Who Can Use Bcg
BCG is a treatment for early-stage bladder cancer that has not yet invaded the muscle of the bladder wall. Called non-muscle invasive bladder cancers or in situ bladder cancers, these account for about half of all bladder cancers.
For 2021, it was estimated that about 83,730 new cases of bladder cancer would be diagnosed in the United States, and about 17,200 American bladder cancer patients would die from the disease.
How Is Bladder Cancer Diagnosed
Bladder cancer is primarily diagnosed by identifying the tumor, imaging the tumors location, and lab tests. Patients will initially see a general practitioner, but the final diagnosis will be made by a urologist or oncologist .
Although bladder cancer is not diagnosed by the symptoms, its a good idea to know when its time to see a doctor. Symptoms of bladder cancer include blood in the urine or urinary obstruction. Other less common symptoms include painful urination, frequent urination, fatigue, and weight loss.
People should also be aware of symptoms if they are at risk of bladder cancer. At the top of the risk list is smoking, a habit that increases the likelihood of bladder cancer six-fold. Other bladder cancer risk factors include schistosomiasis infection , exposure to certain paint, dyes, or petroleum products, advanced age, and male gender.
The gold standard for bladder cancer diagnosis is identifying the tumor directly using cystoscopy. A physician inserts a narrow tube, called a cystoscope, through the urethra into the bladder to view the bladder lining. The physician will note what the tumor looks like and the number of tumors.
During the cystoscopy, a physician will remove a part of the tumor to be analyzed in the lab . A pathologist will study the tumor sample and look for tumor cells in a urine sample to make the definitive diagnosis.
Treating Stage Ii Bladder Cancer
These cancers have invaded the muscle layer of the bladder wall , but no farther. Transurethral resection is typically the first treatment for these cancers, but it’s done to help determine the extent of the cancer rather than to try to cure it.
When the cancer has invaded the muscle, radical cystectomy is the standard treatment. Lymph nodes near the bladder are often removed as well. If cancer is in only one part of the bladder, a partial cystectomy may be done instead. But this is possible in only a small number of patients.
Radical cystectomy may be the only treatment for people who are not well enough to get chemo. But most doctors prefer to give chemo before surgery because it’s been shown to help patients live longer than surgery alone. When chemo is given first, surgery is delayed. This is not a problem if the chemo shrinks the bladder cancer, but it might be harmful if the tumor continues to grow during chemo.
If cancer is found in nearby lymph nodes, radiation may be needed after surgery. Another option is chemo, but only if it wasn’t given before surgery.
For people who have had surgery, but the features of the tumor show it is at high risk of coming back, the immunotherapy drug, nivolumab, might be offered. When given after surgery, nivolumab is given for up to one year.
For patients who cant have surgery because of other serious health problems, TURBT, radiation, chemotherapy, or some combination of these may be options.
Read Also: What Causes An Overactive Bladder At Night
Treating Stage I Bladder Cancer
Stage I bladder cancers have grown into the connective tissue layer of the bladder wall , but have not reached the muscle layer.
Transurethral resection with fulguration is usually the first treatment for these cancers. But it’s done to help determine the extent of the cancer rather than to try to cure it. If no other treatment is given, many people will later get a new bladder cancer, which often will be more advanced. This is more likely to happen if the first cancer is high-grade .
Even if the cancer is found to be low grade , a second TURBT is often recommended several weeks later. If the doctor then feels that all of the cancer has been removed, intravesical BCG or intravesical chemo is usually given. If all of the cancer wasn’t removed, options are intravesical BCG or cystectomy .
If the cancer is high grade, if many tumors are present, or if the tumor is very large when it’s first found, radical cystectomy may be recommended.
For people who arent healthy enough for a cystectomy, radiation therapy might be an option, but the chances for cure are not as good.
Treating Stage 0 Bladder Cancer
Stage 0 bladder cancer includes non-invasive papillary carcinoma and flat non-invasive carcinoma . In either case, the cancer is only in the inner lining layer of the bladder. It has not invaded the bladder wall.
This early stage of bladder cancer is most often treated with transurethral resection with fulguration followed by intravesical therapy within 24 hours.
Recommended Reading: How To Do Bladder Training
Stage 0 Bladder Cancer
Stage 0 describes non-muscle-invasive bladder cancer. It is found only on the surface of the inner lining of the bladder. This stage is also known as in situ. Stage 0 bladder cancer is typically treated with transurethral resection , followed by either close follow-up without further treatment or intravesical therapy using bacillus Calmette-Guérin therapy to try to keep the cancer from coming back.
