Prolapse Surgery Success Rates
The success of prolapse surgery depends on many different factors, including:
- how bad your prolapse is,
- what parts of your pelvic floor is affected,
- what type of surgery you get, and
- lifestyle or genetic factors that could increase the risk of another prolapse in the future.
Studies show that about 80 percent of prolapse surgeries are still successful after 10 years. About 10 to 20 percent of women will have some movement or bulging again, but its usually not enough to need another surgery. Only about two to three percent of women will need a repeat prolapse surgery.
Surgical Options For Bladder Prolapse
Bladder Prolapse or cystocele is when the bladder falls down and often becomes visible. Urinary leakage often accompanies Bladder Prolapse or cystocele. This condition may cause pelvic pressure, difficulty emptying the bladder, a vaginal bulge that can be felt, and incontinence . Repair of Bladder Prolapse or Cystocele involves the surgical reduction of the bulge and placing the bladder back into its normal anatomic location. Medically this is called an Anterior Repair or Anterior Colporrhaphy.
The traditional repair for Bladder Prolapse is plicating or overlapping tissues with suture to reduce the bulge and support the bladder. Excess vaginal tissue is also usually trimmed at the time of surgery. Unfortunately this procedure has a very high failure rate ranging from 25 to 60 percent. Many patients and doctors find this high failure rate unacceptable and successfully repairing Bladder Prolapse or Cystocele is certainly one of the more challenging surgeries gynecologists and urogynecologists perform.
More modern surgical techniques treats Bladder Prolapse or cystoceles as a hernia of the bladder into the vagina, hence, the use of mesh or donor tissues as a patch or graft to improve success rates. The placement of these materials in a safe and effective manner is highly dependent on the surgeons skill and experience. Having used these method extensively over the past number of years, my experience has been a success rates of about 90% in my hands.
What Is The Recovery Time For Pelvic Reconstructive Surgery How Painful Is Prolapse Surgery What Happens If Prolapse Is Left Untreated
- >
- What is the recovery time for pelvic reconstructive surgery? How painful is prolapse surgery? What happens if prolapse is left untreated?
Pelvic floor dysfunction symptoms typically stay or become worse if theyâre not treated. Instead of living with pain and discomfort, you can often improve your everyday life after a visit with your provider. The most common type of pelvic reconstructive surgery is that performed to correct pelvic organ prolapse.
Types of prolapse:
- Cystocele: Bladder falls into the vagina
- Enterocele: Small bowel falls into the vagina
- Rectocele: Rectum falls into the vagina
- Uterine Prolapse: Uterus falls into the vagina
- Vaginal Vault Prolapse: Upper portion of the vagina descends into the vaginal canal
There are two main types of prolapse surgery:
- Transvaginal performed through the vagina.
- Transabdominal performed through the abdomen, usually laparoscopic or robotic via small incisions.
Both approaches are considered minimally invasive, have good success rates, and the approach is dependent on the preference of the patient as well as the surgeon. It should be a joint decision.
Avoid constipation by increasing the fiber content in your diet, avoid taking pain medications as much as you can, and use stool softeners. Straining during bowel movements can place undue pressure on your reconstructive surgery before complete healing.
Don’t Miss: Homeopathic Medicine For Bladder Weakness
Addition Information About Vaginal Surgery When A Synthetic Or Biologic Graft Is Used
In Australia, in January 2018 the TGA withdrew approval for the used of synthetic and biologic mesh for trans-vaginal prolapse repair. The TGA continues to approve synthetic and biological mesh for prolapse when placed using laparoscopy, robot assisted and through an abdominal incision.
In the USA, the Food and Drug Administration has issued the following safety communication regarding the use of mesh.
The FDA wants to inform you about the complications that can occur when surgical mesh is used to treat Pelvic Organ Prolapse and Stress Urinary Incontinence , and provide you with questions to ask your surgeon before having these procedures. This is part of our commitment to keep healthcare professionals and the public informed about the medical products we regulate.
FDA has received reports of complications associated with the placement of mesh through an incision made in the wall of the vagina. Although rare, these complications can have serious consequences. The reports have not been linked to a single brand or model of mesh.
The most frequent complications included erosion through the vagina, infection, pain, urinary problems and recurrence of the prolapse and/or incontinence.
Background
Pelvic organ prolapse can cause pain or problems with bowel and bladder functions or interfere with sexual activity.
Stress urinary incontinence is a type of incontinence caused by leakage of urine during moments of physical stress.
