Grade And Risk Category
The biopsy results will show the grade of the cancer. This is a score that describes how quickly a cancer might grow. Knowing the grade helps your urologist predict how likely the cancer is to come back and if you will need further treatment after surgery.
| Low grade | The cancer cells look similar to normal bladder cells, are usually slow-growing and are less likely to invade and spread. Most bladder tumours are low grade. |
| High grade | The cancer cells look very abnormal and grow quickly. They are more likely to spread both into the bladder muscle and outside the bladder.
In non-muscle-invasive tumours, the grade may be low or high, while almost all muscle-invasive cancers are high grade. Carcinoma in situ is a high-grade tumour that needs prompt treatment to prevent it invading the muscle layer. |
| Risk category | Based on the stage, grade and other features, a non-muscle-invasive bladder cancer will also be classified as having a low, medium or high risk of returning after treatment. This will help your doctors work out which treatments to recommend. |
Risk Stratification Based On Molecular Biomarkers
For molecular biomarkers to be of clinical use, they should be able to increase the predictive accuracy beyond the standard clinical and pathological parameter models. Several investigators have attempted to use molecular biomarkers as prognostic factors to predict outcomes in patients with NMIBC. However, molecular biomarkers have shown mixed results so far and are not sufficiently validated to be used in clinical practice at this time.
It is becoming clear that superficial low-grade cancers and invasive or high-grade cancers harbor distinctive genetic defects: The low-grade, non-invasive papillary tumors are characterized by activating mutations in the H-Ras gene and fibroblast growth factor receptor 3 gene and the high-grade invasive tumors are characterized by structural and functional defects in the p53 and retinoblastoma protein tumor-suppressor pathways. The deletion of both arms of chromosome 9 occurs frequently in bladder cancer during the earliest stages of tumorigenesis. However, these chromosomal aberrations do not seem to distinguish between the two tumor development pathways. Tumor invasion and progression in the bladder seems to be a multifactorial process, promoted by micro-environmental changes that include the up-regulation of N-cadherin, the down-regulation of E-cadherin, the overexpression of matrix metalloproteinases 2 and 9, an imbalance between angiogenic and anti-angiogenic factors and increased synthesis of prostaglandin.
What Impacts The Bladder Cancer Survival Rate
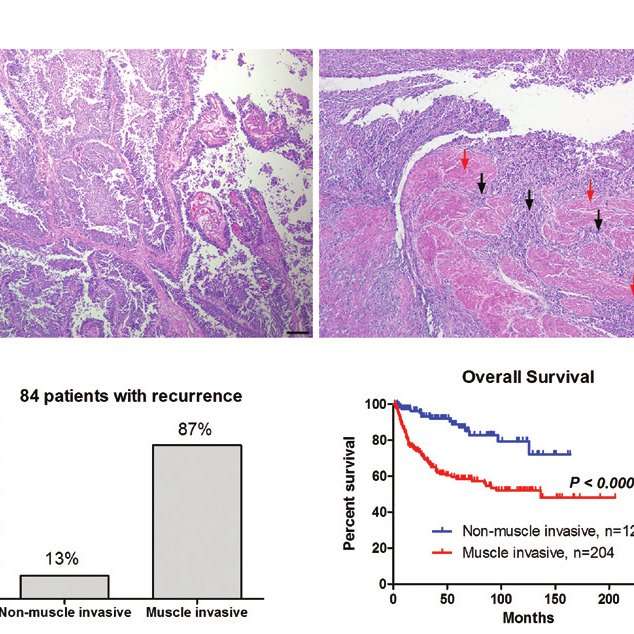
Survival rates depend on many factors, including the type and stage of bladder cancer that is diagnosed. According to the ACS, the five-year survival rate of people with bladder cancer that has not spread beyond the inner layer of the bladder wall is 96%. This is called non-muscle invasive bladder cancer . More than half of people are diagnosed at this stage.
If a tumor is invasive but has not yet spread outside the bladder, the five-year survival rate is 69%. Approximately 33% of bladders cancers are diagnosed at this stage. If the cancer extends through the bladder to the surrounding tissue or has spread to nearby lymph nodes or organs, the five-year survival rate is 37%. If the cancer has spread to distant parts of the body, the five-year survival rate is 6%. About 4% of people are diagnosed at this stage.
