What Is Sling Surgery
Recovering from bladder sling surgery takes several weeks. Because of the vaginal incision, doctors usually recommend no tampons or sex for up to 6 weeks. There also are limitations on working out and lifting heavy weights so the sling doesnt get moved out of place. After weeks of recovery, you can resume full activity and ideally should be in total control of your bladder. Success rates vary, but one meta-analysis of surgery reported an 82% success rate.
The Ultimate Conservative Treatment
In the study that investigated surgical success rates, the second most effective treatment was pelvic floor exercises. Youve probably heard this advice before, particularly after childbirth: Do your Kegels. Although pelvic floor exercises have been proven to be effective for SUI, many women dont do Kegels correctly or consistently enough to notice a difference. In order to better support the bladder, you must regularly contract the relevant muscles in order to strengthen the pelvic floor. But its difficult to remember to do Kegels or even to know whether youre squeezing the right muscles.
So what are the alternatives? Several conservative treatment options are available for you to consider before surgery, including devices that actually perform Kegels for you.
How Painful Is Bladder Lift Surgery
Bladder lift surgery is often done laparoscopically.
This means that a surgeon will make just a few small cuts in the abdomen during the surgery. To perform the surgery, theyll use a small camera and tools inserted through tubes placed in the cuts.
Laparoscopic procedures are less invasive than open surgery. Recovery time for midurethral sling surgery and colposuspension performed laparoscopically is often much quicker than for open surgery.
Youll most likely leave the hospital after your surgery to recover at home. In some cases, though, you may need to stay overnight.
On the other hand, a traditional sling surgery and colposuspension with abdominal surgery usually require that you stay in the hospital to recover for a few days.
You may feel some pain or cramping in your lower abdomen and may need to take pain medications for 1 or 2 weeks. Most people fully recover from this procedure in about 6 weeks.
As with any surgery, bladder lift surgery comes with some risks. These include:
- bleeding
Also Check: Cystoscopy Transurethral Resection Of Bladder Tumor
What To Expect After Surgery
Urethral sling surgery can be safely performed in an outpatient surgery center. There is normally a 2-4 week recovery period, during which you should avoid doing too much activity to allow your body to properly heal.
Its likely you will feel some pain and discomfort where your incision is and you may feel some cramping in your abdomen. Your doctor will prescribe you medication to help with the pain during the first few days after surgery. If you continue to experience pain, be sure to contact your doctor immediately.
Somethings Not Right Down There

Discovering your organs are out of place can be alarming! Most women notice a bulge of tissue protruding from their vagina when theyre showering or using the toilet, explains Tracy Cannon-Smith, M.D., a Urology Partners surgeon certified in female pelvic medicine and reconstructive surgery. In some cases, a woman may have to push the bulge in vaginally to urinate or have a bowel movement. Other women say they feel like theyre sitting on a ball.
There are other signs, too. Vaginal pain, bleeding, spotting or feeling like you have pulled a groin muscle are all symptoms of POP. Experts estimate that nearly 50 percent of all women will struggle with pelvic organ prolapse at some point during their lifetime. For a woman who is still sexually active, prolapse can be embarrassing and prevent intimacy with her partner, Dr. Cannon-Smith adds. Fortunately, there are several ways to fix prolapsevaginally and robotically.
Read Also: What Is The Best Medication For Bladder Infection
Where Can Someone Get More Information On Prolapsed Bladders
- Urologic conditions that can occur around the time a woman goes through menopause include
- bladder control problems,
- bladder prolapse , and
- urinary tract infections.
