Addition Information About Vaginal Surgery When A Synthetic Or Biologic Graft Is Used
In Australia, in January 2018 the TGA withdrew approval for the used of synthetic and biologic mesh for trans-vaginal prolapse repair. The TGA continues to approve synthetic and biological mesh for prolapse when placed using laparoscopy, robot assisted and through an abdominal incision.
In the USA, the Food and Drug Administration has issued the following safety communication regarding the use of mesh.
The FDA wants to inform you about the complications that can occur when surgical mesh is used to treat Pelvic Organ Prolapse and Stress Urinary Incontinence , and provide you with questions to ask your surgeon before having these procedures. This is part of our commitment to keep healthcare professionals and the public informed about the medical products we regulate.
FDA has received reports of complications associated with the placement of mesh through an incision made in the wall of the vagina. Although rare, these complications can have serious consequences. The reports have not been linked to a single brand or model of mesh.
The most frequent complications included erosion through the vagina, infection, pain, urinary problems and recurrence of the prolapse and/or incontinence.
Background
Pelvic organ prolapse can cause pain or problems with bowel and bladder functions or interfere with sexual activity.
Stress urinary incontinence is a type of incontinence caused by leakage of urine during moments of physical stress.
Talking to your doctor
What You Need To Know
- Vaginal prolapse, also known as vaginal vault prolapse, occurs when the top of the vagina weakens and collapses into the vaginal canal. In more serious cases of vaginal prolapse, the top of the vagina may bulge outside the vaginal opening.
- Symptoms of vaginal prolapse include the feeling of vaginal pressure or fullness like youre sitting on a small ball and the sensation that something has fallen out of your vagina.
- A cystocele or rectocele usually occurs with vaginal prolapse.
- Mild cases of vaginal prolapse do not require treatment. Moderate to severe symptoms require nonsurgical therapies or minimally invasive surgeries, such as vaginal prolapse repair.
Overactive Bladder Problems After Hysterectomy
Sometimes nerve damage or infections are the reason for an overactive bladder after surgery. This crazy, unstoppable feeling of having to go to the toilet, even if you have little or no urine in the bladder, is due to the bladders detrusor muscle malfunctioning. After a hysterectomy, overactive bladder problems include frequent visits to the bathroom, even during the night , and leaking urine.
What can you do about it?
Strengthen the pelvic muscles with Kegel exercises. Avoid substances that will irritate the bladder like coffee, alcohol, carbonated drinks, and spicy meals. Get rid of the extra pounds, as your extra weight can have a notable impact on the pelvic floor muscles that support your bladder. There are several medications that can help to relax the Detrusor muscle. Common side effects of these medications are dry mouth, constipation, and sometimes confusion.
Read more in our post: 5 Effective home remedies for overactive bladder
Read Also: What Can You Take For Bladder Pain
Treating Pelvic Organ Prolapse
There are several treatment options available for a pelvic organ prolapse, depending on your circumstances.
The treatment most suitable for you depends on:
- the severity of your symptoms
- the severity of the prolapse
- your age and health
- whether you’re planning to have children in the future
You may not need any treatment if your prolapse is mild to moderate and not causing any pain or discomfort.
The various treatments for pelvic organ prolapse are outlined below.
What You Can Do For Vaginal Prolapse
They make devices called pessaries, which one can insert into the vagina and serve to keep the pelvic structures in their proper position. Avoiding strenuous lifting can help prevent and treat prolapse.
You can also do pelvic floor exercises, called Kegel exercises. These are simple exercises your doctor can teach you that will strengthen the pelvic floor muscles so that the supporting muscles will better hold up the pelvic structures. It can take several months of daily Kegel exercises to see an effect on urinary incontinence.
I can recommend The Bathroom Key , a book that presents an 8 to 12-week program with specific exercises to strengthen the pelvic floor muscles and that will help you to regain bladder control. It provides step by step instructions on how you can cure urinary incontinence without resorting to medication or surgery
If the prolapse after hysterectomy is severe, often surgery is the only real option, depending on how much the tissues affect you. With surgery, they aim to reconstruct the pelvic floor and to bring back the pelvic organs in their original position.
