakage or overflow those patients wont benefit, says Dr. Vasavada. It might even make their symptoms worse.
If youre pretty sure you have urinary stress incontinence, however, its OK to try bladder supports.
If women are experiencing leakage with laughing, coughing, running, sneezing or lifting, and it seems like its pretty clear-cut, then trying an over-the-counter bladder support is completely appropriate, Dr. Ferrando says. They dont necessarily need to see their doctor first.
Recommended Reading: Bladder Leakage Pads For Women