Sacral Nerve Stimulation Therapy
Sacral nerve stimulation is a treatment in which mild electrical impulses are sent to the sacral nerves near the lower back. A device — implanted in the upper buttocks under the skin — is used to provide electrical pulses that influence bladder function. The procedure to implant the device does involve surgery, but it is minimally invasive, and reversible.
What Are The Specific Symptoms Of Overactive Bladder
Overactive bladder represents a collection of symptoms that can include:
- Urinary urgency: This is a failure to be able to postpone the need to urinate. When you feel you need to urinate, you have a limited amount of time to get to a bathroom.
- Frequency of urination: People who experience this symptom need to urinate very often. Typically its an increase in the number of times you urinate compared to what you previously experienced.
- Urge incontinence: In this case, there can be a leakage of urine when you get the urge to urinate.
- Nocturia: This symptom is characterized by the need to get up and urinate at least two times each night.
Behavioral Modification For The Treatment Of Overactive Bladder
Various types of behavioral modifications may also be recommended for the treatment of overactive bladder. Examples include:
- Dietary Changes: Decreasing water consumption throughout the day can help reduce leakage, as can avoiding substances that irritate the bladder, such as caffeine, fruit juices, and spicy foods.
- Bladder Retraining: This method uses a set schedule for urination throughout the day. Between these times, no urination is allowed, even if leaks occur. The goal is to increase the time between bathroom visits to three to four hours.
- Electrical Stimulation and Biofeedback: This technique provides information about when a patient is squeezing the muscles of her pelvic floor. A sensor is placed in the vagina or anus so that pelvic floor muscle contractions can be recorded. Exercises can help strengthen weak pelvic floor muscles, and if they don’t respond, electrical stimulation can activate the appropriate muscles.
Also Check: Bladder Cancer After Prostate Radiation
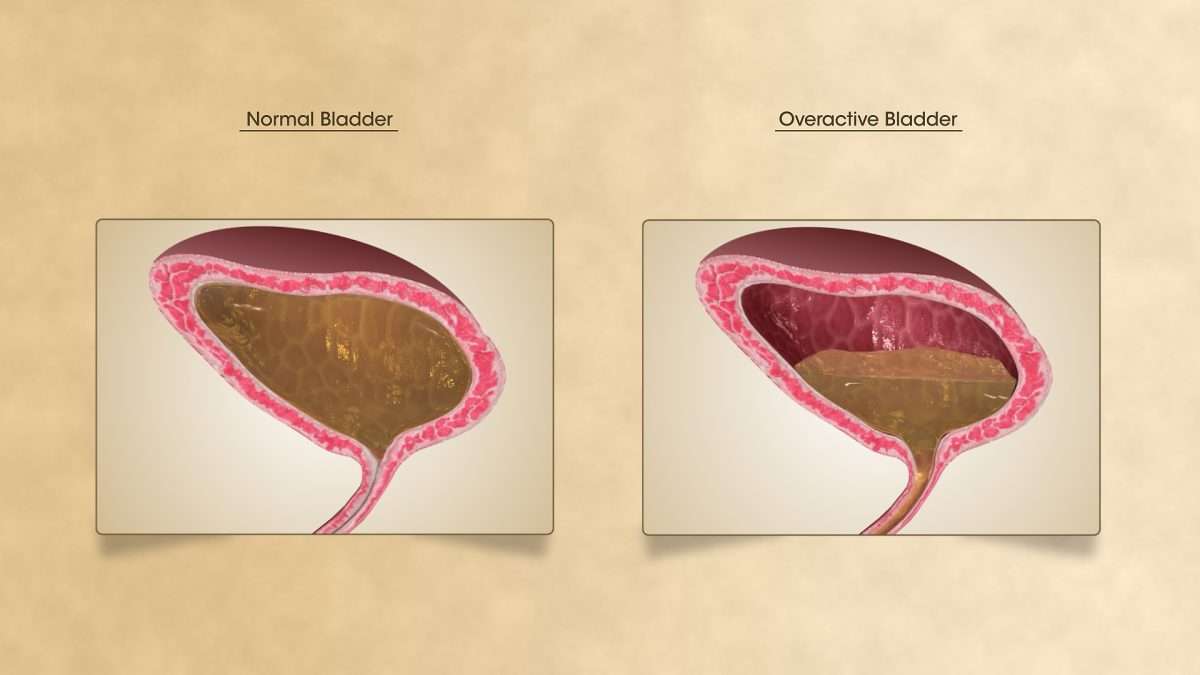
What Is Overactive Bladder
Overactive bladder is, simply put, a frequent urge to urinate that can come on unexpectedly, and be hard to control. If you have OAB, you may get up a lot at night to urinate, and might need to go often during the day as well. Urinary incontinence can also be an unwanted side effect of OAB.