Recommended Reading: Florida Bladder Institute Patient Portal
Anterior Vaginal Wall Prolapse
Anterior vaginal wall prolapse often occurs at the top of the vagina where the uterus used to be in women who have had a hysterectomy. This type of prolapse occurs when the bladderâs supportive tissue, called fascia, stretch or detach from the attachments securing it to the pelvic bones. With this loss of support, the bladder falls down into the vagina. As this condition worsens, the prolapsed pelvic organs may bulge outside the opening of the vagina causing pressure, discomfort or pain. Other symptoms MAY include:
- Urinary frequency, nighttime voiding, loss of bladder control and recurrent bladder infectionsusually due to the bladder not emptying well
- Stress urinary incontinence with activity such as laughing, coughing, sneezing, or exercise) cause by weakened support for the urethra
You May Like: Cramping In Bladder Or Uterus
You May Like: How To Strengthen Your Bladder
How Is A Vaginal Sling Done
Traditional sling: The surgeon will make a small incision inside the vagina and use an instrument to place a soft, thin tube under the urethra by threading it through the tunnel.
The other end of the tube is sewn to ligaments on either side of your vaginal opening so that it acts like a hammock that holds the urethra in place while adding support to your bladder.
A vaginal sling can be done during a regular surgery or under anesthesia without needing an overnight hospital stay.
Mid-urethral sling: In order to fix urinary incontinence, a mid-urethral sling is used by inserting a narrow strip of synthetic material underneath the urethra and attaching it to the bladder. The new placement of your urethra allows urine flow to be redirected while strengthening the support around the organ.
Smaller incisions are needed for this surgery, but more than one may be required if youre obese , pregnant or post-menopausal. Additionally, a trial may be done to see how you do with the surgery before making the decision to remove your bladder sling.
In order to hold everything in place properly, this surgery is done under general anesthesia so that youll need an overnight stay at the hospital for recovery.
This surgery can sometimes cause complications such as:
- Pain while urinating
- Bladder puncture or injury to other organs during surgery.
Bladder Prolapse At A Glance
- Bladder prolapse occurs when the hammock of pelvic floor muscles that support the bladder weakens and the bladder drops out of its proper position.