Recommended Reading: How Can I Treat A Bladder Infection At Home
Can I Develop Prolapse After A Hysterectomy
For women suffering from uterine prolapse, hysterectomies have found a place in medicine as a viable surgical treatment. But while this procedure can greatly improve quality of life, some studies suggest that it may also increase the risk of post-hysterectomy prolapse.
Because a hysterectomy removes part or all of the uterus, other pelvic organs that rely on the uterus to secure their positioning within the body may begin to fall out of place. While bladder prolapse is the most common form in general, women who suffer from post-hysterectomy prolapse are at a greater risk of apical prolapse, such as vaginal vault prolapse . The reason for this is that the vagina is connected to the uterus, and after removing the uterus during surgery, the apex of the vagina is no longer naturally attached within the body and therefore must be reattached to healthy ligaments that were not removed during surgery.
Depending on the type of hysterectomy procedure that is chosen, surgical steps taken by the operating physician to prevent future vaginal vault prolapse may not have lasting results. Its worth noting that some physicians claim that more invasive open abdominal or vaginal hysterectomies may result in removing ligaments that are essential for securing the vagina, while laparoscopic hysterectomies do not have this unwanted side effect.
How To Treat Bladder Prolapse
Women who have mild bladder prolapse without symptoms usually dont require treatment. The doctor may advise regular follow-up and conservative measures such as exercises to strengthen the pelvic muscles and prevent worsening. You do not need to treat your prolapse if it is not causing distress.
Treatment options for bladder prolapse depend on the grade of the condition. A combination of medical treatment and exercises to strengthen the pelvic floor muscles, and lifestyle modifications may be needed.
Treatment options include:
- Behavioral techniques:
- Fluid and diet management: This includes reducing or avoiding alcohol, caffeine or acidic foods, and fluid consumption.
- Bladder training: This includes training the bladder to delay urination after having the urge to urinate. The patient could start by trying to hold off going to the bathroom for 10 minutes every time theres an urge to urinate and gradually lengthening the time between going to the bathroom.
- Double voiding: This means to urinate and then waiting to urinate again after a few minutes.
Recommended Reading: Pictures Of Bladder Cancer Tumors
Apical Prolapse Or Uterine Prolapse
If a woman has had a hysterectomy, the top part of the vagina can become detached from the ligaments and muscles of the pelvic floor. Often, uterine or vault prolapse is associated with loss of anterior or posterior vaginal wall support. When the cervix protrudes outside the vagina, it can develop ulcers from rubbing on underwear. Sometimes these ulcers will bleed if they become irritated. Most women experience symptoms of bulge or pressure sensation in the pelvis.
Treatment For Asymptomatic Bladder Prolapse
If you have no symptoms of bladder prolapse, you may not need treatment. This may be the case with stage 1 or stage 2 prolapse. In fact, you may not be aware of the bladder prolapse at all. It may be picked up by your GP during a routine examination, such as during a cervical screening test.
Lifestyle changes and physiotherapy are the key aspects of managing such cases. There are things you can do to help prevent the condition from getting worse, which may include:
- weight loss
- correction of position when sitting on the toilet
- avoiding heavy lifting
- pelvic floor exercises, which have been proven to reduce the symptoms of an early stage bladder prolapse and prevent any worsening
- seeking treatment and management for chronic cough and lung disease.
Seeing a pelvic floor physiotherapist is always recommended so that they can assess your pelvic floor function properly and show you the correct technique for doing pelvic floor exercises. The best published evidence supports supervised pelvic floor muscle exercises for the management of prolapse and urinary incontinence.
Also Check: Antibiotics For Bladder And Kidney Infection
How Is Vaginal Prolapse Treated
Treatment for vaginal prolapse varies, depending on the severity of the symptoms. Many cases will not require treatment. In mild cases, your physician may recommend pelvic floor exercises to strengthen the muscles. In moderate cases, your doctor may insert a vaginal pessary to support your vaginal wall. In the most severe cases, you may benefit from surgery, such as colposuspension, a minimally invasive surgical procedure, where the vaginal wall is attached to a stable ligament in the pelvis.
Avoid Lifting Heavy Objects And Certain Exercises
Any activities that place a strain on your pelvic floor also increase your chances of developing pelvic organ prolapse after a hysterectomy. Not only should lifting heavy objects be avoided, but any exercises designed to strengthen your core muscles such as sit-ups, crunches, leg raises, and plank exercises should be practiced with caution.