If you urinate more than twice at night or at least eight times in the day, you may have OAB.
What Happens With Botox Treatment
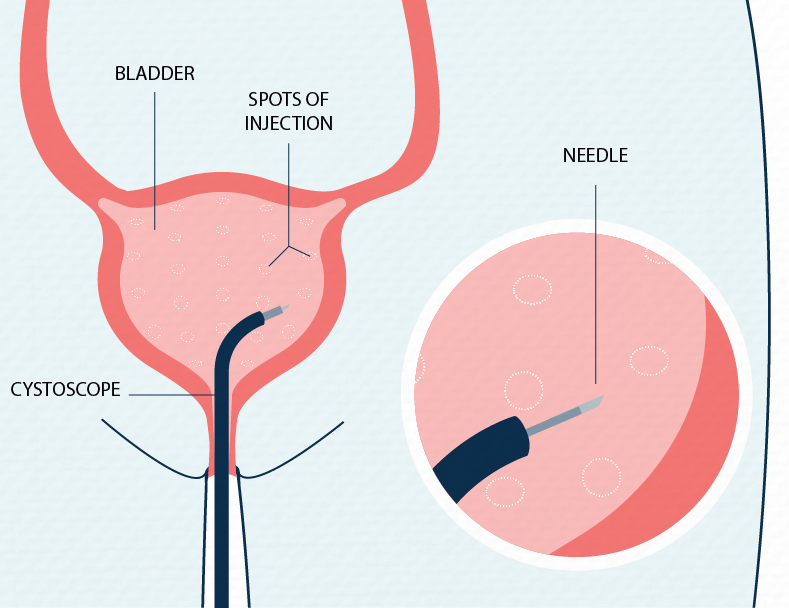
Its a very quick treatment. Botox is injected into your bladder, which helps the muscles relax. The injection doesnt hurt a lot, but you may feel a bit of discomfort. The doctor will keep you for 30 minutes after the injection, to check you tolerate the Botox well, which most people do.
Whats great about this procedure is that youll experience the benefits quickly, in a few days. When you need to urinate, it wont be such an urgent need. The injection lasts about six months, and you can have further injections.
One possible side effect of the injections is the onset of urine retention . The risk of this occurring is small: around 5-10% and normal emptying returns as the injections wear off .
Also Check: Yoga Exercises For Prolapsed Bladder
What To Expect: Botox Injection For Overactive Bladder
Youve probably heard of Botox being used to improve the cosmetic appearance of facial wrinkles. However, botox has many medical uses that go beyond improving ones appearance. For example, botox is commonly used to improve internal body functions. In the field of urology, it can be injected into the bladder muscle to improve symptoms of overactive bladder .
What is botox?
Botox is derived from the most poisonous substance known to manbotulinum toxin. This neurotoxin is produced by the Clostridium bacterium, responsible for botulism. Botulism is a rare but serious illness that can result in paralysis. Botulinum toxin, when used in minute quantities in a derivative known as botox, is a magically effective and powerful potion.
How does botox work?
Botox is a neuromuscular blocking agent that weakens or paralyzes muscles. Beyond cosmetics, it can be beneficial for a variety of medical conditions that have some form of localized muscle overactivity. Botox is generally used to improve conditions with muscle spasticity, involuntary muscle contractions, excessive sweating and eyelid or eye muscle spasm.