- Bladder prolapse, also called cystocele, commonly occurs in women due to age, injury or childbirth.
- The main symptom of BP is tissue protruding in the vagina, which women describe as a feeling like a ball.
- BP is categorized on a scale of 1 to 4, based on how far the bladder drops into the vagina.
- Treatment ranges from lifestyle changes to medications and surgery.
You May Like: Hernia Of The Urinary Bladder
What Is A Prolapsed Bladder
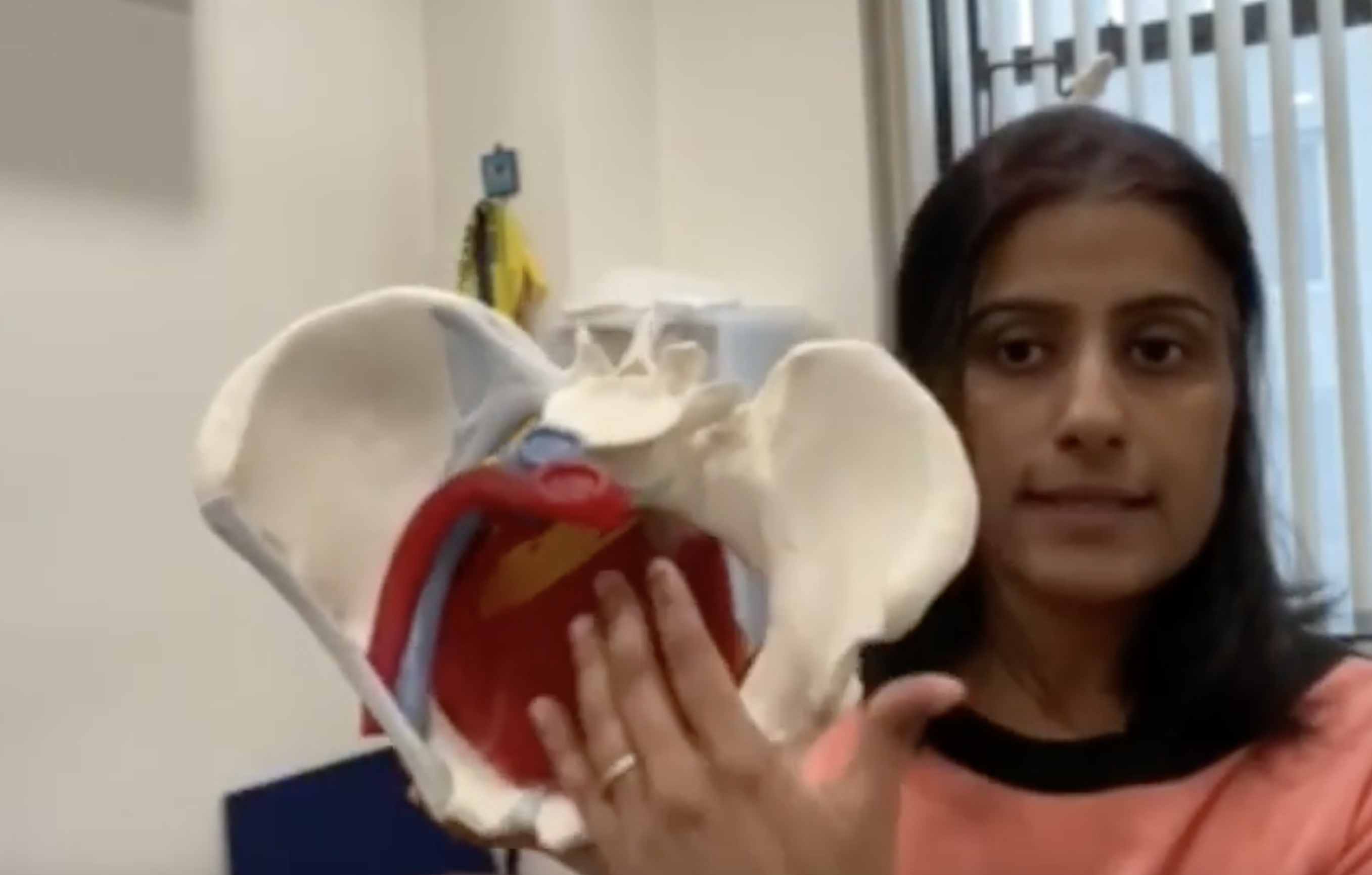
Pelvic organ prolapse is a surprisingly common condition. In fact, its estimated that about half of women over 50 have some level of prolapse. The pelvic floor is a web of muscles and tissues that supports your pelvic organs, including the bladder, bowel, and uterus. When these muscles and tissues become weakened or damaged, one or more of these pelvic organs can drop or collapse, causing uncomfortable symptoms.
While any of the organs listed above can drop, the most common type of prolapse is a dropped bladder, also known as a cystocele.
There are different levels of a prolapsed bladder, which are measured on a grade from 1-3 with 1 being the mildest, and grade 3 being the most severe. The grade of prolapse is measured by how far the bladder has fallen into the vagina. A grade 1 cystocele is when the bladder has dropped only slightly. A grade 2 cystocele is when the bladder has dropped to the opening of the vagina. A prolapsed bladder is classified as a grade 3 when the bladder has fallen so far that it bulges out of the vagina.
Recommended Reading: Can You Have A Bladder Infection Without Symptoms
How To Diagnose And Treat A Prolapsed Bladder
This article was medically reviewed by Lacy Windham, MD. Dr. Windham is a board certified Obstetrician & Gynecologist in Tennessee. She attended medical school at the University of Tennessee Health Science Center in Memphis and completed her residency at the Eastern Virginia Medical School in 2010, where she was awarded the Most Outstanding Resident in Maternal Fetal Medicine, Most Outstanding Resident in Oncology, and Most Outstanding Resident Overall.There are 12 references cited in this article, which can be found at the bottom of the page.wikiHow marks an article as reader-approved once it receives enough positive feedback. In this case, 96% of readers who voted found the article helpful, earning it our reader-approved status. This article has been viewed 112,458 times.
