Increased Diversity Of Tcr Repertoire After Bacillus Calmetteguerin Treatment
Antigens released from tumor cell killing upon BCG treatment could expand and recruit effector and memory T cells leading to an overall increase in the diversity of TCR in the tissue microenvironment. TCR clonal proportion and clonal space homeostasis at pre and 3M post-BCG were then analyzed to further decipher the impact of BCG treatment on the diversity of TCR in the tumor microenvironment.
Figure 4 Enhanced TCR repertoire diversity after Bacillus Calmette-Guerin treatment. Clonal proportion of the top n clonotypes. Red bar represents the clonal proportion taken by the 10 most abundant clones. Clonal proportion taken by top 10 most abundant clone at Pre and 3M post-BCG time point . 1 on Y-axis represents 100% of the total TCR repertoire. Proportion of homeostasis space occupied by clonotypes classified as rare , small , medium , large , and hyperexpanded 1 on Y-axis represents the 100% of the total TCR repertoire. Proportion of occupied homeostatic space for pre versus 3M post-BCG time points as classified by rare, small, medium, large, and hyperexpanded clone size, respectively. Graphs show mean with standard deviation. *p< 0.05 by Mann-Whitney U test. Connecting lines showed two pairs of matched pre- and post-BCG samples.
Taken together, the above data showed significant increase in smaller TCR clones suggesting the expansion of newly induced and potentially tumor-reactive T cells post-BCG.
Bacillus Calmetteguerin Treatment Alters The Frequencies Of T And Nkt Subsets In Peripheral Blood
Figure 2 Altered frequencies in immune subsets in peripheral blood mononuclear cells after Bacillus Calmette-Guerin treatment. t-SNE maps showing four clusters significantly different at three time points using repeated measure ANOVA test. Left, representative dot plots for NKT cells colored by intensity of Granzyme B expression from patient 10. Right, line plot showing the frequencies of GB+NKT cells over total immune cells at three time points from all patients. Left, representative dot plots for GB expressing PD-1-TIM3+CD8+ T cells from patient 16. Right, line plot showing the frequencies of GB+PD-1-TIM3+CD8+ T cells over total immune cells at three time points from all patients. Left, representative dot plots for central memory CD4+ T cells from patient 16. Right, line plot showing the frequencies of CD4+CCR7+CD45RO+ T cells over CD4+ T cells at three time points from all patients. Left, representative dot plots for Treg cells from patient 02. Right, line plot showing the frequencies of Treg cells over total immune cells at three time points from all patients. BâE, connected line specifies samples from same patient at different time points. *adjusted p< 0.05 or not significant by non-parametric One-way ANOVA by Friedmanâs test followed by Dunnâs post-test for matched data points with complete set of three time points.
Transcriptomic Signature Of Post Bacillus Calmetteguerin
Figure 3 Post-Bacillus Calmette-Guerin treated tissues show upregulation in genes involved in multiple immune activation pathways. Heatmap showing all differentially expressed genes from matched tissues between Pre and 3M Post-BCG time points . Functional pathways annotated by DAVID pathway enrichment analysis of the genes enriched in Pre or 3M Post-BCG time points . Volcano plot showing DEGs in the Pre and 3M Post-BCG tissues. Genes enriched in Post-BCG time point are colored in blue while genes enriched in Pre time point are colored in red. Selected genes are highlighted. The orange line denotes the p value of 0.05. Representative dot plots showing CD8+CD27+ cells gated from CD3+CD56- T cells of isolated cells from tissues with low and high CXCL9 genes, respectively. Median value for CXCL9 genes was used as the cutoff point for dichotomisation into two groups. Proportion of CD27 expressing CD8 T cells from tissues with low CXCL9 group , and high CXCL9 group , respectively. Graph shows mean with standard deviation. *p< 0.05 by Mann-Whitney U test.
