Time Elapsed Since Hysterectomy
The amount of time since the hysterectomy can influence prolapse occurrence.
The risk of prolapse increases with increasing length of time elapsed since the hysterectomy.
One study reported the the proportion of women with requiring a prolapse repair 20 years after hysterectomy was 3.3% and this figure increased to 5.1% at 30 years after hysterectomy.1
Why Do I Need A Vaginal Repair
A vaginal repair operation is performed to correct a prolapse. It is possible to perform this at the same time as a hysterectomy. A vaginal repair is carried out in order to tighten and lift the weakened tissues allowing the bladder and bowel to return to their correct positions and reducing or alleviating symptoms. This surgery is carried out vaginally using dissolvable stitches to support the muscles.
Laparoscopic Hysterectomy And Prolapse Bladder Repair
sharron2071
Hi I’m waiting to have a hysterectomy done by laparoscopy taking womb cervix tubes and maybe ovaries depending if they are healthy or not and prolapsed bladder repaired at same time, has anybody had this done and can tell me what there recovery was like and how long they had to stay in hospital please x
Posted 7 years ago
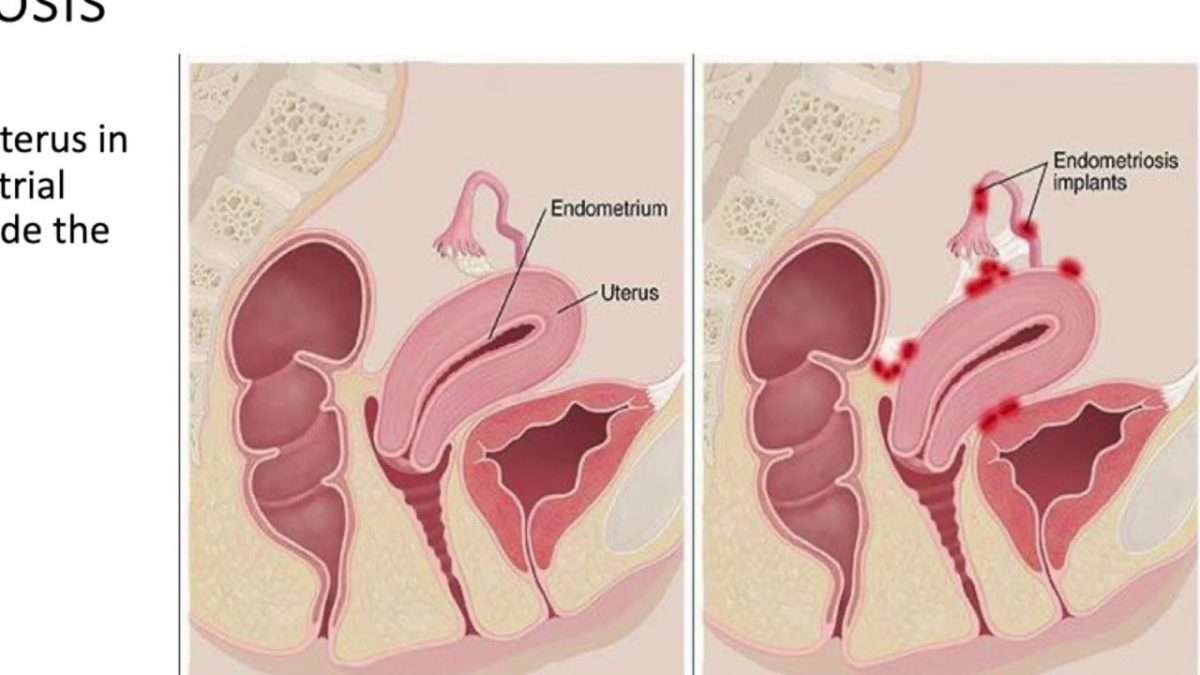
Hi. I’m also waiting for lap hysterectomy inc ovaries. When I had a lap for just release of ovaries and womb for endometriosis they took catheter out before I woke up and I was able to get up for wee as soon as I’d drunk my cuppa but was on day case and wasnt meant to stay in but guessing by what you’ve been told its not the case when they do actual hysterectomy. I wish hospitals would tell you that! Saying that I had catheter in following complications after i gave birth a number of years ago and you hardly know when its being removed so please Dont worry about that. I have been told one night in and 4 weeks off work if that helps but by the posts on here we need to take it easy so doesn’t set us back. When are you going in? Good luck xx
Recommended Reading: What Can Cause You To Lose Control Of Your Bladder
Managing Your Body Weight
Body weight has the potential to increases the load on the pelvic floor, especially abdominal fat that sits around the organs directly above the pelvic floor.