What To Expect During Bcg Treatment
First, make sure you havent had any fluids for four hours before the treatment. Right before you go into the treatment room your doctor or nurse will have you empty your bladder.
Youll lie on your back, and the medical professional will insert a catheter into your urethra and into your bladder, likely using some local numbing, and use this tube to infuse the treatment.
Once the treatment is infused, your doctor or nurse will remove the catheter. Theyll have you lie on your back, each side, and your stomach for 15 minutes each. The BCG mycobacteria needs to touch the bladder cancer cells to activate the immune system. Youll then be free to go but will need to hold off on peeing for another hour.
Verywell / Alex Dos Diaz
For at least six hours after your infusion, youll need to disinfect your pee to ensure none of the mycobacteria spread to anyone else. Pour an equal amount of bleach into the toilet after you pee and let it sit for 15 minutes before flushing.
Also, people with a penis who undergo BCG treatment should avoid sex for 48 hours to ensure they dont pass the mycobacteria to their partners.
You will likely need multiple BCG treatments. They may be given weekly for a few weeks, then less often for months or years to prevent cancer from coming back.
Don’t Miss: Why Do I Have A Bladder Infection
Understanding The Statistics: Cancer Survival
It is important to remember that all cancer survival numbers are based on averages across huge numbers of people. These numbers cannot predict what will happen in your individual case.
Survival rates will not tell you how long you will live after you have been diagnosed with bladder cancer. But, these numbers can give you an idea of how likely your treatment will be successful. Also, survival rates take into account your age at diagnosis but not whether you have other health conditions too.
New Treatments For Bladder Cancer In 2020
In 2019 and early 2020, the U.S. Food and Drug Administration approved a number of new drugs for bladder cancer of all stages, and more treatments are on the horizon. Heres a snapshot of whats happening right now in bladder cancer treatment:
Non-muscle invasive bladder cancer treatments
In patients with NMIBC, tumors are confined to the inner cell layer of the bladder and have not invaded the thick muscle tissue of the bladder. NMIBC is usually treated by surgical excision in a procedure known as trans urethral resection of bladder tumor , followed by repeated drug injections into the bladder most commonly with a drug called Bacillus Calmette-Guerin .
BCG is a bacterial vaccine that is primarily used to immunize against tuberculosis, but may also trigger a broader immune response against cancer cells. BCG certainly improves outcomes for patients whose tumors have been resected nevertheless, over a half of these patients will experience recurrence within one year, and some do not respond to BCG at all. Intravesical chemotherapy drugs are used for higher-grade NMIBC.
Newly emerging treatment options for NMIBC include:
Of course, the biggest news for NMIBC is the recent FDA approval of the immune checkpoint drug pembrolizumab for systemic treatment of high grade NMIBC that is not responsive to BCG. In clinical testing, 41% of patients experienced complete responses with median duration of 16 months.
Don’t Miss: How Can A Man Strengthen His Bladder
Treatment Options For Recurrent Bladder Cancer
Treatment options for patients with recurrent bladder cancer include the following:
Palliative radiation therapy should be considered for patients with symptomatic tumors.
Clinical trials
Recurrent or progressive disease in distant sites or after definitive local therapy has an extremely poor prognosis, and clinical trials should be considered whenever possible.
Other Treatments For Bladder Cancer
For many early-stage bladder cancers, BCG is the best option for treatment. Other treatments for bladder cancer include:
- Surgery to remove the tumor: Early cancers can be removed with TURBT surgery. More advanced cancers may require more extensive surgery, like removal of part or all of the bladder .
- Intravesical chemotherapy: This treats the inside of the bladder with chemotherapy drugs. Chemotherapy drugs commonly used for bladder cancer include Mutamycin , Gemzar , or Valstar .
- Radiation therapy
- Clinical trials
Read Also: Locally Advanced Bladder Cancer Stage
Stage Ii Bladder Cancer
Stage II cancer has invaded the muscle of the bladder wall but is still confined to the bladder. Depending on the extent and grade of the cancer, we may recommend a partial or total cystectomy. Some people may need chemotherapy before surgery. We may be able to remove the tumor with TUR followed by radiation and chemotherapy.
What Are The Common Side Effects Of Bladder Cancer Medication
Side effects of bladder cancer medications will vary depending on the medication, the dose, and the patients other medical conditions. This is not a complete list.
Almost two in three patients that receive intravesical BCG will experience bladder irritation that includes pain, swelling, painful urination, and a frequent need to urinate. BCG is a live culture of a bacteria similar to tuberculosis, so the next most common side effects are reactions to this bacteria as if it were an infection. The most serious side effect is an actual infection that will require antibiotic treatment.