Talking to your doctor
What Is A Vaginal Mesh Suspension
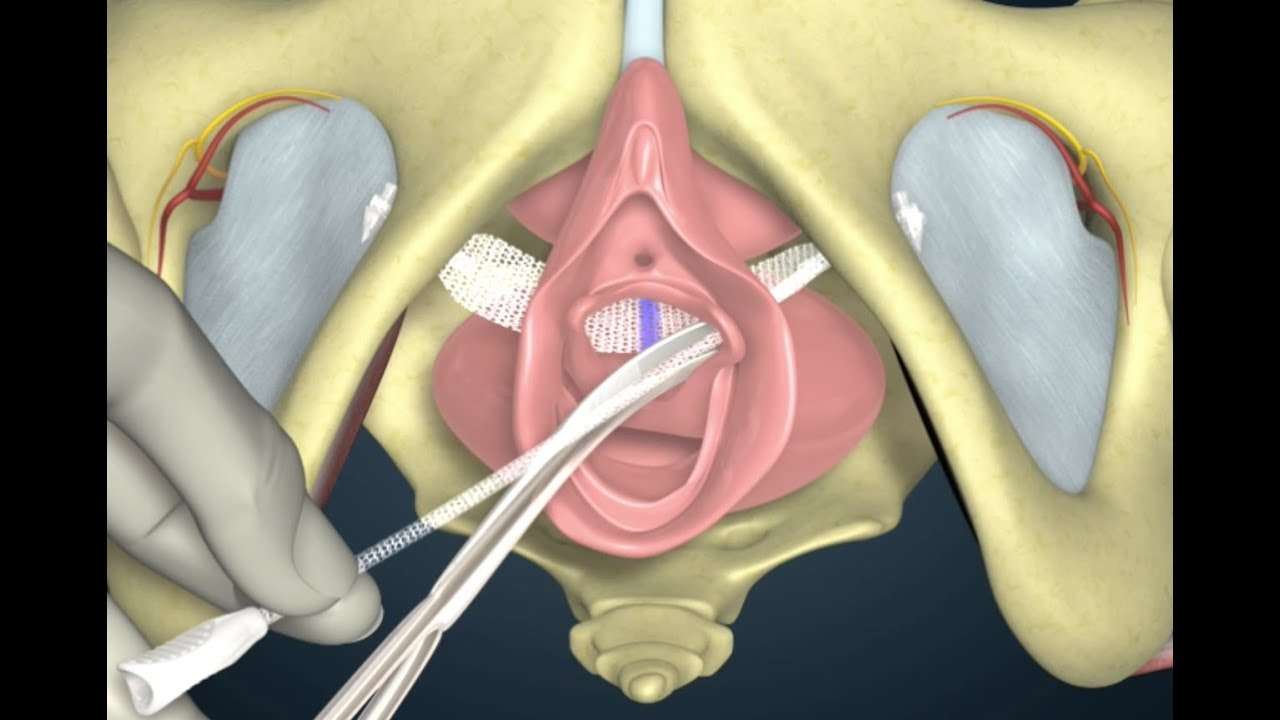
In some women, the supporting ligaments of the vagina are so weakened or torn that they are beyond repair. For these women, an artificial material can be used to take the place of the weakened ligaments. There are a number of types of materials used to perform this operation, but the most common is a thin, plastic, non-reactive mesh. This mesh is flexible, much like cloth, and can be cut and tailored to fit each woman’s anatomy. The mesh is first sutured onto the top of the vagina as it sits inside the body. The vagina is pulled up to its normal position, and the other end of the mesh is sutured to the connective tissue around the sacral bone to hold the vagina in place. The mesh is very strong, and the operation has a high success rate. However, in rare cases, the body can have a reaction to the mesh since it is foreign material. For that reason, the procedure is reserved for women who have had a previous failed vaginal prolapse surgery and need repeat surgery.
This mesh operation is called a sacral colpopexy and is most often performed through an abdominal incision. However, recent innovations now allow this procedure to be performed laparoscopically by experienced laparoscopic surgeons. In some centers the addition of the Da Vinci Robot has assited with laparoscopic support surgery. As with other laparoscopic procedures, the hospital stay is shorter and the recovery faster.
Also Check: Loss Of Bladder Control In Cancer Patients
Study: Common Surgery For Prolapse Fails Nearly 1 Out Of 3 Women
We’ve written a lot about the scary complications associated with vaginal mesh, synthetic devices that are surgically implanted to treat women suffering from prolapse. This condition, which afflicts millions of women after childbirth or as they age, occurs when stretched or weakened pelvic-area tissues give way, allowing the bladder or other organs to sag or bulge into the vagina.
Now, adding to the mounting data on the potential risks of prolapse surgery in general, a new study in the Journal of the American Medical Association finds that a common surgical treatment for prolapse one considered the “gold standard” involving abdominal surgery fails nearly 1 out of 3 women.
