Adjuvant/neoadjuvant Chemotherapy For T3 T4 N1
Since 1976, when cisplatin entered clinical trials in bladder cancer as a single agent, chemotherapy in bladder cancer has evolved a great deal. Sequential trials showed its superiority over supportive care and then the era of M-VAC started. Combination chemotherapy such as M-VAC was found to be superior to cisplatin alone and to CISCA . Since then M-VAC or M-VEC has been studied in many trials as mentioned above. Looking at the toxicity profile, attempts have been made to either eliminate epirubicin and vinblastin from M-VEC or use gemcitabine + cisplatin combination . Both these regimes have shown equal results with less toxicity perhaps cost would be an issue to GC.
Whats The Treatment For Stage 3 Bladder Cancer
The standard treatment for stage 3 bladder cancer is surgery, usually in combination with other therapies.
Be sure to discuss your treatment goals with your doctor. Assess all the potential benefits and risks of each therapy. Some treatments aim for a cure. Others work to slow progression or relieve symptoms. The recommended treatment may depend on your overall health.
If cancer continues to progress or comes back during treatment, you may have to reconsider your options.
N Categories For Bladder Cancer
The N category describes spread only to the lymph nodes near the bladder and those along the blood vessel called the common iliac artery. These lymph nodes are called regional lymph nodes. Any other lymph nodes are considered distant lymph nodes. Spread to distant nodes is considered metastasis . Surgery is usually needed to find cancer spread to lymph nodes, since this is seldom seen on imaging tests.
The N categories are described in the table above, except for:
NX: Regional lymph nodes cannot be assessed due to lack of information.
N0: There’s no regional lymph node spread.
Don’t Miss: Exercises To Stop Bladder Leakage
Is Surgery Advisable In Poor/minimal Responders And No Responders To Chemotherapy
One of the important prognostic factors that determines the success of combination therapy is the degree of response to chemotherapy. As discussed in this article before, the patients who achieve better survival rate are the ones who had major/complete response to chemotherapy and those having non-visceral metastasis. No patient who achieved less than a major response to chemotherapy survived five years in any of the series reported in this article, despite post chemotherapy surgery. Therefore one has to be extremely careful in advising surgery to these patients.
Surgical resection in chemo refractory patients has been rarely rewarding and is rarely reported except in palliation of selected cases. A study from Germany looked at these patients who underwent surgery despite poor response to chemotherapy and found very dismal results.
Newer Agents And Ongoing Trials In Adjuvant Setting
In the light of the success of taxanes and gemcitabine in metastatic bladder cancer, efforts have been made to use them with cisplatin in adjuvant setting. The combination of gemcitabine and cisplatin has similar survival outcomes with less toxicity compared to M-VAC in advanced or metastatic setting.
There are many ongoing trials looking at adjuvant chemotherapy in locally advanced bladder cancer such as Cancer and Leukemia Group B 90104 , EORTC 30994 , SWOG . The results would be interesting and would perhaps help in deciding if this could be a standard of care.
You May Like: Causes Of Weak Bladder Muscles
The Stages Of Invasive Bladder Cancer
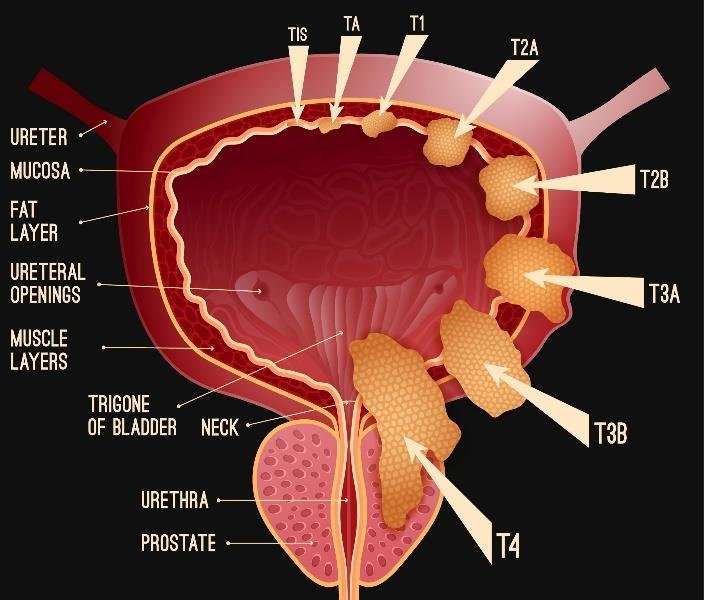
Your doctor diagnoses invasive bladder cancer by looking at how far cancer tumours have grown into the bladder. This is called the T stage . There are three T stages of invasive bladder cancer:
- T2 means cancer has grown into the muscle layer of the bladder
- T3 means cancer has grown through the muscle layer into the fatty tissue layer
- T4 means cancer has grown outside the bladder OR into the prostate, womb or vagina, OR into the wall of the pelvis or tummy
Your doctor also looks at:
- whether cancer has spread to any lymph nodes
- whether or not it has spread to other parts of the body like the bones, lungs or liver
Use Of Nomograms In Locally Advanced Bladder Cancer
Currently, treatment strategies for advanced bladder cancer in many oncological centers are based on the data discussed above. Many centers opt for radical cystectomy followed by adjuvant chemotherapy or neoadjuvant chemotherapy followed by surgery alone or additional courses of chemotherapy following surgery. There are no set guidelines for this as yet. The current literature does give us a rough idea about chances of recurrence-free survival, but better ways are now explored with the help of nomograms.