Don’t Miss: Can You Treat A Bladder Infection Without Antibiotics
Optimization Of The Use Of The Scarce Vials Of Bcg
As soon as BCG shortages began, different strategies were adopted at different levels, from improvements in BCG production to modifications of the recommended treatment.
Improving BCG Production
The production of BCG is not an easy matter. Due to the slow growth of the mycobacteria, any inaccuracy during the manufacturing process can lead to a large loss of time and money, as the BCG shortages have proven. For this reason, some researchers proposed optimizing BCG bulk production by modifying the growth in pellicles to the use of bioreactors or evaluating the possibility of extending the shelf life of the already manufactured BCG vials.
Regulatory Issues/Favorable Policies
Variations in Clinical Guidelines Recommendations
For intermediate-risk NMIBC patients
-
Intravesical chemotherapy must be used as a first-option treatment instead of BCG. Induction once a week for six to eight weeks plus a monthly maintenance schedule for one year.
-
For second-line treatment, a one-third dose of BCG instead of full-dose BCG can be used. In that case, different patients can be treated the same day clustered in groups of three to avoid BCG wastage.
-
Maintenance BCG can be omitted.
For high-risk NMIBC
When To See A Doctor
There are a few side effects that can be especially dangerous, so make sure to talk to your doctor if you notice that you:
- Have a severe skin rash
- Are wheezing or having difficulty breathing
- Are finding swallowing to be difficult
- Have a high fever that isnt lowered with Tylenol or other over-the-counter fever reducers
Don’t Miss: Botox Injection For Bladder Incontinence
Current Clinical Use Of Intravesical Bcg Therapy
At initial diagnosis, approximately 70% of bladder cancer patients are diagnosed with non-muscle invasive bladder cancer , which include tumor stages Ta , T1 , and carcinoma in situ . The remaining patients have muscle-invasive tumor , which usually requires radical cystectomy. In contrast, most visible NMIBC lesions can be removed by endoscopic surgery, i.e., transurethral resection . For complete resection, a second TUR within 6 weeks after the initial resection is advised for T1 tumor. One problem in the management of NMIBC is the high intravesical recurrence rates ranging from 30% to nearly 80%, depending on the risk profile. Several mechanisms for intravesical recurrence have been proposed including microscopic persistence of tumor, cancer cell implantation, and new tumor formation. More importantly, NMIBC may progress to muscle-invasive cancer during repeated episodes of intravesical recurrence. Urothelial CIS, unlike CIS in other organs, has high malignant potential. CIS has over 50% risk of progression to muscle-invasive cancer.
| Definition | |
|---|---|
| Any combination of T1 and/or G3 and/or CIS | TURBT+ intravesical BCG with induction and maintenance |
| Immediate radical cystectomy should be considered for high grade, multiple T1 tumors T1 tumors located at a site difficult to resect residual T1 tumors on resection high-grade tumors with CIS |
| Local |
|---|
| Pneumonitis |
Prospect Of Engineered Mycobacterium Vaccine
Intravesical BCG therapy is not free from treatment failure, and AEs include rare but possibly fatal complications. Therefore, major clinical efforts have been made to develop more active and less toxic modes of immunotherapy these include use of a combination of interferon, reduction of BCG dose, and prophylactic administration of tuberculostatic agents. Although some strategies show promising results, further clinical evaluation is needed.