It is important to remember that statistics about the five-year survival rates for people with bladder cancer are estimates only and come from annual data based on the number of people with this cancer. A number of new and promising bladder cancer treatments that have been approved by the Food and Drug Administration in the last five years might not be reflected in a five-year survival rate statistic.
Just like no single treatment is appropriate for all bladder cancer patients, there is not one statistic that applies to everyone either. Talk with your doctor about your own individual situation to gain the best understanding you can.
Recommended Reading: Air Bladder To Open Car Door
Perspectives Of Bladder Microbiome And Urobiome: A New Opportunity For A Predictive Response
NGS technologies enable the study of the microbiome . Microbial dysbiosis impacts several human diseases including bladder carcinogenesis . However, the mechanistic links between microbiome signatures and bladder pathogenesis are still unknown. Urobiome studies may open the way to understand how bladder microbiota affects immunotherapy response leading to BCG-unresponsive patients .
Urinary microbiome through the 16S ribosomal RNA sequencing and expanded quantitative urine culture enable unculturable and/or rare microbes detection . The core step in microbiome analysis is the taxonomic classification of the representative sequences and clustering of operational taxonomic units . To assess the association between microbiome signatures and clinical phenotype, useful bioinformatic tools are PERMANOVA-S and MiRKAT . Bladder microbiome analysis showed that the most abundant genera are Lactobacillus , followed by Corynebacterium , Streptococcus , Actinomyces , and Staphylococcus . Innovative drug strategies based on precise antimicrobial peptides might boost the host immune system to ensure bladder microbiome homeostasis . Novel urinary biomarkers proved to be endowed with prognostic and diagnostic value in urological malignancies derived from exosomes, such as H2B1K and alpha-1 antitrypsin .
Data Collection And Quality Assessments
Study selection was carried out in a standardized, unblinded manner by one reviewer. Abstracts and titles were read, and if considered relevant then full papers were obtained and reviewed. After the initial screen, 23 articles were selected and their methodology reviewed. Retrospective studies were checked for using the same patient data, and the data were unique in each case.
For selected studies, the relevant outcome data were collected using a data-extraction spreadsheet in Microsoft Excel 2010. All data collected were verified for comparability and compared with the data in the publication. For each study, the time period, methodological design, duration of follow-up, number of patients, proportion of Ta/T1, proportion of concomitant CIS, CSS rate, lymph node involvement at pathological staging, pathological upstaging proportion, progression rate and associated p value were extracted. An assessment of the risk of bias for each study is given in Table 1.
Table 1
An assessment of the risk of bias for each study using a standard approach with defined criteria modified from Viswanathan et al.
Recommended Reading: Symptoms Of Bladder Stones In Cats
Muscle Invasive Bladder Cancer
24 February 2012
Patients with muscle invasive bladder cancer have at best 50% overall survival depending upon their pathological stage and lymph node status. However, despite the progress made with the use of cisplatin-based combination chemotherapy in metastatic disease, chemotherapy is seldom used for infiltrating bladder cancer in the pre and post-cystectomy settings.
Clinical trials have been fraught with difficulties. There is currently more evidence available from randomised clinical trials in favor of upfront, neoadjuvant chemotherapy. In the adjuvant post-operative setting, many clinical trials have been closed early due to poor accrual. Due to the methodological issues in many of the studies in the peri-operative setting, the only conclusions that can be drawn are from meta-analyses combining the results of randomised trials.
Neo-adjuvant chemotherapy trials in bladder cancerResults of a recently published EORTC-MRC neoadjuvant randomized clinical trial will be highlighted. Prior meta-analysis of Phase III randomised trials with cisplatin-based combination chemotherapy has suggested a 5% benefit for cisplatin-based chemotherapy in the neo-adjuvant setting.
Adjuvant chemotherapy trials
Most recently, a large cohort analysis assessing the effect of adjuvant chemotherapy from several large centers suggested the greatest impact of adjuvant chemotherapy is seen in patients with extravesical extension or N+ disease.
Challenges
Saturday, 25 February
Category:
Risk Groups For Early Bladder Cancer
Doctors classify bladder cancer that has not grown into the muscle layer of the bladder wall into risk groups. These risk groups are based on several factors, including the size and grade of the cancer. The risk groups allow the doctor to estimate the chance that the cancer will come back and continue to grow and spread . Doctors also use the risk groups to help plan the best treatment.
Any non-invasive and non-muscle-invasive bladder cancers are classified as low, intermediate or high risk.
