Bladder Cancer Clinical Trials
What about Clinical Trials?
You may hear about clinical trials for your bladder cancer. Clinical trials are research studies that test if a new treatment or procedure is safe and effective.
Through clinical trials, doctors find new ways to improve treatments and the quality of life for people with disease. Trials are available for all stages of cancer. The results of a clinical trial can make a major difference to patients and their families. Please visit our clinical trials research webpage to learn more.
Treating Bladder Cancer That Progresses Or Recurs
If cancer continues to grow during treatment or comes back after treatment , treatment options will depend on where and how much the cancer has spread, what treatments have already been used, and the patient’s overall health and desire for more treatment. Its important to understand the goal of any further treatment if its to try to cure the cancer, to slow its growth, or to help relieve symptoms as well as the likely benefits and risks.
For instance, non-invasive bladder cancer often comes back in the bladder. The new cancer may be found either in the same place as the original cancer or in other parts of the bladder. These tumors are often treated the same way as the first tumor. But if the cancer keeps coming back, a cystectomy may be needed. For some non-invasive tumors that keep growing even with BCG treatment, and where a cystectomy is not an option, immunotherapy with pembrolizumab might be recommended.
Cancers that recur in distant parts of the body can be harder to remove with surgery, so other treatments, such as chemotherapy, immunotherapy, targeted therapy, or radiation therapy, might be needed. For more on dealing with a recurrence, see Understanding Recurrence.
Summary Ofevidence And Guidelines For Metastatic Disease
|
Summary of evidence |
|
|
In a first-line setting, performance status andthe presence or absence of visceral metastases are independent prognosticfactors for survival. |
|
|
In a second-line setting, negative prognostic factorsare: liver metastasis, PS 1 and low haemoglobin . |
|
|
Cisplatin-containing combination chemotherapy canachieve median survival of up to 14 months, with long-term disease-free survival reported in ~15% of patients with nodal disease and good PS. |
GC = gemcitabine plus cisplatin FGFR =fibroblast growth factor receptor HD-MVAC = high-dose intensity
methotrexate, vinblastine, adriamycin plus cisplatin.
Figure 7.2: Flow chart for the management of metastatic urothelialcancer*
*Treatment within clinical trials is highly encouraged.
BSC = best supportive care CR = complete response DD-MVAC = dose dense methotrexate vinblastine doxorubicin cisplatin EV = enfortumabvedotin FDA = US Food and Drug Administration FGFR = pan-fibroblast growth factorreceptor tyrosine kinase inhibitor GFR = glomerular filtration rate IO =immunotherapy PR = partial response PS = performance status SD = stable disease.
Read Also: How To Live With Overactive Bladder
What To Expect With Mibc
Muscle invasive bladder cancer is a serious and more advanced stage of bladder cancer. MIBC is when the cancer has grown far into the wall of the bladder .
For patients with MIBC, the overall prognosis has not changed in the last 30 years. In patients who undergo cystectomy , the cancer return rate can be from 20-30% for stage T2. The cancer return rate can be 40% for T3, greater than 50% for T4 and usually higher when lymph nodes are involved. If bladder cancer does recur, it most often will happen within the first two years after bladder surgery.
Evaluationof Comorbidity Frailty And Cognition
Rochon et al. have shown thatevaluation of comorbidity provides a better indicator of life expectancy in MIBC thanpatient age . Evaluation of comorbidity helps to identifyfactors likely to interfere with, or have an impact on, treatment and the evolution andprognosis of MIBC .
The value of assessing overall health before recommendingand proceeding with surgery was emphasised by Zietman etal., who have demonstrated an association between comorbidity and adversepathological and survival outcomes following RC . Similarresults were found for the impact of comorbidity on cancer-specific and other-causemortality in a population-based competing risk analysis of > 11,260 patients from theSurveillance, Epidemiology, and End Results registries. Age carried the highest riskfor other-cause mortality but not for increased cancer-specific death, while the stage oflocally advanced tumour was the strongest predictor for decreased CSS .
Stratifying older patients according to frailty using amultidisciplinary approach will help select patients most likely to benefit from radicalsurgery and to optimise treatment outcomes . There are manydifferent screening tools available for frailty and local approaches can be used. Examplesinclude the G8 and the Clinical Frailty Scale .