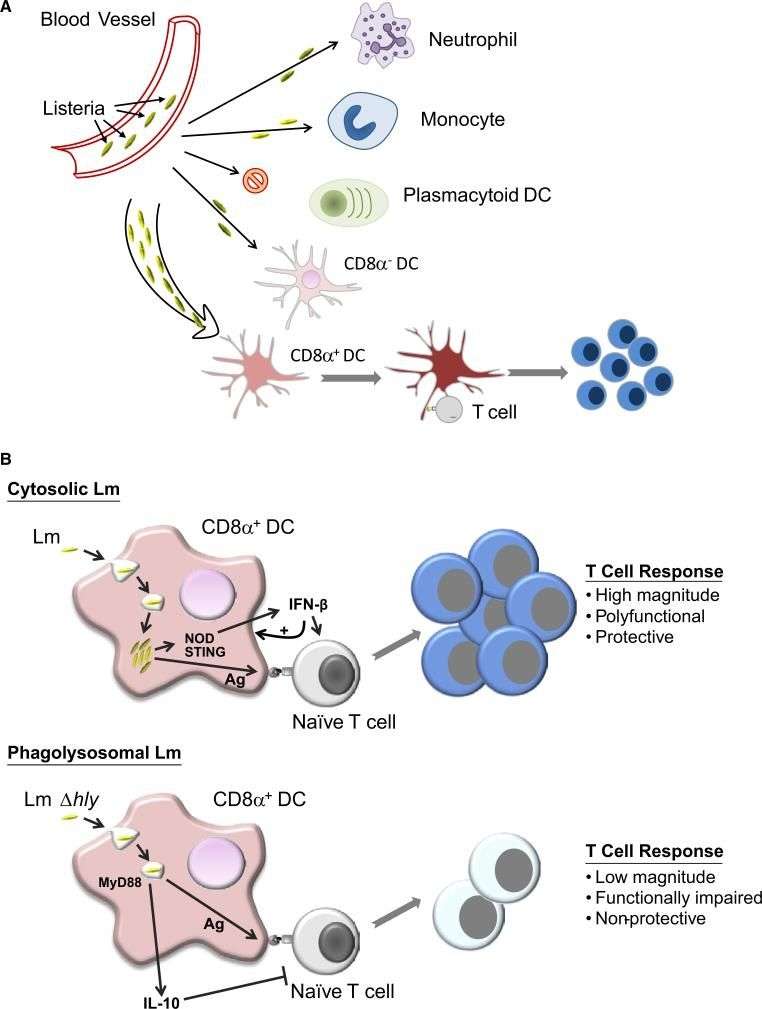
Based on recent increases in understanding of BCG-induced immune responses, a variety of preclinical studies have been conducted to overcome the limitations of BCG therapy. One approach is the generation of Th1 cytokine-expressing recombinant forms of BCG . In animal models, some cytokine-expressing rBCGs showed promising results against malignant melanoma and breast cancer however, studies using intravesical models of bladder cancer are still limited.
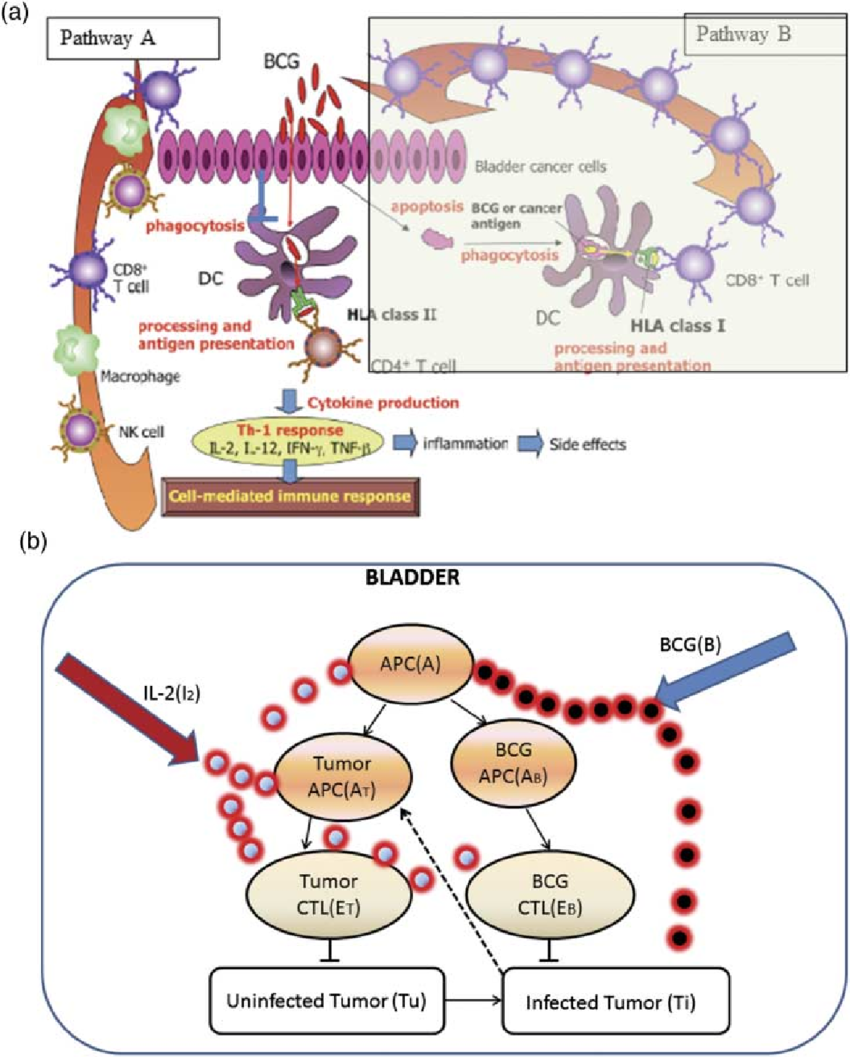
Figure 1
You May Like: Non Invasive Papillary Carcinoma Bladder
What To Know About Bcg For Bladder Cancer
Did you know May is Bladder Cancer Awareness Month? It’s a time to raise extra awareness and promote facts about this disease. Education and raising awareness about bladder cancer is an important part of moving closer to a cure.
If you or a loved one is diagnosed with bladder cancer it can be frightening. However, your doctor and medical team are there to help you.
Talk with your healthcare team about all the available forms of treatment. They will tell you about possible risks and the side effects of treatment on your quality of life.
Your options for treatment will depend on how much your cancer has grown. Your urologist will stage and grade your cancer and assess the best way to manage your care considering your risk. Treatment also depends on your general health and age. Visit our condition article to learn more about treatment options for bladder cancer.
Who Can Use Bcg
BCG is a treatment for early-stage bladder cancer that has not yet invaded the muscle of the bladder wall. Called non-muscle invasive bladder cancers or in situ bladder cancers, these account for about half of all bladder cancers.