Recommended Reading: How Do They Diagnose Bladder Cancer
Monotherapy Combination Therapy And Multi
Combination therapies based on immunomodulators such as checkpoint inhibitors have shown a synergistic effect to augment the immune response .
A discrete amount of studies are based on combination therapy with chemotherapeutic drugs, intravesical BCG, and immune checkpoint inhibitors, as some trials reported in Table 1 . Currently, an FDA-approved combination therapy is based on intravesical gemcitabine and cisplatin for NMIBCs .
As shown in Table 2, several clinical trials are designed to investigate combination therapies based on BCG immunotherapy and different chemical or biological compounds or vaccines . Combination therapies encompass also combination chemotherapies especially in recurrent and advanced BC including . Furthermore, photodynamic immunotherapy emerged recently to stimulate the immune response in NMIBC BCG-refractory or intolerant to BCG treatment as well .
One frontier of medicinal chemistry is polypharmacology . Benedetti et al. reviewed the immuno-oncological dynamic interactions to design multi-target modulators.
Stage 3 Bladder Cancer
Stage 3 bladder cancer means that the cancer cells have spread beyond the bladder muscle.1,2,3 Stage 3 bladder cancer includes the following combined TNM stages:
In all three types of stage 3 bladder cancer, the cancer cells have not spread to the lymph nodes near the bladder and they have not spread to other parts of the body.
In a bladder tumor that is stage T3a or stage T3b, the bladder cancer cells have grown into the layer of fatty tissue that surrounds the outside of the bladder. This layer of fatty tissue is called perivesical tissue.
In a stage T3a bladder tumor, the bladder cancer cells in the perivesical tissue are only visible through a microscope. In a stage T3b bladder tumor, the bladder cancer cells have grown into the perivesical tissue and are large enough that they are visible using an imaging test or they can be felt by a healthcare professional. A stage T4a bladder tumor is different in women and men. In women, the stage T4a tumor has grown through the perivesical tissue and into the uterus and/or vagina. In men, the stage T4a tumor has grown through the perivesical tissue and into the prostate. However, in both women and men, a stage T4a tumor has not grown into the pelvic wall or the abdominal wall.
Don’t Miss: Can A Bladder Infection Cause Dizziness
Biomarker May Help Predict Survival In Patients With Bladder Cancer
Long-term survival data from the first prospective, randomized biomarker validation trial in patients with muscle-invasive bladder cancer being treated with cisplatin-based chemotherapy before surgery will be reported at the 2022 Genitourinary Cancers Symposium of the American Society of Clinical Oncology on February 18, 2022.
The results are from the S1314 clinical trial conducted by the SWOG Cancer Research Network, a cancerclinical trials group funded by the National Cancer Institute , part of the National Institutes of Health .
Primary results of the S1314 study were published in the journal Clinical Cancer Research in 2021 and reported an association between a gene-expression biomarker called the COXEN GC score and a tumor’s pathologic response to chemotherapy. The new findings being presented at GU ASCO are results of a prespecified secondary analysis of S1314 data that looked for associations between COXEN score and how long a patient lived after starting treatment , and between COXEN score and how long a patient lived without their disease getting worse .
The work was led by Thomas W. Flaig, MD, a SWOG investigator at the University of Colorado Cancer Center and vice chancellor for research at the University of Colorado Anschutz Medical Center. “The work on S1314 was a tremendous collaborative effort across many institutions,” Flaig said, “and it provides important information on patients being treated with preoperative chemotherapy for bladder cancer.”
Baseline Characteristics Of The Patients
Table shows the basic characteristics of the 100 patients involved in the study. The median follow-up time was 77.4 months. The mean age of the patients was 65.1±11.2years, and more than 80% of the patients were males. Ninety-one patients had an ASA physical status below 3. All patients were diagnosed as having muscle-invasive bladder cancer with T2-4N0-3M0 10% of the patients underwent neoadjuvant chemotherapy, 35% of the patients underwent radical cystectomy with standard pelvic lymph node dissection , whereas 65% of the patients had extended PLND. Moreover, 65% of the patients underwent ileal conduit urinary diversion, and the remaining 35% underwent neobladder diversion.
