What To Do If You Have Both
If you are experiencing bowel and bladder symptoms, bring both to the attention of your healthcare provider. Because of the stigma regarding “bathroom symptoms,” many people are too shy to discuss their issues with their healthcare providers.
Don’t be embarrassed. Elimination is a normal part of being human, as your healthcare provider well knows. They will help find a diagnosis and provide you a plan to manage each problem.
Depending on your condition, you might also get a referral to a urologist, urogynecologist, or neurologist.
Based on your diagnosis, your doctor will tailor your treatment for the bladder problem you are experiencing. For example, if your problems are related to pelvic floor dysfunction, your doctor may recommend physical therapy or biofeedback.
If your symptoms appear to be related to visceral hypersensitivity, they may recommend a medication that targets the nervous system. This could be a medication to increase levels of the neurotransmitter serotonin or a medication with anticholinergic effects.
Causes Of Inflammation Of The Bladder
The urinary system of the body includes the kidneys, ureters, urethra, and bladder, all of which play a role in removing waste from the body. The bladder is a hollow organ situated in the lower abdomen that stores urine it expands when it is being filled, and contracts when urine is being passed. The walls of this sac-like organ become inflamed when an infection kicks in. Three common types of bladder infections that result in bladder inflammation are bacterial cystitis, noninfectious cystitis, and interstitial cystitis.
Uc Treatments And Urinary Changes
Sometimes, UC treatments can affect urinary habits. Corticosteroids such as prednisolone may cause urinary changes in people with UC. This medication usually causes someone to pee less, but it can also cause someone to pee more often.
Several members have noticed this effect. Has anybody ever experienced frequent, urgent urination whilst on prednisolone? asked one member. I am definitely peeing more often, but the urgency at which I need to get to the bathroom to have a pee is a bit worrying. Another member mentioned that they had experienced this effect. When I take prednisone or budesonide, I urinate much more frequently, which is a known side effect of steroids.
Using high doses of steroids or using steroids for a long time can sometimes lead to problems with the adrenal glands small organs that make hormones to regulate many body processes. Frequent urination can be a sign of this issue. Other symptoms include dizziness, a fast heart rate, irregular heartbeats, blurry vision, or feelings of weakness. Tell your doctor if you notice these symptoms while taking steroids.
Several other health conditions unrelated to UC could also lead to increased urination. They include:
- Prostate problems, including prostatitis or benign prostatic hyperplasia
- An overactive bladder
- Interstitial cystitis, also known as painful bladder syndrome
Taking diuretics also leads to increased urination. These medications are used to treat heart failure and certain kidney and liver problems.
Recommended Reading: Stage One Bladder Cancer Treatment
What Causes Bladder Or Bowel Incontinence
Many conditions may affect the nerves and muscles that control the bladder and bowel.
Bladder incontinence can be caused by things such as:
-
Damage to nerves in sphincter muscles
-
Holding urine in too long , which can damage the bladder
-
Having to urinate many times during day and night, often urgently
Bowel incontinence can be caused by things such as:
-
Damage to the nervous system from disease or injury
-
Vaginal childbirth
How To Prevent Urinary Problems In Ibs
There are also some steps that people with IBS can take to prevent urinary problems or stop them from becoming worse.
Kegel Exercises
One of the most effective methods for preventing urinary problems is strengthening the pelvic floor muscles. The best way to do this is to perform regular Kegel exercises. They involve tensing the muscles that stop the flow of urine and prevent you from passing gas.
It is possible to do Kegel exercises while standing, sitting, or lying down. However, it is important that the bladder is empty before starting.
- Relax in a comfortable position and take a few deep breaths.
- Tighten the pelvic floor muscles and hold for three to five seconds, then release.
- Relax for three to five seconds, and repeat.
- Perform 10 repetitions, three times a day.
Bladder Breaks and Training
Some other helpful techniques include scheduling bathroom breaks and bladder retraining. Holding on for a few extra minutes each time you need to urinate can help to increase bladder strength.