For 2021, it was estimated that about 83,730 new cases of bladder cancer would be diagnosed in the United States, and about 17,200 American bladder cancer patients would die from the disease.
Also Check: What Is Best For Bladder Infection
Doing My Research About Bcg
This treatment along with other alternatives was explained to me by my urologist after two operations to remove tumors from the bladder. My medical team was confident that my cancer was contained within the bladder lining. So as a result of this feedback and doing my research on the effects of BCG I opted for this course of treatment. The BCG is given once a week for a period of six weeks through an outpatient department. The drug is delivered through a catheter into the bladder and is relatively painless and takes no longer than 2 minutes. I was told after each visit to go home after treatment to relax and not to pass urine for two hours after. This helps to increase the concentration and of effects of BCG in your bladder.
Different Strains Of Bcg
There are several different strains of BCG available. The more commonly used strains include the Tice strain produced by Organon Teknika, the RIVM strain produced by Bilthoven, and the Connaught strain produced by Connaught Laboratories. Morales used a strain of BCG which came from the Institut Armand Frappier in Montreal, in fact BCG-Connaught is derived from this strain.
As there are several commercially available strains of BCG, uncertainty exists in the literature about whether the various strains of BCG have identical immunotherapeutic efficacy and identical clinical effectiveness. Given this fact direct comparison between clinical studies is difficult when different strains of BCG have been used.