Table 1 Basic patient characteristics
You May Like: How To Use A Drain Cleaning Bladder
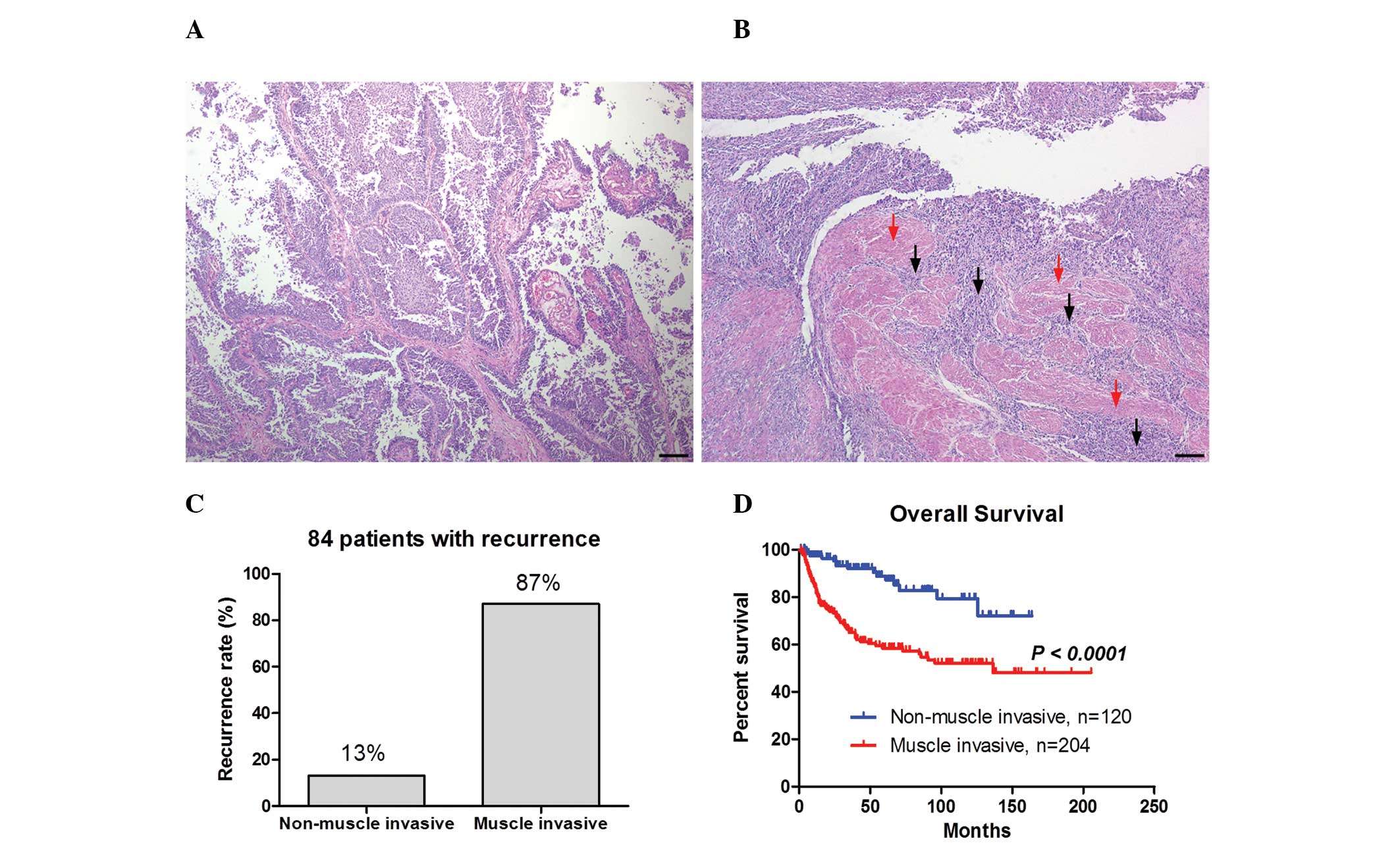
What Is Muscle Invasive Bladder Cancer
Muscle invasive bladder cancer is a cancer that spreads into the detrusor muscle of the bladder. The detrusor muscle is the thick muscle deep in the bladder wall. This cancer is more likely to spread to other parts of the body.
In the U.S., bladder cancer is the third most common cancer in men. Each year, there are more than 83,000 new cases diagnosed in men and women. About 25% of bladder cancers are MIBC. Bladder cancer is more common as a person grows older. It is found most often in the age group of 75-84. Caucasians are more likely to get bladder cancer than any other ethnicity. But there are more African-Americans who do not survive the disease.
What is Cancer?
Cancer is when your body cells grow out of control. When this happens, the body cannot work the way it should. Most cancers form a lump called a tumor or a growth. Some cancers grow and spread fast. Others grow more slowly. Not all lumps are cancers. Cancerous lumps are sometimes called malignant tumors.