Table 5.1: G8 screening tool
|
Items |
Read Also: Not Being Able To Hold Bladder
Monotherapy Combination Therapy And Multi
Combination therapies based on immunomodulators such as checkpoint inhibitors have shown a synergistic effect to augment the immune response .
A discrete amount of studies are based on combination therapy with chemotherapeutic drugs, intravesical BCG, and immune checkpoint inhibitors, as some trials reported in Table 1 . Currently, an FDA-approved combination therapy is based on intravesical gemcitabine and cisplatin for NMIBCs .
As shown in Table 2, several clinical trials are designed to investigate combination therapies based on BCG immunotherapy and different chemical or biological compounds or vaccines . Combination therapies encompass also combination chemotherapies especially in recurrent and advanced BC including . Furthermore, photodynamic immunotherapy emerged recently to stimulate the immune response in NMIBC BCG-refractory or intolerant to BCG treatment as well .
One frontier of medicinal chemistry is polypharmacology . Benedetti et al. reviewed the immuno-oncological dynamic interactions to design multi-target modulators.
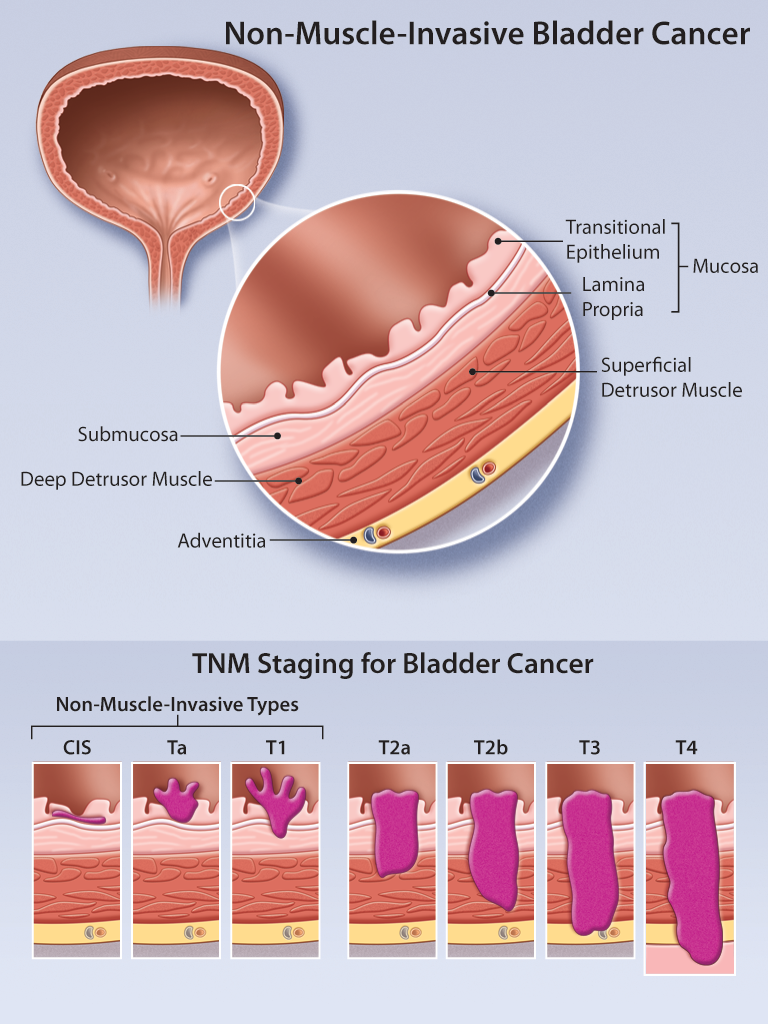
Cellular Classification Of Bladder Cancer
More than 90% of bladder cancers are transitional cell carcinomas derived from the uroepithelium. About 2% to 7% are squamous cell carcinomas, and 2% are adenocarcinomas. Adenocarcinomas may be of urachal origin or nonurachal origin the latter type is generally thought to arise from metaplasia of chronically irritated transitional epithelium. Small cell carcinomas also may develop in the bladder. Sarcomas of the bladder are very rare.
Pathologic grade of transitional cell carcinomas, which is based on cellular atypia, nuclear abnormalities, and the number of mitotic figures, is of great prognostic importance.