Read Also: Why Do I Get Recurring Bladder Infections
Induction Of Immune Responses
As shown in Table , various types of cytokines are detectable in the urine after BCG instillation. The cytokines in the urine indicate an immunological response specific for BCG instillation, although not completely. Most of the cytokines are detected after the second BCG instillation, and their concentrations increase after BCG instillations., Macrophages and activated lymphocytes are thought to be major sources of these cytokines. In contrast, some cytokines such as interleukin -1, IL-6, and IL-8 are detected after the first BCG instillation., Miyazaki et al. reported that cultured urothelial cells release IL-6 and IL-8 directly in response to BCG. Although this urothelial cell reaction is not specific to BCG, urothelial cells are supposed to be involved in the early phase of mucosal cytokine network induction by BCG. In addition to Th1 and Th2 cytokines, recently, several investigations showed that IL-17 plays a crucial role in generation of Th1-cell responses in BCG vaccination. At present, clinical data about IL-17 is limited, but in a mouse model, increases in IL-17 family genes and urinary IL-17 concentrations are reported. Recently, Takeuchi et al. reported that IL-17-producing T cells induced recruitment of neutrophils to the bladder.
Severe Pain And A Loss Of Appetite
My entire body literally shut down on me. I had major fever type symptoms, excruciating pain in all joints and a severe headache. I was unable to eat and just about managed to take on fluids over the two days. After discussions with my medical team who assured my wife it was a reaction to the BCG, I was admitted to hospital for a further three days unable to breathe properly, with severe kidney pains that could only be eased with morphine. A CT scan was taken that fortunately showed no abnormality in my kidneys, so I was eventually sent home with a course of antibiotics.
Don’t Miss: How Do Doctors Test For Bladder Infection
Immunological Hallmarks For Clinical Response To Bcg In Bladder Cancer
- 1Translational Immunology Institute , SingHealth-DukeNUS Academic Medical Centre, Singapore, Singapore
- 2Duke-NUS Medical School, Singapore, Singapore
- 3Division of Pathology, Singapore General Hospital, Singapore, Singapore
- 4Institute of Molecular Cell Biology , Agency of Science, Technology and Research , Singapore, Singapore
- 5Department of Urology, Singapore General Hospital, Singapore, Singapore
Bcg Failure And Subclassification
About 40% of patients of NMIBC will fail intravesical BCG treatment. Although many factors might lead to BCG failure, the dose of BCG and type of T helper response may lead to dramatically diverging outcomes. Low-dose BCG might not trigger enough TH1-type immune response, which is the main response to BCG activity. Too high doses of BCG may paradoxically activate mixed TH1/TH2 responses which will counterbalance the TH1 response . Other factors of BCG failure include occult micrometastatic disease prior to BCG therapy .
Patients who fail intravesical BCG treatment are usually sub-classified into three categories based on the type of failure:
BCG refractory, which is the persistence of disease after induction or maintenance BCG treatment.
BCG relapse, the recurrence of disease after a disease-free period post BCG treatment.
BCG intolerance when the patient is not tolerating the completion of BCG induction .
The definitions, endpoints and clinical trial designs for NMIBC as recommended by the International Bladder Cancer Group might serve as an excellent current state-of-the-art resource . The type of failure should be clearly defined. Because stakes are very high for these patients, for whom BCG has failed, and options are limited, single-arm designs may be relevant for the BCG-unresponsive population. The consensus for a clinically meaningful initial complete response rate or recurrence-free rate is of at least 50% at 6 months, 30% at 12 months and 25% at 18 months.