Read Also: How Does Overactive Bladder Medication Work
Causes Of Pelvic Organ Prolapse
Pelvic organ prolapse happens when the group of muscles and tissues that normally support the pelvic organs, called the pelvic floor, becomes weakened and cannot hold the organs in place firmly.
A number of things can weaken your pelvic floor and increase your chance of developing pelvic organ prolapse.
These include:
- pregnancy and childbirth especially if you had a long, difficult birth, or if you gave birth to a large baby or multiple babies
- getting older and going through the menopause
- being overweight
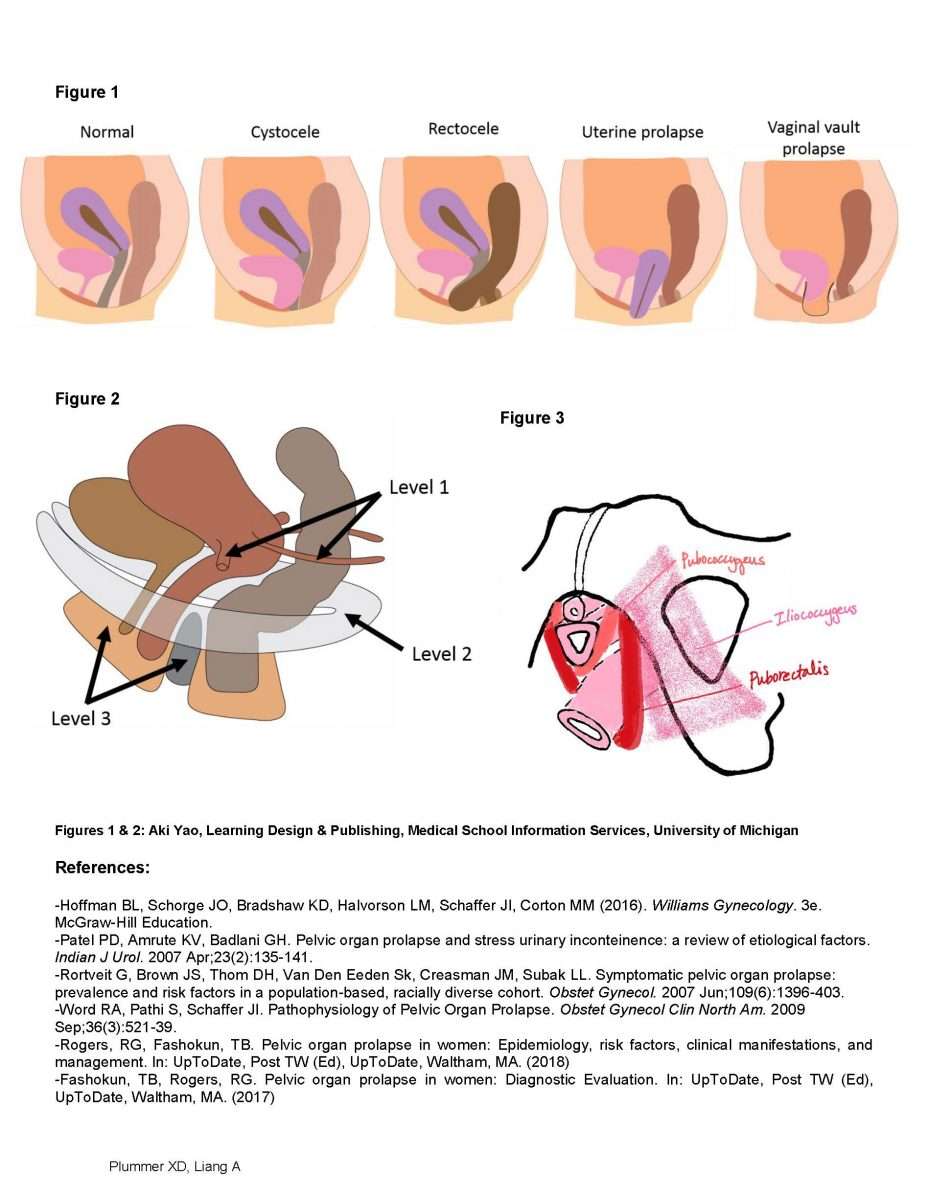
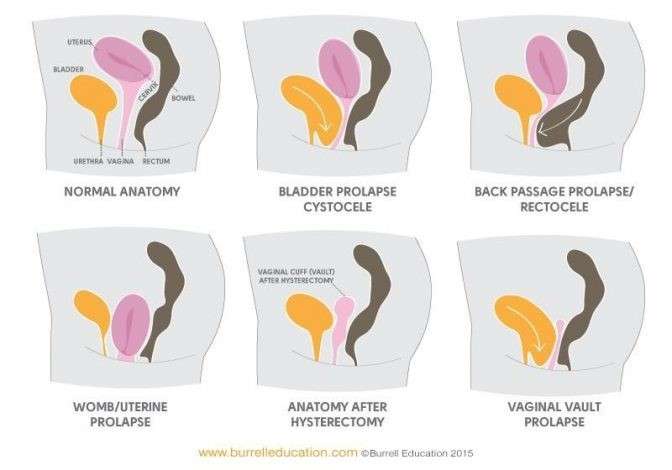
The 4 main types of prolapse are:
- the bladder bulging into the front wall of the vagina
- the womb bulging or hanging down into the vagina
- the top of the vagina sagging down this happens to some women after they have had surgery to remove their womb
- the bowel bulging forward into the back wall of the vagina
It’s possible to have more than 1 of these at the same time.
Pelvic organ prolapse will usually be classified on a scale of 1 to 4 to show how severe it is, with 4 being a severe prolapse.
Page last reviewed: 24 March 2021 Next review due: 24 March 2024
Causes Of Prolapse After Hysterectomy
Normally, there are muscles and ligaments in the pelvic floor that support the organs of the pelvis. When the pelvic muscles become weak, gravity takes hold and the organs fall through the weakest spot, which, in this case, is the vagina. There are supporting ligaments as well that can stretch and can fail to suspend the pelvic structures in their proper position and the structures fall.
Things that can contribute to having a vaginal vault prolapse or other types of prolapse into the vagina include the following:
- Giving birth. The more times a woman gives birth, the more the vagina gets stretched and the greater is the degree of laxity in the pelvic floor muscles and ligaments. Traumatic births and prolonged pushing are two other reasons.