So why does prolapse surgery matter? As the JAMA study authors note, nearly 1 in 4 woman have at least one pelvic floor condition and “more than 225,000 surgeries are performed annually in the United States for pelvic organ prolapse.” So, any woman considering this surgery should be aware of the “long-term risks of mesh or suture erosion.”
USA Today reports on the latest findings:
She says she cant comment on the prolapse study with respect to specific surgical technique and procedure, but she still has these thoughts to share:
This program aired on May 23, 2013. The audio for this program is not available.
Pain After Prolapse Surgery
You will experience cramping or pressure in your pelvic area after your surgery. Most people experience this pain for about two weeks, but it may last up to six weeks. If you have an abdominal incision, you may have pain around the incision as it heals. Some people take prescription and/or over-the-counter pain medication to help manage their pain.
Also Check: Can A Kidney Or Bladder Infection Cause Back Pain
What Can Be Done If The Rectum Is Bulging
Repair of a bulging rectum is also a common operation. Childbirth sometimes can injure the supporting tissues of the rectum. Weakened or torn tissue will not hold the rectum down in its proper place, and the rectum bulges up inside the vagina. Surgery can repair these weakened or torn connective tissues. The repair follows a similar design as the bladder repair. The wall between the vagina and the rectum is opened, and the doctor can actually see and feel the tears just as you can feel a tear in a piece of cloth. Each tear is sutured and closed individually, in a procedure called a site-specific rectocele repair. Once the tears have been fixed, the connecting tissue should be strong enough to keep the rectum in its proper place.
What Causes Pelvic Organ Prolapse
There are many factors that are thought to cause a prolapse. In most cases, anything that may apply or put increased pressure in the abdomen can lead to a pelvic organ prolapse. Some of the common causes may include:
- Pregnancy, labor, and childbirth are the most common causes
- Obesity
- Respiratory problems with a chronic, long-term cough
- Constipation
- Surgical removal of the uterus
- Diastasis recti
Are you looking for safe and restorative exercises to heal from pelvic floor symptoms
Learn more about the RYC program
Are you looking for safe and restorative exercises to heal from pelvic floor symptoms
Learn more about the RYC program
Read Also: What Can Cause An Overactive Bladder
Degree Of Bother By Symptoms Is A Key Factor
In older patients, whether and how to treat POP depends on their functional status, the degree to which they are bothered or inconvenienced by the condition, and their personal preference.
If an elderly woman has anatomic POP but lacks bothersome symptoms, the condition rarely requires treatment. Conversely, POP symptoms may cause depression and poor self-image and impair participation in social activities. Associated bladder, bowel or sexual symptoms can also take their toll. And quality of life may be impacted regardless of the stage of prolapse. Vaginal bulge causing discomfort and/or bleeding, difficulty voiding and/or defecating, recurrent urinary tract infections and POP-associated low back pain are all symptoms that may warrant treatment.
Laparoscopic/robotic Sacrocolpopexy Vs Open Sacrocolpopexy
Although open sacrocolpopexy is a good treatment option for apical prolapse repair, with long-term success rates of 78% to 100%, it is associated with increased length of hospital stay, analgesic requirements, and cost compared with transvaginal procedures . New surgical techniques such as LSC or RSC have been developed to overcome these limitations. Compared with open sacrocolpopexy, LSC or RSC decreases overall morbidity and has good anatomical durability . Freeman et al. performed a randomized study comparing open sacrocolpopexy and LSC in patients with vault prolapse, and found that the methods demonstrated clinical similar recurrence rates at 1 year. In 2016, Costantini et al. conducted the longest randomized follow-up study comparing open sacrocolpopexy and LSC, and found that both techniques are efficacious with no patients in their sample experiencing apical recurrences. The 2016 Cochrane review reported that there may be no difference between the results of LSC and open sacrocolpopexy for repeat surgery for prolapse .
Read Also: Back Pain And Bladder Leakage
Free Pelvic Floor Educational Series
Dr. Sarah Duvall, PT, DPT, CPT and the CES Team have helped thousands of women create the strength and stability needed to overcome common and not-so-common pelvic floor issues.
Join us today for this 4-part Pelvic Floor Video Series, absolutely free.
We don’t spam or give your information to any third parties. View our Terms of Use and Privacy Policy.
Pros Of Bladder Suspension Surgery

1. Less Urine LeakageWhen the procedure is effective, urine leakage is not only reduced but almost nonexistent. This means that you can return to your normal activities and not have to be self-conscious when you are on-the-go. Urine leakage can impact your emotional and mental state negatively, but bladder suspension surgery can help you get your life back.