Read Also: Homemade Cat Food For Bladder Stones
Baseline Densities Of Cd4+foxp3
Figure 5 Higher baseline CD4+FOXP3- and CD8+PD-1+ T cells is predictive of response to Bacillus Calmette-Guerin treatment. Representative multiplexed immunofluorescence image of tissue area with an enlarged image for Pre-BCG tissues, showing staining of CD4 and FOXP3 , CD8 and PD-1 , for both responders and non-responders , respectively. Scale bar equals to 100 um. Quantification of baseline densities of total CD4+FOXP3+, CD4+FOXP3- CD8+PD-1+, and CD8+PD-1- T cells in R versus NR, respectively. ***p< 0.001, *p< 0.05 or not significant by two-tailed Mann-Whitney U test. RFS for patients with low versus high baseline densities of total CD4+FOXP3- and CD8+PD-1+ T cell. RFS for patients with baseline densities of low CD8+PD-1+ and low CD4+FOXP3- low CD8+PD-1+ and high CD4+FOXP3- high CD8+PD-1+ and low CD4+FOXP3- and high CD8+PD-1+ and high CD4+FOXP3- respectively. Low and high cell densities were < median versus > median. **p < 0.01 by Mantel-Cox log-rank test HR, Hazard Ratio. RFS represents recurrence-free survival .
Box : Prognostic Factors For Recurrence
-
Number of tumours more tumours mean more frequent recurrences.
-
Previous recurrence rate* or a recurrence at three months.
-
Size of the tumour those > 3 cm carry a worse prognosis.
-
Grade of anaplasia.
-
Presence of CIS.
*The recurrence rate being the number of positive cystoscopies per year over the number of cystoscopies performed per year.
For progression, tumour grade is the most important factor. It is also known that T1 tumours have a worse prognosis than Ta tumours. Using these factors patients with superficial bladder cancer can be divided into three groups: the lowest risk group with a single less than 3 cm Ta G1 tumour, and a recurrence rate of less than one tumour per year a high risk tumour of T1 G3, multifocal, large, highly recurrent, and CIS and other tumours of intermediate risk. Recent studies further confirm these criteria.
Don’t Miss: Is Pumpkin Seed Oil Good For Overactive Bladder
When Is Bcg Treatment Used
You may have BCG directly into your bladder after surgery to remove non-muscle-invasive bladder cancer. This type of surgery is called a transurethral resection of a bladder tumour .
This treatment helps prevent the cancer from coming back in the bladder lining. It also reduces the risk of the cancer becoming muscle-invasive. Doctors usually suggest this treatment if you have a high-risk bladder cancer, or sometimes if you have an intermediate-risk bladder cancer.
There is usually at least 2 weeks between the surgery to remove the cancer and the start of BCG treatment. This is to give your bladder enough time to heal from the surgery.
You usually have BCG treatment once a week for 6 weeks. This is sometimes called the induction course. You may be offered more BCG treatments. This is usually called maintenance treatment.
Treatment times vary. Your doctor will explain what is best for you.
Study Approval And Specimens
Five patients with NMIBC who underwent transurethral resection to remove all endoscopically visible tumors followed by BCG instillations in Singapore General Hospital were recruited upon informed consent according to guidelines from institutional review board . The patientsâ baseline clinicopathological parameters were analyzed . After two-four weeks, the patients received weekly intravesical BCG instillations for six times as standard protocol . Upon completion of the 6 doses instillations, surgical specimens were obtained to confirm that no neoplastic pathology of the mucosa by the pathologists. Tissue specimens were obtained from: pre-BCG resected tumor , pre-BCG adjacent non-tumor tissue and post-BCG NT urothelial tissue. Blood specimens were obtained before and two time points after BCG instillations at 1 month and 3 months . Two patients withdrew from the study and stopped BCG treatment before the last time point due to BCG toxicities/intolerance.
A small piece of pre- and post-BCG tissues were subjected to RNA sequencing analysis. Tissue-infiltrating leukocytes were isolated from pre- and post-BCG tissues with enzymatic digestion: 100μg/ml Collagenase IV and 100μg/ml DNase1 and peripheral blood mononuclear cells from blood using Ficoll-Paque layering, both as previously described . TILs were analyzed using flow cytometry and PBMCs were stored with 10% DMSO in liquid nitrogen until later analysis with CyTOF.
Recommended Reading: How To Strengthen Bladder Control Muscles