- Lack of estrogen. This can occur after surgical or natural menopause. You need estrogen to keep the ligaments and muscles strong.
- Having a hysterectomy. The uterus normally holds the ligaments that keep the pelvic organs in its place. When they remove the uterus, they can damage the ligaments, making way for other pelvic organs to fall into the vagina. Vaginal vault prolapse after hysterectomy may also happen when the structures that hold up the top of the vagina are not reattached during the hysterectomy surgery or because these structures weakening over time.
Also Check: Best Thing For Bladder Infection
Bladder Function After Hysterectomy
A number of studies have shown no short-term urinary adverse effects of hysterectomy. However, longer-term follow-up shows an increased risk. This large Swedish study over a 31 year period showed a 2.4-fold risk of urinary stress incontinence surgery in women who had hysterectomies for benign conditions. This Danish study of women aged 40 to 60 years also showed a 2.4-fold risk of stress incontinence in women who had a hysterectomy. A small China study showed a 7.6% rate of pelvic organ prolapse and 67.4% rate of urinary incontinence 6 years post total hysterectomy.
A systematic review of 12 MEDLINE articles that used original data published over a 32 year period âwas consistent with increased odds for incontinence in women with hysterectomyâ¦.Among women who were 60 years or older, summary odds ratio for urinary incontinence was increased by 60% but odds were not increased for women younger than 60 years.â Another review of this same data consistently found an increased risk of incontinence many years after hysterectomy. However, this study also concluded that âOral estrogen replacement therapy seems to have little short-term clinical benefit in regard to incontinence and is associated consistently with increased risk of incontinence in women aged 60 years and older in epidemiologic studies.â
What Are The Most Common Side Effects Of A Hysterectomy
Some of the most common side effects of a hysterectomy are vaginal drainage and irritation at the incision sites.