Recently, attempts have been made to use the nomograms in predicting recurrence-free survival. The study from the International Bladder Cancer Nomogram Consortium by Bochner et al., had studied 9000 patients from 12 different centers who had undergone radical cystectomy and bilateral pelvic LN dissection for the possible risk of recurrence. The nomograms fared much better than standard AJJC staging and standard pathological subgrouping. Concordance index of nomograms was 0.75 as compared to concordance index of standard TNM AJCC classification and that of standard pathological subgrouping . The authors have suggested using the nomograms rather than TNM/pathological subgroupings in predicting the recurrence. The same authors have consolidated this data once again recently. Another study by Karakiewicz et al., who had studied 728 patients of advanced bladder cancer has shown that the nomograms were 3.2% more accurate than TNM AJCC classification.
Recommended Reading: Non Muscle Invasive Bladder Cancer Guidelines
Standard Treatment Options For Stages Ii And Iii Bladder Cancer
The most common treatments for muscle-invasive bladder cancer are radical cystectomy and radiation therapy. There is no strong evidence from randomized controlled trials to determine whether surgery or radiation therapy is more effective. There is strong evidence that both therapies become more effective when combined with chemotherapy. The treatments with the highest level of evidence supporting their effectiveness are radical cystectomy preceded by multiagent cisplatin-based chemotherapy and radiation therapy with concomitant chemotherapy.
Radical cystectomy
Radical cystectomy is a standard treatment option for stage II and stage III bladder cancer, and its effectiveness at prolonging survival increases if it is preceded by cisplatin-based multiagent chemotherapy. Radical cystectomy is accompanied by pelvic lymph node dissection and includes removal of the bladder, perivesical tissues, prostate, and seminal vesicles in men and removal of the uterus, fallopian tubes, ovaries, anterior vaginal wall, and urethra in women. Studies of outcomes after radical cystectomy report increased survival in patients who had more, rather than fewer, lymph nodes resected whether this represents a therapeutic benefit of resecting additional nodes or stage migration is unknown. There are no randomized controlled trials evaluating the therapeutic benefit of lymph node dissection in this setting.
Evidence :
Evidence :
Segmental cystectomy
Neoadjuvant Chemotherapy For Locally Advanced And Metastatic Bladder Cancer
In the light of excellent response to cisplatin-based chemotherapy in metastatic bladder cancer, many trials have been conducted and are ongoing, studying the role of neoadjuvant chemotherapy followed by cystectomy in locally advanced bladder cancer. The results of the three major trials conducted so far have shown significant downstaging of the disease allowing a better surgical clearance, higher recurrence-free survival, almost 80-90% in pT0 on post cystectomy patients and a small but demonstrable 5-6% absolute survival benefit and 10-13% reduction in risk of death from bladder cancer.
The MRC/EORTC trial used CMV as a regime for neoadjuvant therapy in advanced bladder cancer and found an absolute improvement in survival of 5.5% .
Nordic trials I and II which used neoadjuvant chemotherapy cisplatin/doxorubicin and cisplatin/methotrexate regimes in locally advanced bladder cancer patients have found overall five-year survival of 56% in the neoadjuvant group versus 48% with cystectomy alone, favoring chemotherapy .
Meta-analysis of all these trials in more than 3000 patients confirms that neoadjuvant chemotherapy improves survival in locally advanced bladder cancer. Platinum-based combination chemotherapy has a 5% absolute survival at five years and a 13% reduction in the risk of death from bladder cancer.