Botox to treat Overactive Bladder
Overactive Bladder syndrome can be described by the symptoms of urinary urgency , with or without urgency incontinence . Its usually accompanied by frequent urination during both day and night hours. OAB has been described as the bladder squeezing without your permission to do so.
The Refractory Overactive Bladder
Pharmacotherapy in conjunction with behavioral and dietary advice remains the mainstay of the initial management for most patients presenting with OABS. Anticholinergic medications, however, can cause mild to moderate side effects including dry mouth, gastro-intestinal disturbances including constipation, blurred vision, dry eyes, drowsiness, and skin reactions. Rarely, central nervous system stimulation can lead to restlessness, disorientation, hallucinations, and convulsions. Unwanted side effects of anticholinergenics and poor long-term compliance can be progressive issues in patients with symptomatic OAB. The International Consultation on Incontinence states that when the first-line approach is not satisfactory or fails after 8-12 weeks, alternative therapies including surgical management options should be considered.
The main principles of further surgical intervention in patients with the refractory OAB is the utilization of procedures with a potential to achieve a reduction in bladder pressure, induce stabilization of overactivity, and increase bladder capacity. Current interventions include the use of intradetrusor botulinum toxin-A injections and SNM. In more severe cases in which both the above-mentioned interventions fail to improve symptoms, the patient can be counseled on bladder reconstructive surgery such as urinary diversion, augmentation cystoplasty, or detrusor myomectomy.
Recommended Reading: Over The Counter Bladder Medication
What Is Overactive Bladder And How Can You Treat It
Overactive bladder is estimated to affect between 12-14% of the UKs population. It can feel like an embarrassing condition to have, but it is treatable, and major strides have been made in treatment in recent years.
Consultant urologist Mr Jeremy Ockrim talks through the definition of overactive bladder, some potential causes and cutting-edge treatment options.
Overactive Bladder Is A Common And Treatable Condition
Urge incontinence is usually associated with a strong, almost overpowering sense of a need to urinate with concern that you will not be able to make it to the bathroom in time. Overactive bladder may occur with or without urine leakage . Common symptoms are:
- Frequent urge to urinate, in the daytime and at night
- Loss of urine without meaning to urinate
- Sudden and urgent need to urinate
- Bladder pain or discomfort
This condition may be due to actual spasms of the bladder muscle or increased sensitivity of the bladder. These bladder spasms often happen when your bladder is not very full and can be triggered by hearing or feeling running water, cold air or even arriving at home and putting your key in the door. Occasionally it is triggered by a particular amount of urine in the bladder.
Don’t Miss: I Have A Weak Bladder Help
How Is Urinary Incontinence Managed
Your GP will first suggest making lifestyle changes to improve symptoms, including weight loss and cutting down on alcohol and caffeine. Pelvic floor exercises are also recommended to strengthen pelvic floor muscles, which often weaken following childbirth or as a natural result of ageing.
Many women also benefit from using incontinence products, like pads, absorbent pants, or handheld urinals. Sometimes, medicine may be prescribed to help manage symptoms.
If these measures fail, you may be referred for bladder training, guided by a specialist who can help teach you ways to train yourself to wait longer to pass urine.
In some cases, medication or surgery may be the best option where all other means have been unsuccessful.
Seven Effective Treatments For Overactive Bladder
Overactive bladder occurs when sudden or frequent urges to urinate become hard to control, and can often lead to leakage .
In order to best treat overactive bladder, a urologist must pinpoint the underlying cause. Treatment will depend on symptom severity and the degree to which they impact someone’s quality of life. In general, there are three approaches to treatment: medication, behavioral interventions, and surgery.
Also Check: Why Is My Bladder Not Emptying
What Are The Risks Involved In Colposuspension Procedures
Colposuspension has the same risks as the mid-urethral tape, as well as some additional risks associated with it being a more significant procedure, including difficulty emptying the bladder fully, recurring UTIs and painful sex.
There are no risks associated with vaginal healing because the procedure is not carried out through the vagina.
View our patient resources page to download more information regarding procedures for incontinence.