You May Like: Bladder Problems After Spinal Surgery
How To Manage Increased Urination With Ulcerative Colitis
| | | | | |
Ulcerative colitis is a type of inflammatory bowel disease in which the immune system damages the large intestine. People with UC may experience several symptoms, including needing to urinate more often than usual.
Some members of MyCrohnsAndColitisTeam have wondered about urinary symptoms. Do any of the people with UC experience frequent urination? asked one member. Been having lower pelvic pressure, bloating, and increased urination frequency. Anyone else experience this? wrote another.
Symptoms Of Urinary Problems In Ibs
The symptoms of urinary problems in IBS can vary slightly depending on the underlying cause:
- Overactive bladder syndrome: frequent need to urinate, needing to pee at night and urinary incontinence.
- Interstitial cystitis: frequent urination, bladder discomfort, painful urination.
- Chronic prostatitis: lower pelvic pain, frequent and urgent urination, painful urination, urinary incontinence.
Also Check: How To Stop A Bladder Infection From Getting Worse
Preventing Diverticular Disease And Diverticulitis
Eating a high-fibre diet may help prevent diverticular disease, and should improve your symptoms.
Your diet should be balanced and include at least 5 portions of fruit and vegetables a day, plus whole grains. Adults should aim to eat 18g to 30g of fibre a day, depending on their height and weight. Your GP can provide a more specific target, based on your individual height and weight.
It’s recommended that you gradually increase your fibre intake over the course of a few weeks. This will help prevent side effects associated with a high-fibre diet, such as bloating and flatulence . Drinking plenty of fluids will also help prevent side effects.
If you have established diverticular disease, it may be suggested that you avoid eating nuts, corn and seeds due to the possibility that they could block the diverticular openings and cause diverticulitis. People usually find out themselves if these foods cause symptoms. Probiotics have also been recommended, but evidence is lacking. Overall, there is a lack of good quality scientific evidence on how to prevent diverticular disease.
Causes Of Diverticular Disease And Diverticulitis
Diverticular disease is caused by small bulges in the large intestine developing and becoming inflamed. If any of the diverticula become infected, this leads to symptoms of diverticulitis.
The exact reason why diverticula develop is not known, but they are associated with not eating enough fibre.
Fibre makes your stools softer and larger, so less pressure is needed by your large intestine to push them out of your body.
The pressure of moving hard, small pieces of stools through your large intestine creates weak spots in the outside layer of muscle. This allows the inner layer to squeeze through these weak spots, creating the diverticula.
There is currently no clinical evidence to fully prove the link between fibre and diverticula. However, diverticular disease and diverticulitis are both much more common in Western countries, where many people do not eat enough fibre.
Read Also: How To Ease Bladder Discomfort
What Is Inflammatory Bowel Disease
Often confused with Irritable Bowel Syndrome , which is a separate and unpleasant condition in its own right, it is considerably less severe and difficult to manage than IBD. Whether toilet humour which so often accompanies both is ever in good taste is a matter of personal preference, but here it detracts from the very serious nature of the condition.