2. Treats All Types of Stress IncontinenceNo matter what your cause of stress incontinence is, this can be an effective surgical procedure. Those people dealing with urine leakage caused by menopause, child birth, surgery or muscle problems are great candidates for this type of surgery. It is almost 90% effective, which makes it the superior treatment option to Kegal exercises or medication.
Also Check: Can Stress Cause Overactive Bladder
The Pelvic Pro Support Belt For Prolapse Treatment
If you wish to opt out of surgery and would prefer a more natural prolapse treatment option, women from all over the world are finding relief with our Pelvic Pro prolapse support belt. This is a comfortable brace that can be worn under your clothes and stay hidden from anyone noticing. Give our pelvic belt a try before choosing surgery and join other women in finding relief today!
What To Do If You Have Been Diagnosed With Prolapse
If you have been diagnosed with or think you may have a prolapse, you can find out about the different types of treatments that may be offered to you here, as well as ways of helping yourself. This information should be used in conjunction with support from your GP or health professional to help you find the right course of treatment best suited to your individual needs enabling you to manage your condition and improve your quality of life.
Please use this information carefully and always speak to your GP or health professional, they can explain what is causing your problem and how the different treatments may help you. They will also talk to you about any side effects, these are extra problems that can be caused by the treatment.
Together, you can decide which treatment is the most suitable.
You May Like: Uti Bladder Infection Kidney Infection
What Is A Pelvic Floor Disorder
The “pelvic floor” is a group of muscles that form a kind of hammock across your pelvic opening. Normally, these muscles and the tissues surrounding them keep the pelvic organs in place. These organs include your bladder, uterus, vagina, small bowel, and rectum.
Sometimes, these muscles and tissues develop problems. Some women develop pelvic floor disorders following childbirth. And as women age, pelvic organ prolapse and other pelvic floor disorders become more common.
When pelvic floor disorders develop, one or more of the pelvic organs may stop working properly. Conditions associated with pelvic floor disorders include:
- Pelvic organ prolapse
- Anal incontinence
What Can Be Done If The Uterus Is Coming Down
Many gynecologists feel the best way to treat a falling uterus is to remove it, with a surgery called a hysterectomy, and then attach the apex of the vagina to healthy portions of the ligaments up inside the body. Other gynecologists, on the other hand, feel that hysterectomy is a major operation and should only be done if there is a condition of the uterus that requires it. Along those lines, there has been some debate among gynecologists regarding the need for hysterectomy to treat uterine prolapse.
This same uterine preserving procedure may also be accomplished though the vagina making a small entry into the abdomen behind the cervix and reattaching the ligaments to the uterus and cervix. This would be called a vaginal-uterosacral hysteropexy and leaves no abdominal scars.
You May Like: Overactive Bladder And Back Pain
Possible Prolapse Surgery Complications & Risks
Minor symptoms should subside a few weeks after the operation. If they persist, talk to your doctor to clarify what is needed.
Complications can vary from general to specific symptoms including:
- Pain and discomfort during sex
- Bladder problems
- Pelvic pain during and after recovery
- Infection of the surgical site
- Recurrence of pelvic prolapse
- Other serious problems such as:
What about Kegels and Pessaries, you ask? Actually, we have mixed feelings about these methods. Both can provide temporary relief yet they dont solve the root cause of prolapse. Kegels are not suitable for women with tight pelvic floors while pessaries are invasive devices with their own drawbacks!
What Exams And Tests Diagnose A Prolapsed Bladder
An exam of the female genitalia and pelvis is usually required in diagnosing a prolapsed bladder. Seeing the bladder bulging into the vagina on examination is diagnostic. In addition, you will be asked to strain/cough/bear down to determine the extent of the bladder prolapse, as well as determine if you have urinary leakage with increased pressure .
For less obvious cases, the doctor may use a voiding cystourethrogram to help with the diagnosis. During the voiding cystourethrogram, a catheter is placed into the bladder through the urethra. The bladder is emptied and then a sterile contrast is passed through the catheter into the bladder until the bladder is full enough to void. A series of X-ray films then are taken during bladder filling and during urination. These X-ray films help the doctor determine the shape of the bladder and the cause of urinary difficulty. The doctor may also test or take X-ray films of different parts in the abdomen to rule out other possible causes of discomfort or urinary difficulty.
After diagnosis, the doctor may test the nerves, muscles, and the intensity of the urine stream to help decide what type of treatment is appropriate.
A test called urodynamics or video urodynamics may be performed at the doctorâs discretion. Urodynamics measures pressure and volume relationships in the bladder and can also assess the function of the urethra and may be crucial in the decision-making of the urologist/urogynecologist.
Read Also: How To Treat A Leaky Bladder