References
Don’t Miss: Does Uti Cause Bladder Leakage
Standard Treatment Options For Stage Iv Bladder Cancer
Standard treatment options for patients with T4b, N0, M0 disease
Treatment options for patients with T4b, N0, M0 disease include the following:
Chemotherapy alone or as an adjunct to local treatment
Cisplatin-based combination chemotherapy regimens are the standard of care for first-line therapy for stage IV bladder cancer in patients who can tolerate it. The only chemotherapy regimens that have been shown to result in longer survival in randomized controlled trials are MVAC, dose-dense MVAC, and CMV. GC was compared with MVAC in a randomized controlled trial and neither regimen was associated with a statistically significant difference in response rate or survival. The two regimens are generally considered equivalent, but they have never been compared in a noninferiority trial. Of note, patients with good performance status and lymph node-only disease have a low but significant rate of achieving a durable complete remission with MVAC or GC. In the large, randomized, controlled trial comparing MVAC with GC, for example, 5-year OS in patients with lymph node-only disease was 20.9%. Dose-dense MVAC and standard-dose MVAC were compared in a randomized controlled trial, and dose-dense MVAC was associated with longer survival.
Ongoing studies are evaluating new chemotherapy combinations.
Evidence :
Ongoing studies are evaluating new chemotherapy combinations.
Immunotherapy
Pembrolizumab
Evidence :
Transurethral Resection Of The Bladder Cancer Tumor
This is when the tumor is removed from the urinary tract through the urethra using an electrical force. Transurethral resection is an endoscopic or scope procedure that does not involve making an incision in the body.
Drug therapy after TUR is commonly prescribed for patients with large, multiple or high-grade tumors.
Don’t Miss: Antibiotics For Bladder Infection While Pregnant
Time Schedule For Surveillance
Although, based on low level evidence only, some follow-up schedules havebeen suggested, guided by the principle that recurrences tend to occur within the firstyears following initial treatment. A schedule suggested by the EAU Guidelines Panel includesa CT scan until the third year, followed by annual imaging thereafter.Patients with multifocal disease, NMIBC with CIS or positive ureteral margins are at higherrisk of developing UTUC, which can develop late . In those cases, monitoringof the UUT is mandatory during follow-up. Computed tomography is to be used for imaging ofthe UUT .
Since data for follow-up strategies are sparse, a numberof key questions were included in a recently held consensus project . Outcomes for all statements for whichconsensus was achieved are listed in Section 8.6.
Stage Information For Bladder Cancer
The clinical staging of carcinoma of the bladder is determined by the depth of invasion of the bladder wall by the tumor. This determination requires a cystoscopic examination that includes a biopsy and examination under anesthesia to assess the following:
- Size and mobility of palpable masses.
- Degree of induration of the bladder wall.
- Presence of extravesical extension or invasion of adjacent organs.
Clinical staging, even when computed tomographic and/or magnetic resonance imaging scans and other imaging modalities are used, often underestimates the extent of tumor, particularly in cancers that are less differentiated and more deeply invasive. CT imaging is the standard staging modality. A clinical benefit from obtaining MRI or positron emission tomography scans instead of CT imaging has not been demonstrated.
Read Also: How To Treat Overactive Bladder
Bcg Relapse And Salvage Regimens
Guideline Statement 22
22. In an intermediate- or high-risk patient with persistent or recurrent disease or positive cytology following intravesical therapy, a clinician should consider performing prostatic urethral biopsy and an upper tract evaluation prior to administration of additional intravesical therapy.
Discussion
Urothelial carcinoma, particularly CIS, is considered a field-change disease with the entire urothelium at risk in affected individuals. Clinicians should remain aware of sites outside the bladder as potential sources for metachronous tumors. While the initial diagnostic evaluation includes radiographic/endoscopic visualization of the entire urinary tract, the extra-vesical urothelium remains at long-term risk for subsequent tumor development. Moreover, these sites may harbor disease and contribute to cancer recurrence within the bladder.
Of note, the Panel recognizes that evaluation of the upper urinary tract and urethra may be withheld in select patients who have received a single induction course of intravesical BCG and subsequently have persistent evidence of disease and are to undergo a second course of BCG.