Also Check: Galvanized Pressure Tank Vs Bladder Tank
What To Expect After Bladder Sling Surgery
Urinary incontinence is one of the most common issues for women to experience. In fact, around 46 percent of women suffer from stress-induced incontinence involuntary bladder leaks triggered by things like coughing, laughing and exercise yet shame and embarrassment often keep discussion of this topic silent. Here at Proof, we understand the difficulties that come with bladder leakage, and believe that incontinence is nothing to be ashamed about. Our bodies are complex, and deserve to be taken care of no matter how personal the issue. For many women, non-surgical interventions like physical therapy and even pessary rings can be a great solutionespecially when the issue is addressed early on. However, when left untreated, SUI can worsen and become unmanageable. In severe cases, surgery may be a viable option. Lets take a look at the most common surgical intervention, and what to expect after bladder sling surgery.
Complication Rates By Type Of Sling
Before undergoing bladder sling surgery, women should ask their doctors about the technique they plan to use. Complication rates may vary depending on the type of mesh sling and technique.
A 2010 study of bladder sling procedures by Z. Chen and colleagues published in Urologia analyzed the outcomes of 187 women who received bladder slings to treat stress urinary incontinence. Authors found that transobturator vaginal tape inside-out and transobturator vaginal tape out-inside are simpler techniques with fewer complications compared to tension-free vaginal tape .
Women who used TVT had an average hospital stay of five days versus about two days for the TOT group.
The complication rate in the study was:
- 15.6 percent for tension-free vaginal tape
- 9.20 percent for transobturator vaginal tape inside-out
- 8.90 percent for transobturator vaginal tape out-inside
Complications from the procedures included discomfort with urinating, bleeding outside blood vessels and dysfunction of lower limbs. TVT was the only procedure associated with bladder perforation. Despite the complication rate, doctors found the slings safe.
The three tension-free urethral suspension techniques have similar efficacy, all of them are safe and effective procedures for the treatment of female SUI, authors wrote.
Recommended Reading: Tb Virus Treatment For Bladder Cancer
Signs And Symptoms Of Vaginal Sling Failure
The FDA released a warning in 2008 to alert women to potential vaginal sling complications, which include:
- Infection
- Bowel, bladder and blood vessel perforation during insertion
- Vaginal scarring
- Dyspareunia
It is believed that many of these problems stem from shrinkage, contraction, or erosion of the mesh.
Peeing During Sex Is Stressful But These Treatments Help
A loss of bladder control during sex is a secret many women dont discuss, even with their doctors. But theres no need to endure in silence.
Not long after her first son was born in 2005, Elizabeth began experiencing periodic incontinence, or involuntary urination.
The stress of always worrying if shed leak took its toll, and Elizabeth became depressed and anxious, particularly about sex.
I definitely limited sex, said Elizabeth, 41. I was always damp down there, and sexy, she told Healthline. There were all these accommodations and obstacles. I would never be on top because of the risk of urinating on my husband, and I was very reluctant to have sober sex. It was easier to have a few drinks and have sex because I was less inhibited, and if I did leak, I could blame it on being buzzed.
Elizabeth says she never had a gushing episode during sex, but the fear of leaking became an insidious worry.
A lactation consultant had told me that I needed to urinate before and after sex to avoid a urinary tract infection. But then Id think I was going to leak again, and Id have to go one more time. Leading up to orgasm can mimic the need to go, and that inhibited me so much, because I knew I had problems holding in my urine, Elizabeth recalled.
Elizabeth isnt alone. The Mayo Clinic estimates nearly 20 million Americans have urinary incontinence, and of them, 85 percent are women.
Recommended Reading: Can Diabetes Cause Bladder Problems
How Do You Treat Stress Incontinence Naturally
In addition to pelvic floor exercises, these steps can also improve stress incontinence:
- Eat high-fiber foods and drink plenty of water to prevent constipation, which can make incontinence worse.
- Get help to quit smoking or using tobacco products.
- Maintain a healthy weight.
- Manage conditions like diabetes and high blood pressure.
- Use the restroom at set times .
Can Pelvic Floor Exercises Treat Stress Incontinence
Yes, pelvic floor exercises can improve stress incontinence. These exercises strengthen the muscles that support your urinary system. It can be challenging to correctly work and strengthen your pelvic floor muscles.