Understanding Your Urinary Tract
Waste from your body is removed from your blood stream by your kidneys and becomes urine. Normally, urine passes down the ureters into your bladder . A sphincter made of muscle circles the opening of your bladder, where urine flows out of your bladder. The sphincter acts like a valve that opens and closes to control when the urine comes out of your body. When you urinate, your bladder squeezes and your sphincter relaxes. Urine passes from the bladder through the urethra and out of your body. In women, the urethral opening is right above the vagina. In men, the urethral opening is at the tip of the penis. Surgery may involve any of these parts of your urinary tract as well as your intestines or your stomach.
Read Also: Can Being Constipated Affect Your Bladder
Stress & Urinary Incontinence Treatment Options
Several stress incontinence treatment exists and our team of doctors and womens health physiotherapists will recommend treatment for incontinence based on several health factors including age, condition and severity of urinary symptoms.
Sometimes it might be necessary to conduct a bladder operation however these procedures are commonly carried out with manageable symptoms and normally have a quick recovery time with the right after care. Read more about incontinence treatments below.
Probing Sui Surgerys Effects On Bladder Symptoms
SUI surgery produces successful, durable stress-associated leakage-correction outcomes and good rates of patient satisfaction. In clinical practice, it also has been associated with secondary OAB symptom relief. However, the surgerys precise effect on bladder storage symptoms is poorly understood, and postsurgical OAB outcomes have not been well-documented in medical literature.
Analyzing data from three large clinical trials involving more than 1,600 women, researchers from Cleveland Clinic and eight other U.S. medical institutions sought to assess how incontinence-correction surgical procedures affected OAB symptoms in mixed, stress-predominant incontinence patients one and five years postoperatively. They also looked for clinical, physiological or other characteristics that might predict postsurgical bladder symptom outcomes.
The researchers analysis, published recently in Obstetrics and Gynecology, found that a majority of patients who underwent either Burch colposuspension, autologous pubovaginal sling, or retropubic or transobturator midurethral sling surgeries, reported significant OAB symptom improvement. Significant improvement was defined as a positive change of 70 percent or more from baseline symptoms as measured by the Urinary Distress Inventory-Irritative subscale.
Also Check: Ways To Strengthen Your Bladder
The Truth About Overactive Bladder
Today, as a urogynecologist, I focus on pelvic floor disorders in women, which include overactive bladder, urinary incontinence, bowel control problems, pelvic organ prolapse, and more. My job is truly rewarding because I get to help give someone their life back. Often, with a condition like overactive bladder, patients just accept their new normal, even if its holding them back. With overactive bladder, people will feel a frequent and urgent need to urinate, sometimes with actual leakage of urine on the way to the bathroom. Patients might think its a normal part of aging or something they have to live with after giving birth, but thats not true. Its not something anybody should just accept. People can feel tethered to a place where there is a bathroom, missing out on travel or special events because they dont know if theyll find a toilet in time. Worrying about their overactive bladder is a constant distraction and they find it hard to be present and engage with their daily lives because of it. It can be really isolating and significantly impact quality of life, but it doesnt have to be that way. There are good treatments and behavioral changes that can help, and being able to offer someone a life-changing resource is very gratifying.
Drugs For Overactive Bladder
In people with overactive bladder, muscles in the bladder wall contract at the wrong time. A group of drugs called anticholinergics combat this problem by blocking the nerve signals related to bladder muscle contractions. Research suggests that these drugs also might increase bladder capacity and decrease the urge to go.
Anticholinergic drugs include:
Oxytrol for women is the only drug available over the counter. Overall, these drugs work about the same in treating overactive bladder, and generally people tolerate all of them well. The main side effect is dry mouth, but anticholinergics also can cause constipation, blurred vision, and increased heartbeat.
Anticholinergics arent right for everyone. Some people with glaucoma, urinary retention, or gastrointestinal disease should avoid using anticholinergic drugs.
The drugs mirabegron and vibegron called beta-3 adrenergic agonists. These medications work by activating a protein receptor in bladder muscles that relaxes them and helps the bladder fill and store urine.
Another type of drug for overactive bladder is the tricyclic antidepressantimipramine hydrochloride , which also relaxes bladder muscles.