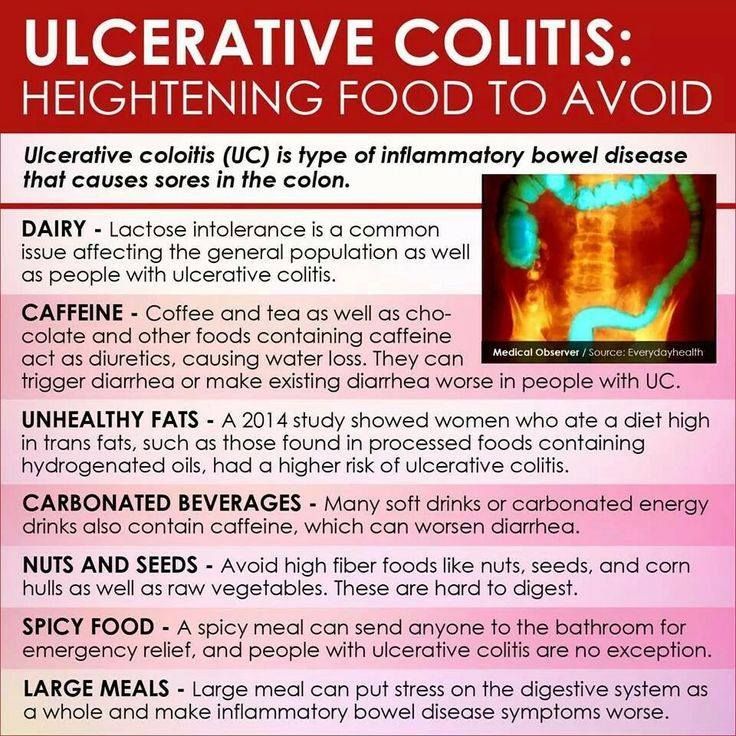
IBD does include some of the same symptoms as IBS , but on top of that, patients can typically suffer from extreme fatigue, joint pain, eye inflammation, rectal bleeding, intestinal scarring, malnutrition and severe weight loss. These are not symptoms that can be taken lightly, and are hardly conducive to a normal lifestyle. As a digestive disease, IBD also requires a strict diet, avoiding fried and fatty foods, as well as caffeinated drinks.
Around 10 million people around the world are currently living with IBD, and the National Center for Biotechnology Information reports that these numbers are on the rise. It is widely accepted that there are many more living with IBD without a medical diagnosis. Due to the unpredictable character of the disease, and complicated nature of treatment, it is notoriously expensive to treat, costing the USA an estimated $2.2 billion a year.
What Causes These Issues
Bladder-related issues may be caused by a variety of different factors including underlying conditions such as infections , cystitis , bladder cancer, or endometriosis. In addition, bladder-related issues may be caused by the natural aging process, pregnancy, or childbirth, as well as a result of another treatment regimen such as radiation or surgery on or around the bladder.1,2
Bowel-related symptoms have some similar causes, including being the result of another treatment procedure or due to the natural aging process. Several conditions may also contribute to the development of bowel-related problems, including irritable bowel syndrome , inflammatory bowel diseases such as Crohn’s disease or ulcerative colitis, celiac disease, endometriosis, and diverticulitis.3,5
It’s also possible that bladder or bowel issues may not be a direct result of endometriosis lesions affecting those organs, but rather, the overlapping of endometriosis with another bowel or bladder-affecting condition such as IBS. Some bladder and bowel-related conditions share similar risk factors with endometriosis, including genetics, family history, inflammation-related issues, and potential immune-system defects. These shared risk factors may contribute to an increase in risk of developing both conditions separately from one another.
Don’t Miss: Lemon Water For Bladder Infection
What Can I Do At Home To Relieve My Ibd Symptoms
Your doctor will talk to you about steps you can take at home to relieve your IBD symptoms. Some steps may include:
- Reducing stress. Stress does not cause IBD, but it can make your IBD symptoms worse. Some studies show that mindfulness therapy, hypnotherapy, and psychotherapy may help.18Get tips on relieving stress.
- Changing your eating habits. Some women report that limiting or avoiding certain foods helps relieve symptoms.19
- Taking vitamin supplements. Your doctor may suggest vitamin supplements if your body does not get all of the nutrients you need from food because of IBD. You may need to take vitamin B12, folic acid, vitamin D, calcium, or iron.
- Taking probiotics. Some research suggests that probiotics, which are live bacteria similar to what is found naturally in the body, may help some people with IBD.20 Probiotics are in foods such as yogurt that indicate there are “live and active cultures” on the label. Probiotics also come as a supplement you can buy in many stores. Vitamins and supplements are not regulated by the Food and Drug Administration in the same way as medicines. Talk to your doctor or nurse about any supplements you take, including probiotics.