A physical therapist who specializes in pelvic floor disorders can help you master the proper techniques. This provider may use biofeedback to ensure you work the right muscles. It can take four to six weeks of regular exercise to see symptoms improve.
Don’t Miss: I Feel A Lot Of Pressure On My Bladder
What Are Stress Incontinence Symptoms
Leaking urine when theres pressure on your bladder is the top sign of stress incontinence. Mild stress incontinence may cause you to leak drops of urine during activities like heavy exercise, laughing, coughing or sneezing.
With moderate to severe stress incontinence, you may leak more than a tablespoon of urine even during less strenuous activities like standing up or bending over. You may even leak urine while having sex.
What Are The Advantages Of The Male Sling Procedure
If the patient was selected properly, the chance of a positive outcome is very high. According to studies, most patients say that the procedure is sufficient to treat urinary incontinence. Patients reduce the severity and frequency of urinary leaks and regain their quality of life .
Additionally, these patients do not require previous training or rehabilitation. They experience improvements shortly after recovering instead of going through an extra step.
Don’t Miss: Frequent Bladder Infections In Females
When Should I See A Health Care Professional
See a health care professional if you have symptoms of a bladder problem, such as trouble urinating, a loss of bladder control, waking to use the bathroom, pelvic pain, or leaking urine.
Bladder problems can affect your quality of life and cause other health problems. Your health care professional may be able to treat your UI by recommending lifestyle changes or a change in medicine.
How Painful Is Bladder Sling Surgery

The actual procedure should be painless, since it will involve anesthesia. During bladder sling surgery recovery, you may feel pain at the incision site, as well as some internal abdominal cramping. Your physician should prescribe you with pain medication during those first few days or weeks, but if your pain is unmanageable, see your doctor right away.
Also Check: Ways To Control Your Bladder
What Else Causes Bladder Control Problems In Women
Certain life events and health problems can lead to stress incontinence in women by weakening the pelvic floor muscles
- pregnancy and childbirth
- menopause
Weak pelvic floor muscles can make it hard for your bladder to hold urine in during stress incontinence. Stress incontinence occurs when an actioncoughing, sneezing, laughing, or physical activityputs pressure on your bladder and causes urine to leak. A weak pelvic floor can also cause fecal incontinence, or bowel control problems.
Counting The Cost Of Sling Surgery
In addition to health risks, sling surgery is a costly option for leaky bladders. The price tag can range from $6,000 to $25,000. And even after surgery, women still spend on average $190 a year to manage residual leaks, spending money on pads, laundry, and dry cleaning. For those women who need a second surgery to remedy a bad first outcome, the total cost can quickly rise to $50,000 for surgical removal of a failed implant.
On the flip side, electing not to pursue any treatment is expensive, as well. The same study referenced above found that women spend on average $750 per year managing their incontinence symptoms.
You May Like: Does Bladder Infection Cause Incontinence
Surgery For A Pelvic Organ Prolapse
If you have severe bladder prolapse, surgery may be required. During surgery, a mesh support is inserted into the vaginal wall and the bladderâs position is corrected. This can be performed under general, regional or local anesthesia. Talk with your doctor for more information on surgery options and if it is required to fix your prolapsed bladder.
What Is A Male Bladder Sling
A male bladder sling or male urethral sling is a surgical treatment for incontinence in men. It is common in stress incontinence but can improve the symptoms of other types.
After placing a male bladder sling, no manual skill or training is required. It works mechanically as a hammock that brings up the urethra and applies gentle pressure. Since it works by itself and does not have complex mechanical parts, patients usually have rapid results .
There are two male bladder sling options available at the moment. One of them is Boston Scientifics AdVance Male Sling System, and the other is Coloplasts Virtue sling. The former uses two arms to do the job, and the latter uses four arms. In the past, there was also a three-arm sling available, the Argus sling.
Don’t Miss: New Drug For Bladder Cancer