What is Bladder Cancer?
When cells of the bladder grow abnormally, they can become bladder cancer. A person with bladder cancer will have one or more tumors in his/her bladder.
How Does Bladder Cancer Develop and Spread?
The bladder wall has many layers, made up of different types of cells. Most bladder cancers start in the urothelium or transitional epithelium. This is the inside lining of the bladder. Transitional cell carcinoma is cancer that forms in the cells of the urothelium.
Survival For All Stages Of Bladder Cancer
Generally, for people diagnosed with bladder cancer in England:
- around 75 out of every 100 survive their cancer for 1 year or more after diagnosis
- almost 55 out of every 100 survive their cancer for 5 years or more after they are diagnosed
- around 45 out of every 100 survive their cancer for 10 years or more after diagnosis
Cancer survival by stage at diagnosis for England, 2019Office for National Statistics
These statistics are for net survival. Net survival estimates the number of people who survive their cancer rather than calculating the number of people diagnosed with cancer who are still alive. In other words, it is the survival of cancer patients after taking into account that some people would have died from other causes if they had not had cancer.
Also Check: Reasons For Frequent Bladder Infections
Predictors Of Good Response
MIBC constitutes a heterogeneous group of tumors. Thus selection criteria are required to determine the ideal candidates for receiving TMT. It would be relevant to identify the subgroup of MIBC types that would not respond to TMT, as the 5-year CSS rate was lower in nonresponders compared to the responders .
Historical series of RT alone have suggested that flat lesions such as CIS, incomplete resection, locally advanced stage disease , and the presence of ureteral obstruction were associated with poorer response to RT . The impact of several pretreatment variables on oncological outcomes has been assessed .
Hydronephrosis has also been suggested as a poor prognostic factor and several studies used it as part of the study exclusion criteria . In fact, the RTOG protocols after 1993 have excluded patients with tumor-related hydronephrosis. Hydronephrosis that occurred in about 10%35% of eligible patients was significantly linked to poorer outcomes, specifically in terms of response rates. The response rate was improved by at least 1.5-fold in the absence of ureteral obstruction .
Although multiplicity has been identified as a predictive factor for relapse in two studies , no significant association was found between multiplicity and CR rate or survival. However, studies did not include patients with diffuse multifocal disease, and TMT is not advocated in this subgroup of patients.
David I. Lee MD, in, 2007
Relationship Between Basal Type And Prognosis
In the case of CK5/6+ and GATA3- samples, more than 1% CK5/6 expression and GATA3- expression was significantly negatively correlated with OS . In the case of CK5/6+ and FOXA1- samples, more than 1% CK5/6+ expression and FOXA1 expression was significantly negatively correlated with OS and CSS . In the case of CK14+ and GATA3-samples and CK14+ and FOXA1- samples were not significantly correlated with OS, CSS and RFS.
Fig. 4
Oncologic outcomes according to ck5/6 and gata3 and ck5/6 and foxa1 in immunochemical staining. a Overall survival, b Cancer specific survival, c Recurrence free survival
Read Also: Cranberry Juice Cure Bladder Infection
An Unmet Medical Need In Mibc
MIBC is frequently undertreated in the United States. An evaluation of the National Cancer Database included over 28,000 patients with localized T2T4a MIBC initiating treatment between 2004 and 2008 and revealed that nearly half did not receive aggressive therapy . Aggressive therapy was defined as potentially curative therapy in the form of radical or partial cystectomy, or definitive radiation therapy with or without chemotherapy, to a total dose 50 Gy. In this analysis, 52.5% of patients received aggressive therapy, including 44.9% having surgery and 7.6% having radiation therapy. One-fourth of patients had observation only. Multivariate analyses indicated that patient factors associated with nonreceipt of aggressive therapy included advanced age, lower socioeconomic status, black race, lack of access to high-volume centers, higher Charlson comorbidity score, and the presence of hydronephrosis or hydroureter. Treatment with observation occurred in over 25% of patients aged 7079 years and nearly 40% of patients aged 8089 years.
Access to health care and management of MIBC in patients who are considered unfit due to age or comorbid conditions represents clear unmet medical needs. With broader uptake of selective bladder preservation, TMT could bridge this important gap in the care of MIBC patients.
Yun-Sok Ha, Tae-Hwan Kim, in, 2018