Guideline Statement 23
23. In an intermediate- or high-risk patient with persistent or recurrent Ta or CIS disease after a single course of induction intravesical BCG, a clinician should offer a second course of BCG.
Discussion
Guideline Statement 24
Discussion
Guideline Statement 25
Discussion
Guideline Statement 26
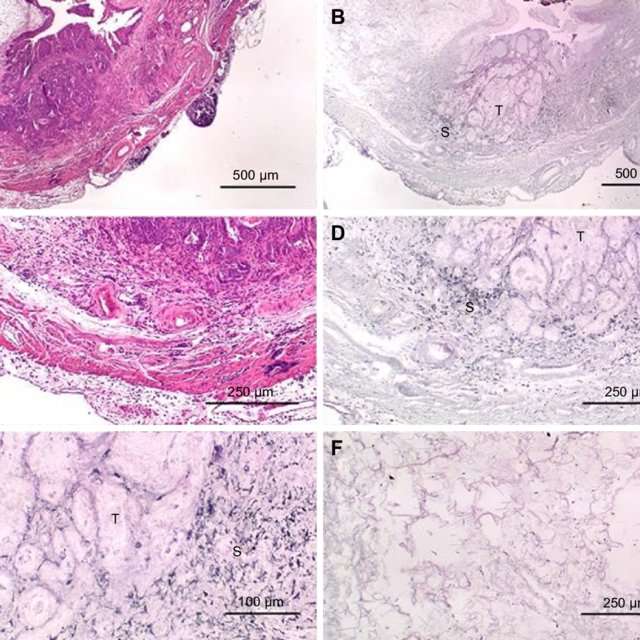
Guidelinesfor The Assessment Of Tumour Specimens
|
Recommendations |
Strength rating |
|
Record the depth ofinvasion . |
Strong |
|
Record margins with special attention paid to theradial margin, prostate, ureter, urethra, peritoneal fat, uterus and vaginalvault. |
|
|
Record the total number of lymph nodes , thenumber of positive LNs and extranodal spread. |
|
|
Record lymphatic or blood vessel invasion. |
|
|
Record the presence of carcinoma in situ. |
|
|
Record the sampling sites as well as information ontumour size when providing specimens to the pathologist. |
Read Also: Non Muscle Invasive Bladder Cancer Guidelines
Standard Treatment Options For Stages Ii And Iii Bladder Cancer
The most common treatments for muscle-invasive bladder cancer are radical cystectomy and radiation therapy. There is no strong evidence from randomized controlled trials to determine whether surgery or radiation therapy is more effective. There is strong evidence that both therapies become more effective when combined with chemotherapy. The treatments with the highest level of evidence supporting their effectiveness are radical cystectomy preceded by multiagent cisplatin-based chemotherapy and radiation therapy with concomitant chemotherapy.
Radical cystectomy
Radical cystectomy is a standard treatment option for stage II and stage III bladder cancer, and its effectiveness at prolonging survival increases if it is preceded by cisplatin-based multiagent chemotherapy. Radical cystectomy is accompanied by pelvic lymph node dissection and includes removal of the bladder, perivesical tissues, prostate, and seminal vesicles in men and removal of the uterus, fallopian tubes, ovaries, anterior vaginal wall, and urethra in women. Studies of outcomes after radical cystectomy report increased survival in patients who had more, rather than fewer, lymph nodes resected whether this represents a therapeutic benefit of resecting additional nodes or stage migration is unknown. There are no randomized controlled trials evaluating the therapeutic benefit of lymph node dissection in this setting.
Evidence :
Evidence :
Segmental cystectomy
Treatment Options For Recurrent Bladder Cancer
Treatment options for patients with recurrent bladder cancer include the following:
Palliative radiation therapy should be considered for patients with symptomatic tumors.
Clinical trials
Recurrent or progressive disease in distant sites or after definitive local therapy has an extremely poor prognosis, and clinical trials should be considered whenever possible.
You May Like: Can You Live Without A Bladder
Cystoscopy With Cautery Destruction Of The Bladder Tumor
Cystoscopy is an outpatient procedure during which a thin, lighted tube with a camera is passed through the urethra into the bladder, allowing your doctor to see the inside of the bladder.