Managing your body weight to protect your pelvic floor involves losing weight if you are overweight and avoiding unnecessary weight gain.
Carrying too much abdominal weight increases the load on your pelvic floor and your pelvic floor supports increasing the risk of strain and prolapse.
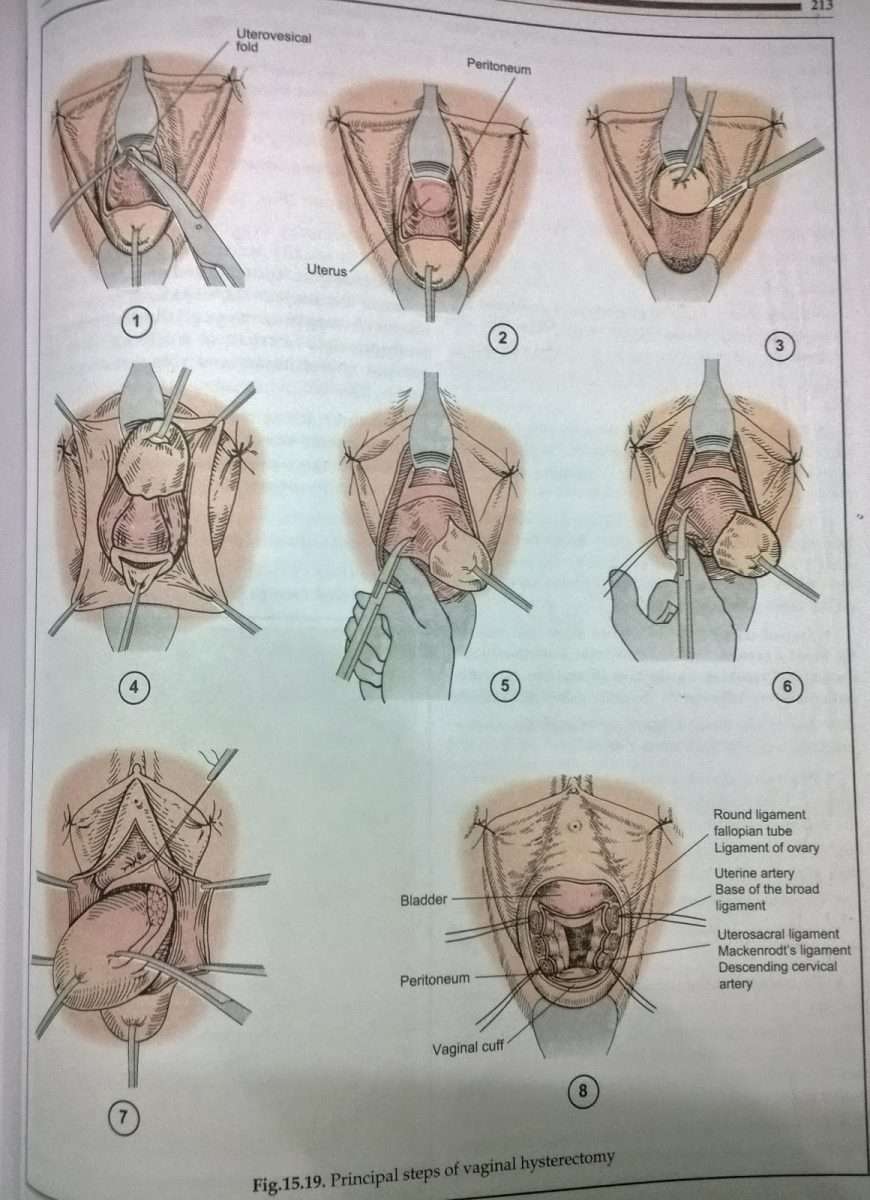
Vaginal Hysterectomy For Prolapse
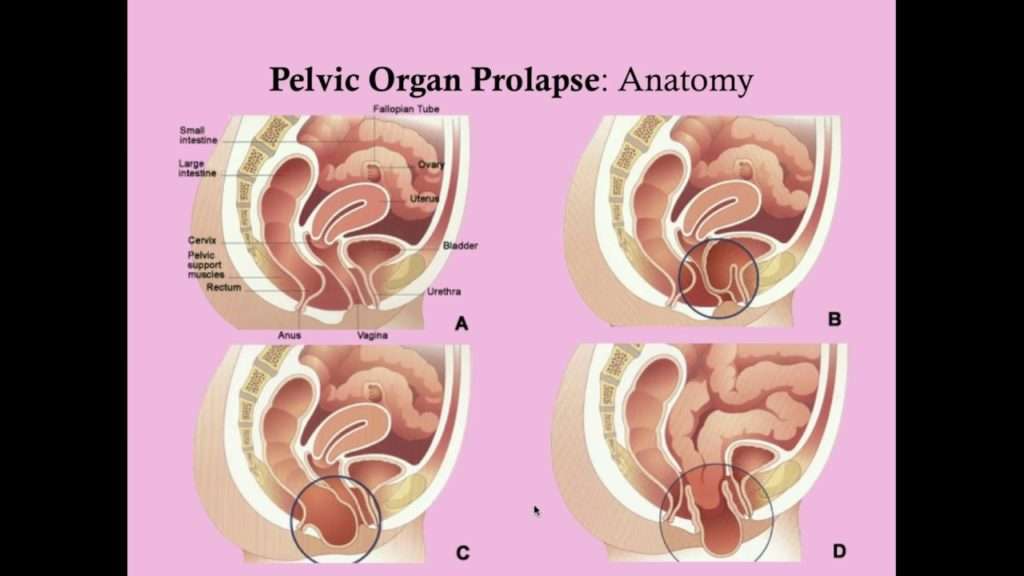
Prolapse is the loss of normal support of the vagina and/or uterus . Prolapse of the uterus and/or vaginal walls is a common condition with up to 11% of women requiring surgery during their lifetime. Prolapse generally occurs due to damage to the supporting structures of the uterus or vagina. Weakening of the supports can occur during childbirth, following chronic heavy lifting or straining , chronic cough, obesity, and as part of the aging process. In some cases, there may be a genetic weakness of the supportive tissues.
Prolapse of the uterus can cause an uncomfortable bulging sensation, a feeling of fullness, or pressure in the vagina. In more advanced prolapse the cervix can extend beyond the entrance to the vagina.
Normal uterus and vagina, no prolapse , and Prolapse of the uterus, bladder, and rectum
This is a procedure in which the uterus is surgically removed through the vagina. The operation is frequently combined with prolapse repairs of the bladder and/or bowel. There are no abdominal or laparoscopic incisions.
Appearance after hysterectomy
A vaginal hysterectomy offers many benefits over abdominal or laparoscopic procedures. It offers overall fewer complications, shorter healing time, less pain, less scarring, a lower chance of infection, less risk of hernias, and faster return to activities. Also, a prolapsed uterus is easier to access via the vagina.