If your ovaries were removed at the time of your hysterectomy, you may experience menopausal symptoms such as:
Your doctor will discuss treatment options to avoid the side effects of menopause mentioned above.
Don’t Miss: How Do I Cure A Bladder Infection
How Can I Treat Prolapse After A Hysterectomy
If you find that your post-hysterectomy prolapse is progressively getting worse even with lifestyle changes, then its time to consult with your physician about appropriate treatment options depending on the stage of prolapse.
For women who suffered from prolapse prior to having a hysterectomy, these treatment options are likely already known, but for those whose first occurrence of prolapse happens after a hysterectomy, here are the three most common options.
Treatments For Post Hysterectomy Vaginal Vault Prolapse
Treatment options will likely vary depending on the severity of the prolapse. Your treatment plan may also depend on factors such as your age, your sexual activity and your general health. Some nonsurgical treatment options include:
- Exercising the pelvic muscles
- Insertion of a vaginal pessary to provide support
If surgery is deemed necessary, options include:
- Sacrocolpopexy A piece of mesh is used to attach the vaginal vault to the tailbone.
- Vaginal vault suspension The vagina is attached to ligaments inside the pelvis.
- Colpocliesis The vagina is stitched shut to limit the chances of another prolapse. Tampa General Hospital treats a variety of female urology problems, including post hysterectomy vaginal vault prolapse.
Read Also: Interstim Implant For Bladder Control
Vaginal Hysterectomy For Prolapse
Prolapse is the loss of normal support of the vagina and/or uterus . Prolapse of the uterus and/or vaginal walls is a common condition with up to 11% of women requiring surgery during their lifetime. Prolapse generally occurs due to damage to the supporting structures of the uterus or vagina. Weakening of the supports can occur during childbirth, following chronic heavy lifting or straining , chronic cough, obesity, and as part of the aging process. In some cases, there may be a genetic weakness of the supportive tissues.
Prolapse of the uterus can cause an uncomfortable bulging sensation, a feeling of fullness, or pressure in the vagina. In more advanced prolapse the cervix can extend beyond the entrance to the vagina.
Normal uterus and vagina, no prolapse , and Prolapse of the uterus, bladder, and rectum
This is a procedure in which the uterus is surgically removed through the vagina. The operation is frequently combined with prolapse repairs of the bladder and/or bowel. There are no abdominal or laparoscopic incisions.
Appearance after hysterectomy
A vaginal hysterectomy offers many benefits over abdominal or laparoscopic procedures. It offers overall fewer complications, shorter healing time, less pain, less scarring, a lower chance of infection, less risk of hernias, and faster return to activities. Also, a prolapsed uterus is easier to access via the vagina.
With any operation there is always a risk of complications:
As Pop Worsens You May Notice:
- A bulging, pressure or heavy sensation in the vagina that worsens by the end of the day or during bowel movements
- The feeling of “sitting on a ball”
- Needing to push stool out of the rectum by placing fingers into or around the vagina during a bowel movement
- Difficulty starting to urinate or a weak or spraying stream of urine
- Urinary frequency or the sensation that you are unable to empty the bladder well
- Lower back discomfort
- The need to lift up the bulging vagina or uterus to start urination
- Urinary leakage with intercourse. Though unusual, severe prolapse can block the flow of urine and cause recurrent urinary tract infections or even kidney damage.
Also Check: What Antibiotics Treat Uti And Bladder Infections
Medications For Prolapsed Bladder
Estrogen replacement therapy may be used for a prolapsed bladder to help the body strengthen the tissues in and around the vagina. Estrogen replacement therapy can’t be used by everyone . Womenâs bodies stop creating as much estrogen naturally after menopause, and the muscles of the vagina may weaken as a result. In mild cases of prolapsed bladder, estrogen may be prescribed in an attempt to reverse bladder prolapse symptoms, such as vaginal weakening and incontinence. For more severe degrees of prolapse, estrogen replacement therapy may be used along with other types of treatment.Estrogen can be administered orally as a pill or topically as a patch or cream. The cream has very little systemic absorption and has a potent effect locally where it is applied. Topical administration has less risk than the oral preparations. The application of estrogens to the anterior vagina and urethral area may be very helpful in alleviating urinary symptoms, such as urgency and frequency, even in the face of prolapsed bladder.