Most modern cystoscopes are also equipped with channels that permit small instruments to be passed into the bladder. During a cystoscopy, your doctor may use these instruments to remove tissue, stop bleeding with a special electrical device called an electrocautery or even perform laser treatment. If the bladder cancer tumor is small enough, this cautery may be used to remove the cancer.
Options And Choices For Treatment
Your options for treatment will depend on how much your cancer has grown.
There are essentially two options:
- Bladder removal with chemotherapy or without chemotherapy
- Chemotherapy with radiation
Bladder Removal Procedures
Neoadjuvant cisplatin-based chemotherapy
Bladder removal with chemotherapy increases survival rates for bladder cancer patients. Before removing your bladder, your physician will likely offer neoadjuvant chemotherapy. Adjuvant means, added to. If you have MIBC, you may get chemotherapy along with having your bladder removed. Before your doctor does a radical cystectomy , he/she may try to shrink your tumor first with neoadjuvant cisplatin-based chemotherapy . This means the drug cisplatin or a combination of drugs including cisplatin is first given as chemotherapy and then bladder removal is done afterwards.
Adjuvant chemotherapy means the drug is given after surgery. Your doctor may offer this treatment if it is appropriate for you.
Also Check: Will Cranberry Pills Help An Overactive Bladder
Treating Stage Ii Bladder Cancer
These cancers have invaded the muscle layer of the bladder wall , but no farther. Transurethral resection is typically the first treatment for these cancers, but it’s done to help determine the extent of the cancer rather than to try to cure it.
When the cancer has invaded the muscle, radical cystectomy is the standard treatment. Lymph nodes near the bladder are often removed as well. If cancer is in only one part of the bladder, a partial cystectomy may be done instead. But this is possible in only a small number of patients.
Radical cystectomy may be the only treatment for people who are not well enough to get chemo. But most doctors prefer to give chemo before surgery because it’s been shown to help patients live longer than surgery alone. When chemo is given first, surgery is delayed. This is not a problem if the chemo shrinks the bladder cancer, but it might be harmful if the tumor continues to grow during chemo.
If cancer is found in nearby lymph nodes, radiation may be needed after surgery. Another option is chemo, but only if it wasn’t given before surgery.
For people who have had surgery, but the features of the tumor show it is at high risk of coming back, the immunotherapy drug, nivolumab, might be offered. When given after surgery, nivolumab is given for up to one year.
For patients who cant have surgery because of other serious health problems, TURBT, radiation, chemotherapy, or some combination of these may be options.
What About Clinical Trials
You may hear about possible clinical trials for your bladder cancer. Clinical trials are research studies that involve people. They test if a new treatment or procedure is safe and effective.
Through clinical trials, doctors find new ways to improve treatments and the quality of life for people with disease. Although clinical trials may or not be effective for your particular problem, they present an option to think about. Trials are available for all stages of cancer.
Also Check: What Causes Overactive Bladder In Women
Urinarydiversion After Radical Cystectomy
From an anatomical standpoint, three alternatives are currently used aftercystectomy:
- abdominal diversion, such as an uretero-cutaneostomy, ileal or colonic conduit, andvarious forms of a continent pouch
- urethral diversion, which includes various forms of gastrointestinal pouches attached tothe urethra as a continent, orthotopic urinary diversion
- rectosigmoid diversions, such as uretero-rectostomy .
Different types of segments of the intestinal tract have been used toreconstruct the urinary tract, including the stomach, ileum, colon and appendix .
Several studies have compared certain aspects ofhealth-related quality of life such as sexual function, urinary continence and bodyimage in patient cohorts with different types of urinary diversion . However, further research evaluating the impact ofpre-operative tumour stage, functional- and socio-economic status, and time interval toprimary surgery are needed.
7.3.6.1.Patient selection and preparationsfor surgery
In consultation with the patient, both an orthotopic neobladder and ilealconduit should be considered in case reconstructive surgery exposes the patient to excessiverisk .
Ensuring that patients make a well-informed decisionabout the type of urinary diversion is associated with less decision regretpost-operatively, independent of the method selected .
In the presence of positive LNs, orthotopic neobladdercan nevertheless be considered in case of N1 involvement but not in N2 or N3 tumours .
7.3.6.2.2.Ileal conduit