Doctors also treat men with drugs that relax a muscle at the bladder neck and prostate to help with emptying. They include:
Also Check: Homeopathic Medicine For Bladder Weakness
Read Also: Feels Like I Have To Pee But Bladder Is Empty
Can Hormone Therapy Help Females Manage Oab Symptoms
For postmenopausal females with OAB, vaginal estrogen hormone therapies may have a role, but only in certain situations.
Estrogens do have a role in the function of the urinary tract, though the use of estrogen replacement therapy in the management of OAB in postmenopausal females remains controversial for several reasons. Therefore, this question requires a very individualized approach that is best addressed between an individual and their doctor.
Vaginal estrogen cream can be beneficial in some instances. For example, it may help when vaginal atrophy and dryness contribute to urinary symptoms, particularly if the person is experiencing recurrent urinary tract infections alongside OAB. Treatment with vaginal estrogen cream may also be effective for some people with mild stress urinary incontinence, such as leakage that occurs with coughing or laughing.
However, for most females with OAB particularly those who are premenopausal hormone therapy is a treatment with limited efficacy.
Is Surgery For Me
The decision to have surgery can be difficult, as there are pros and cons with each procedure. But, if your OAB symptoms are severe, and you have tried all other options, surgery may be right for you. Be sure to talk with your doctor about all of your options, including what the procedure is like, the materials used, the pros and cons of different surgical options, and the recovery times for each. Its also important to talk with your doctor about what you can expect after surgery, as not everyone is completely cured from incontinence after these procedures. A frank discussion with your doctor, and your own research on surgical options can help you decide if this is a path you would like to consider.
Learn more about surgery options for OAB in our 6th and final video of our series on managing Overactive Bladder.
You May Like: Is Cystitis A Bladder Infection
When Is Botox To The Bladder Used
If medication has failed to control an unstable bladder, then you may be offered Botox treatment. During such a procedure, Botulinum toxin A is injected into the sides of the bladder to stop urge incontinence or overactive bladder syndrome.
This is a short procedure that requires no incisions or stitches. It involves injecting Botox into the bladder wall via a camera called a cystoscope. You will be able to go home the same day, after passing urine.
The effects of botox often last for 3-12 months, and treatment can be repeated if found to have helped.
Other Treatments To Try

In rare cases when all OAB treatment fails and overactive bladder is severe, doctors may recommend one of several types of surgery.
A procedure called bladder augmentation uses part of the bowel to increase bladder capacity. Or, urinary diversion, an alternate route for bladder drainage for severe, complicated OAB patients.
Sacral nerve stimulation. Another procedure implants a small device, similar to a pacemaker, under the skin. The device is connected to a wire, which sends small electrical pulses to nerves around the pelvic floor that control the bladder and muscles surrounding it. This helps build bladder control. Itâs often called a bladder pacemaker. The main limitation with this treatment is that it keeps you from having a spinal MRI.
Percutaneous tibial nerve stimulation. The doctor places a needle on nerves near your ankle that affect bladder control. Youâll have one session a week for 12 weeks and then maintenance treatments as needed. This procedure is done in the office.
An overactive bladder doesnât have to get in the way of your daily life. With a little time, patience, and the right treatment, you can regain control — and peace of mind. Whatever treatment for overactive bladder you and your doctor decide upon, it’s important that you stick with it. If you do, chances are your condition will improve in time.
Show Sources
Read Also: Treatment Of Muscle Invasive Bladder Cancer
How Can Overactive Bladder Be Treated
For generations, those with overactive bladder were told that they would have to live with urgency and incontinence symptoms, with their options limited to toilet mapping staying in close vicinity to toilet facilities or wearing incontinence pads.
Options for treatment evolved, but were still limited to medical therapy , major surgery, physical therapies and behavioural techniques .
The good news is that, in recent times, the treatment options available and their success rate has much improved, although knowledge of new techniques and access to specialists remains limited.
Modern, less invasive advances, such as Botox injections and sacral nerve stimulation therapy, now mean that you can be treated much more successfully.