Changes In Bladder Voiding Parameters
As an immediate comparison with the clinical symptoms of OAB and IC/PBS, there have been a number of well-documented studies into the effects of transient colitis on bladder voiding. During the acute phase of trinitrobenzesulfonic acid -induced colitis in rodents, when colonic inflammation is pronounced, there are consistent changes in bladder voiding parameters. This includes deceased micturition intervals, decreased voided volumes, and decreased bladder capacity, as well as increased micturition frequency . By 7 days post-TNBS administration, colonic inflammation has begun to spontaneously resolve, with a corresponding increase in the integrity of the colonic wall. By 28 days post-TNBS, there are no observable histological changes in the colon compared with healthy control mice . However, changes in bladder micturition parameters remain altered at 10 and 12 days post-TNBS and may persist long term . Accordingly, these studies indicate that transient experimental colitis can have profound acute and long-term effects on bladder function following resolution of the initial inflammatory stimuli. This provides us with the closest possible analogy to the symptoms of urgency, urge incontinence, and frequency observed in humans with OAB and IC/PBS .
Table 1. Reported changes in bladder function in response to experimental colitis
Recommended Reading: Do You Need Antibiotics For Bladder Infection
Can Overactive Bladder Cause Constipation
According to a 2016 study, some aspects of OAB can lead to constipation.
Additionally, if you have urinary urgency, you might delay trips to the bathroom. In doing so, you may hold in bowel movements, which increases the risk of dried stool and constipation.
In some cases, OAB can indirectly cause constipation. If you have urinary urgency, you might be prescribed medication that relaxes your bladder muscle. This medication can also relax the gut, resulting in slow-moving stool and constipation.
Some people are more likely to experience constipation and overactive bladder.
This includes:
Clinical Evidence Of Cross
Gastrointestinal disorders can be generally defined as being either organic or functional on the basis of their perceived underlying etiology. For instance, IBD, which includes both Crohns disease and ulcerative colitis, is an organic digestive disease. IBD is characterized by chronic remitting and relapsing inflammation of the intestine , resulting in abdominal pain, diarrhea, gastrointestinal bleeding, and malnutrition in ~0.5% of the Western population . Although the etiology of IBD is unknown, it is generally acknowledged that IBD development occurs through an exaggerated or inadequately suppressed immune response to luminal antigens, probably derived from intestinal microbiota, in genetically susceptible individuals . In contrast, IBS is a prevalent chronic functional gastrointestinal disorder that affects ~11% of the global population . While IBS is characterized by abdominal pain or discomfort associated with altered bowel habit , it differs from IBD in that these symptoms present in the absence of overt intestinal inflammation. Persistent neuroplasticity of the sensory afferent pathways innervating the colon contribute to these symptoms in the absence of inflammation and may arise following acute bouts of intestinal inflammation that resolve . This neuroplasticity may also be the result of low-grade inflammation not identified during routine clinical screening .
Read Also: Why Do I Have Bladder Leakage
Database And Study Population
This study was approved under University of Mississippi Medical Center IRB #2019-0194 for retrospective analysis of 3272 identified charts of individuals with either UC or CD. This study was designed using a retrospective cohort model. The data was collected by IRB-approved researchers from 2012 to 2019 from a research data base that recorded data from 6 integrated facilities associated with one tertiary healthcare center based around Jackson, Mississippi. The study data was collected from EPIC, de-identified, and managed using Research Electronic Data Capture tools hosted at UMMC .
Granulomatous Salpingitis And Oophoritis
In rare instances, Crohn’s disease is a cause of granulomatous lesions involving the fallopian tubes or the ovaries, usually by direct extension of the inflammatory process from the bowel.14 These lesions commonly present with unilateral pelvic pain or a pelvic mass, and may masquerade as pelvic inflammatory disease, endometriosis, active intestinal inflammation, appendicitis, diverticulitis or primary ovarian pathology. The diagnosis of Crohn’s disease should be considered when a patient presents with an adnexal mass. Computed tomographic scanning with oral contrast medium will demonstrate a thickened abnormal ileum, and barium contrast studies will document primary bowel pathology. Extensive adnexal disease may also impair fertility.