Read Also: What Is Overactive Bladder Syndrome
Current Treatment And Outcomes Benchmark For Locally Advanced Or Metastatic Urothelial Cancer From A Large Uk
- 1Leeds Cancer Centre, St James’s University Hospital, Leeds, United Kingdom
- 2IQVIA, London, United Kingdom
- 3Janssen Pharmaceuticals, Wycombe, United Kingdom
- 4Bradford Royal Infirmary, Bradford, United Kingdom
- 5School of Medicine, University of Leeds, Leeds, United Kingdom
Objectives: To characterize treatment patterns and survival outcomes for patients with locally advanced or metastatic malignancy of the urothelial tract during a period immediately preceding the widespread use of immune checkpoint inhibitors in the UK.
Patients and Methods: We retrospectively examined the electronic case notes of patients attending the Leeds Cancer Center, UK with locally advanced or metastatic urothelial carcinoma, receiving chemotherapy between January 2003 and March 2017. Patient characteristics, treatment patterns, and outcomes were collected. Summary and descriptive statistics were calculated for categorical and continuous variables as appropriate. The KaplanMeier method was used to estimate median survival and Cox regression proportional hazards model was used to explore relationships between clinical variables and outcome.
This study provides a useful benchmark for outcomes achieved in a real-world setting for patients with locally advanced or metastatic UC treated with chemotherapy in the immediate pre-immunotherapy era.
Treating Bladder Cancer That Progresses Or Recurs
If cancer continues to grow during treatment or comes back after treatment , treatment options will depend on where and how much the cancer has spread, what treatments have already been used, and the patient’s overall health and desire for more treatment. Its important to understand the goal of any further treatment if its to try to cure the cancer, to slow its growth, or to help relieve symptoms as well as the likely benefits and risks.
For instance, non-invasive bladder cancer often comes back in the bladder. The new cancer may be found either in the same place as the original cancer or in other parts of the bladder. These tumors are often treated the same way as the first tumor. But if the cancer keeps coming back, a cystectomy may be needed. For some non-invasive tumors that keep growing even with BCG treatment, and where a cystectomy is not an option, immunotherapy with pembrolizumab might be recommended.
Cancers that recur in distant parts of the body can be harder to remove with surgery, so other treatments, such as chemotherapy, immunotherapy, targeted therapy, or radiation therapy, might be needed. For more on dealing with a recurrence, see Understanding Recurrence.
Recommended Reading: Radiotherapy Success Rate For Bladder Cancer
Carcinogenesis And Risk Factors
Increasing age is the most important risk factor for most cancers. Other risk factors for bladder cancer include the following:
- Use of tobacco, especially cigarettes.
- Family history of bladder cancer.
- HRAS mutation .
- Rb1 mutation.
There is strong evidence linking exposure to carcinogens to bladder cancer. The most common risk factor for bladder cancer in the United States is cigarette smoking. It is estimated that up to half of all bladder cancers are caused by cigarette smoking and that smoking increases a persons risk of bladder cancer two to four times above baseline risk. Smokers with less functional polymorphisms of N-acetyltransferase-2 have a higher risk of bladder cancer than other smokers, presumably because of their reduced ability to detoxify carcinogens.
Surgery As A Consolidation Therapy
Patients who respond to primary chemotherapy may benefit from surgical consolidation if the disease is limited and located in the regional lymph nodes or metastatic site/sites amenable to surgical removal . The concept of metastasectomy in urothelial carcinoma was first described in the early 1980s, when Cowles et al. reported long-term survival for six patients who underwent wedge resection for solitary pulmonary metastasis. After more than one decade, multiple reports started to demonstrate the suggested benefits of surgical excision of metastatic lesions as part of a multimodality approach . In the age of immunotherapeutics, reduction of tumor burden may become even more important.
Recommended Reading: The Most Frequent Initial Symptom Of Bladder Cancer Is
Managing Locally Advanced Or Metastatic Bladder Cancer
care services have tended to be requested because of profound physical symptoms in people with terminal bladder cancer. Increasing use of cross sectional imaging is detecting incurable disease much earlier, when there are often no physical symptoms. However the psychological and spiritual impact of a terminal diagnosis will always be profound and input from specialist palliative care at this earlier stage may be of significant benefit. The specialist palliative care needs of people with advanced bladder cancer are covered in . This chapter deals with the use of for people with distant metastases and with specific symptoms from locally advanced or metastatic bladder cancer.