Bladder cancer chemotherapy drugs all reduce the ability of bone marrow to produce white blood cells. As a result, infections are a common side effect and could be serious enough to require hospitalization.
Antitumor antibiotics commonly cause nausea, vomiting, and hair loss, as well as possible heart damage.
Common side effects of gemcitabine include flu-like symptoms, fatigue, nausea, skin rash, and a decrease in white blood cells, red blood cells, and platelets. Lowered red blood cells, or anemia, can cause fatigue, tiredness, and shortness of breath. Platelets are responsible for blood clotting, so patients on gemcitabine may have bleeding or bruising problems.
Common side effects of granulocyte-colony stimulating factors include bone pain, pain in the extremities, nausea, fever, and low platelet counts, which can cause bleeding and bruising problems.
Don’t Miss: Botox For Bladder Control Reviews
Bcg Relapse And Salvage Regimens
Guideline Statement 22
22. In an intermediate- or high-risk patient with persistent or recurrent disease or positive cytology following intravesical therapy, a clinician should consider performing prostatic urethral biopsy and an upper tract evaluation prior to administration of additional intravesical therapy.
Discussion
Urothelial carcinoma, particularly CIS, is considered a field-change disease with the entire urothelium at risk in affected individuals. Clinicians should remain aware of sites outside the bladder as potential sources for metachronous tumors. While the initial diagnostic evaluation includes radiographic/endoscopic visualization of the entire urinary tract, the extra-vesical urothelium remains at long-term risk for subsequent tumor development. Moreover, these sites may harbor disease and contribute to cancer recurrence within the bladder.
Of note, the Panel recognizes that evaluation of the upper urinary tract and urethra may be withheld in select patients who have received a single induction course of intravesical BCG and subsequently have persistent evidence of disease and are to undergo a second course of BCG.
Guideline Statement 23
23. In an intermediate- or high-risk patient with persistent or recurrent Ta or CIS disease after a single course of induction intravesical BCG, a clinician should offer a second course of BCG.
Discussion
Guideline Statement 24
Discussion
Guideline Statement 25
Discussion
Guideline Statement 26
Cystoscopy Is The Hallmark Of Surveillance
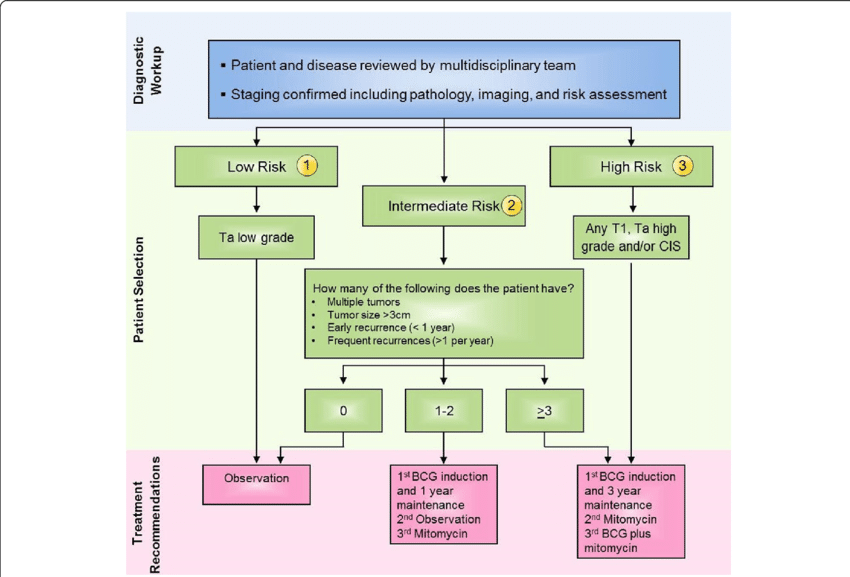
The EAU recommendations for follow up in patients after TUR of NMIBC are :
Patients with TaT1 tumours at low risk of recurrence and progression should have a cystoscopy at 3 months. If negative, the following cystoscopy is advised 9 months later, and then yearly for 5 years.
Patients with TaT1 tumours at high risk of progression and those with CIS should have a cystoscopy and urinary cytology at 3 months. If negative, the following cystoscopy and cytology should be repeated every 3 months for a period of 2 years, and every 6 months thereafter until 5 years, and then yearly. Yearly imaging of the upper tract is recommended.
Patients with TaT1 tumours at intermediate risk of progression should have an in-between follow-up scheme using cystoscopy and cytology, which is adapted according to personal and subjective factors.
During follow up in patients with positive cytology and no visible tumour in the bladder, R-biopsies or biopsies with PDD and investigation of extravesical locations are recommended.