You May Like: Cream Of Tartar For Bladder Infection
How Does Ibd Affect Pregnancy
IBD can affect your chances of getting pregnant and your symptoms during pregnancy. Pregnant women with IBD may have a high-risk pregnancy.
- Before you get pregnant: You may have more trouble getting pregnant during a flare-up . Also, if you have IBD, talk to your doctor about your risk of problems during pregnancy. If you have a flare-up during pregnancy, you have a slightly higher risk of premature birth, low birth weight, and cesarean delivery than women who do not have IBD.30
Your doctor may also change the type or amount of the medicine you take. Some medicines, such as methotrexate and thalidomide, cause birth defects and other health problems and should not be taken while you are pregnant or breastfeeding.31 If you might become pregnant, talk to your doctor about any medicines you take.
- During pregnancy: Some women say their symptoms get better during pregnancy, but others say they get worse. Women whose IBD is in remission before getting pregnant are more likely to stay symptom-free during pregnancy.31
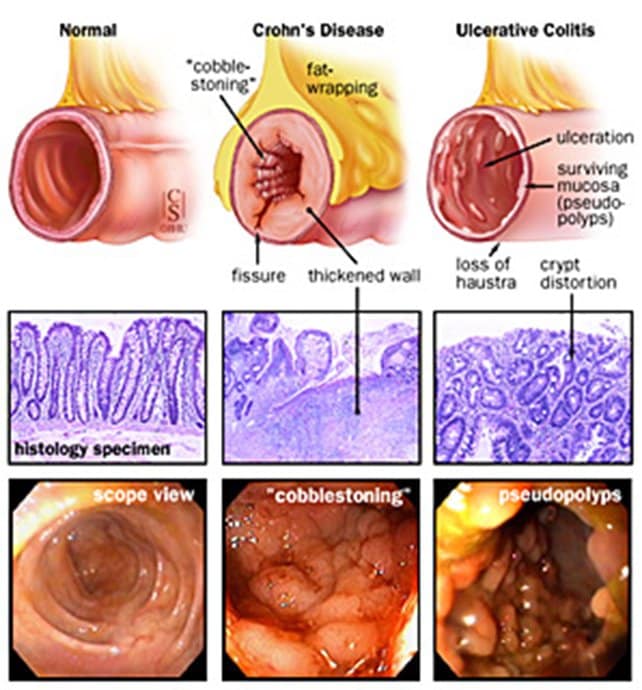
Crohns Vs Ulcerative Colitis
Crohnâs disease is often confused with another condition called ulcerative colitis. The symptoms are similar, and both involve periods of active flare-ups, followed by times when you donât have symptoms, which is called remission.
The only way to find out if you have Crohnâs or ulcerative colitis is to see your doctor for tests.
You May Like: Can A Bladder Infection Cause Lower Back Pain
How Are Bladder And Bowel Issues Evaluated
Evaluating bladder and bowel problems, especially if their underlying source is endometriosis, may be particularly challenging since many similarly presenting conditions have the ability to cause these issues. As an example of this potential difficulty, an individual may go to their general practitioner with a complaint of pain while urinating or defecating. Their primary care doctor may then send them to a gastroenterologist to determine what could be impacting their bowel function, as well as to a urologist to look at their bladder. These specialists may speculate a bowel or bladder-only related condition, and not consider endometriosis. It may take a long time for other non-endometriosis causes to be ruled out, which may not even occur until the individual starts experiencing other symptoms that might bring them to their OB-GYN, who then might suspect endometriosis.4
Conversely, if an individual is having pelvic pain and difficulty while defecating, they may be sent directly to an OB-GYN, but have a gastrointestinal-related condition rather than endometriosis. Since all of these conditions are very similar and are sometimes treated or investigated in different ways, it may take some time for all of the pieces to come together.