Locally Advanced Bladder Cancer
Locally advanced bladder cancer means your cancer has spread:
- through the bladder and into the nearby tissues including the vagina, womb, ovaries, prostate, and back passage
- into nearby lymph nodes
Advanced bladder cancer means that your cancer has spread to:
- the wall of the tummy or between the hips
- distant lymph nodes
Read Also: What To Do For A Bladder Infection
What Is Cervical Cancer
Cervical cancer is a malignant tumor of the cervix, which is the lowermost part of the uterus.
The most common cause of almost all cervical cancer cases is Human Papillomavirus , which is the most common sexually transmitted infection . Many people with HPV do not develop any symptoms but can still infect others through sexual contact. HPV can cause warts in various parts of the body, including the genitals, or cervical cancer.
Signs and symptoms of locally advanced cervical cancer include, but are not limited to, a mass in the vaginal area, swelling of the legs as a result of enlarged lymph nodes, blockage in the urinary tract, irregular bleeding and discharge, and pain.
All women are at risk for cervical cancer, but it most often occurs in women over age 30. Cervical cancer is highly preventable in most Western countries because of screening tests, such as a pap smear, and a vaccine to prevent HPV infections. When detected early, cervical cancer is highly treatable and associated with long-term survival and good quality of life.
Intraoperative Finding Of Enlarged Lymph Nodes
Herr et al. reported on a series of 84 patients with grossly enlarged resectable lymph node at time of RC and PLND. The median survival was 19 months and about one fourth of patients achieved long term survival of 10 years. They concluded that if PLND can be performed completely and safely, it is better to proceed with RC and PLND .
You May Like: Clear A Bladder Infection Without Antibiotics
Post Chemo Surgery For Metastatic Bladder Cancer
The results of post chemotherapy surgery that clears the pelvis and regional LNs are encouraging, but the same cannot be held true for patients who have undergone metastatectomy of the lesions outside the pelvis. The results of the three reported series have shown median survival time of around 30 months with approximately one-third of these patients surviving for three to five years.
Selected Adverse Events Analysis
Blood tests to identify hematological and hepatic treatment-related adverse events were available for 98.0% of the platinum-treated sub-cohort. The distribution of events was similar between cisplatin-based and carboplatin-based sub-cohorts, with neutropenia representing the most common grade 3 or 4 AE observed in both sub-cohorts . Severity of recorded events tended to be higher in the carboplatin sub-cohort.
Figure 4. Adverse events recorded for study cohort by common terminology criteria for adverse events grade of severity and by platinum sub-cohort. Numbers tested: blood disorders , liver disorders . Cis, cisplatin sub-cohort carbo, carboplatin sub-cohort ALT, alanine aminotransferase AST, aspartate aminotransferase ALK, alkaline.
You May Like: Why Do I Get Frequent Bladder Infections
Cellular Classification Of Bladder Cancer
More than 90% of bladder cancers are transitional cell carcinomas derived from the uroepithelium. About 2% to 7% are squamous cell carcinomas, and 2% are adenocarcinomas. Adenocarcinomas may be of urachal origin or nonurachal origin the latter type is generally thought to arise from metaplasia of chronically irritated transitional epithelium. Small cell carcinomas also may develop in the bladder. Sarcomas of the bladder are very rare.
Pathologic grade of transitional cell carcinomas, which is based on cellular atypia, nuclear abnormalities, and the number of mitotic figures, is of great prognostic importance.
References
Role Of Neoadjuvant Chemotherapy
In the landmark phase III randomized intergroup clinical trial conducted by the Southwest Oncology Group in patients with MIBC T2T4aN0M0, Grossman et al. demonstrated that the estimated risk of death is reduced by 25% in patients receiving three cycles of M-VAC NAC plus RC compared to RC alone. The trial also proved that patients who had been down-staged to pT0 had a better survival than those who did not achieve complete response . An update of the advanced bladder cancer meta-analysis collaboration systematic review and meta-analysis based on 11 trials with 3,005 patients supported this beneficial effect of NAC over definitive local therapy alone with a 14% reduction in the estimated risk of death compared to definitive local therapy alone. This is also equivalent to an absolute survival benefit of 5%, improving OS from 45% to 50% at 5 years . NAC was not associated with increased risk of death, did not affected the patients chance of undergoing RC and did not increase perioperative morbidity . Despite that and the compelling level 1 evidence, NAC is still underutilized and treatment is often with RC alone or RC with adjuvant chemotherapy .
Recommended Reading: How To Know If You Have Bladder Problems