A number of tumour markers have shown the ability to improve upon the sensitivity of cytology, but specificity is lower for most. Because of these facts, there are no markers that are accurate enough to replace cystoscopy or cytology in the follow up of NMIBC. Change in lifestyle habits can be advised and the most important are an increase in fluids, smoking cessation and a low-fat diet.
Also Check: Loss Of Bladder Control When Drinking Alcohol
Complications Of Transurethral Resection Of Bladder Tumours
Intraoperative complications
The major complications of uncontrolled haematuria and clinical bladder perforation occur in less than 5% of cases. Cauterization is used for the bleeding site. The vast majority of perforations are extraperitoneal, but intraperitoneal perforation is possible when resecting tumours at the dome . Management of extraperitoneal perforation is usually possible by prolonged urethral catheter drainage. Intraperitoneal perforation is less likely to close spontaneously and often requires open surgical repair. To prevent bladder perforation it is necessary to perform the resection if the bladder is not overdistended.
Postoperative complications
Minor bleeding and irritative symptoms are common side effects in the immediate postoperative period, but sometimes clot retention can occur, especially if an extensive resection was performed. When tumours are located at or near the ureteral orifice, obstruction of the upper tract can occur. Therefore, in these situations a postoperative ultrasound should be performed.
Living With Advanced Cancer
Advanced cancer usually means cancer that is unlikely to be cured. Some people can live for many months or years with advanced cancer. During this time palliative care services can help.
Most people continue to have treatment for advanced cancer as part of palliative care, as it helps manage the cancer and improve their day-to-day lives. Many people think that palliative care is for people who are dying but palliative care is for any stage of advanced cancer. There are doctors, nurses and other people who specialise in palliative care.
Treatment may include chemotherapy, radiation therapy or another type of treatment. It can help in these ways:
- slow down how fast the cancer is growing
- shrink the cancer
- help you to live more comfortably by managing symptoms, like pain.
Treatment depends on:
- how far it has spread
- your general health
Recommended Reading: Natural Remedies For Bladder Health
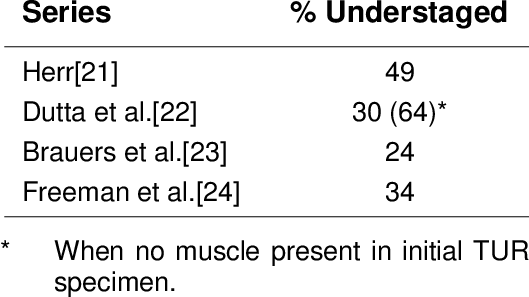
Transurethral Resection Of Bladder Tumours
Complete visualization to plan the resection is now facilitated by the initial flexible cystoscopy. In the past it was recommended that a 70° rod lens be used, which allowed maintenance of the anatomic relationships. Bipolar electroresection allows TUR in saline and minimizes the risk of the obturator reflex that can lead to bladder perforation . The use of general anaesthesia with muscle-paralyzing agents or anaesthetic block of the obturator nerve also prevents obturator reflex for tumours located at the lateral wall of the bladder. Resection of diverticular tumours presents a particular risk of bladder wall perforation and accurate staging is difficult to achieve because the underlying detrusor is absent. Invasion beyond the lamina propria immediately involves perivesical fat or stage T3a. Partial or radical cystectomy should therefore be considered for high-grade diverticular tumours.
Treatment Of Failure Following Intravesical Therapy
Patients with high-grade Ta, T1 or CIS are at high risk for recurrence and, more importantly, progression. Thus, both the American Urological Association and the EAU recommend initial intravesical treatment with BCG followed by maintenance therapy for a minimum of 1 year. The complete response rate to BCG therapy in patients with high-risk NMIBC can be as high as 80%. However, most patients with high-risk disease suffer from recurrence. Treatment with BCG is considered to have failed in the following situations:
When a muscle-invasive tumour is detected during follow up.
When a high-grade, nonmuscle invasive tumour is present at both 3- and 6-month follow up. In patients with a tumour present at 3 months, an additional BCG course can achieve a complete response in over 50% of cases, both in patients with papillary tumours and CIS , but with increasing risk of progression .
Any worsening of the disease under BCG treatment, such as a higher number of recurrences, higher T-stage or higher grade, or the appearance of CIS, in spite of an initial response.
In patients whose condition fails to respond to conservative treatment with noninvasive recurrences and who refuse surgical therapy or are not suitable candidates for surgery, the treatment options become even more complicated. Patients with nonmuscle invasive recurrence of urothelial bladder carcinoma after intravesical chemotherapy can benefit from BCG instillations .
Also Check: How Long Does It Take To Cure A Bladder Infection