With any operation there is always a risk of complications:
Read Also: How To Do Kegel Exercises For Overactive Bladder
Who Performs Uterine Prolapse Surgery
The following specialists perform uterine prolapse surgery:
-
Obstetrician-gynecologists specialize in womens health and .
-
Urologists specialize in diseases and conditions of the urinary tract and the male reproductive organs.
-
Female pelvic medicine and reconstructive surgeons are urologists or gynecologists who have completed specialized training in womens pelvic floor disorders.
Recommended Reading: Does Macrobid Treat Bladder Infection
Free Pelvic Floor Educational Series
Dr. Sarah Duvall, PT, DPT, CPT and the CES Team have helped thousands of women create the strength and stability needed to overcome common and not-so-common pelvic floor issues.
Join us today for this 4-part Pelvic Floor Video Series, absolutely free.
We dont spam or give your information to any third parties. View our Terms of Use and Privacy Policy.
You May Like: Bladder Cancer Ct Scan With Contrast
Results Demonstrate Hysterectomy Cost
TVH/USLS costs on average $587.61 more than HPXY per case of prolapse. But TVH/USLS prevents 1.1% of women from post-menopausal bleeding and diagnostic evaluation and 1% of women from undergoing subsequent major surgery for the treatment of either prolapse or cancer. The model calculated the cost of treating endometrial cancer at $2,698,677 this makes TVH/USLS a cost-effective treatment in preventing death from endometrial cancer. Despite the low incidence of endometrial cancer among prolapse patients, hysterectomy is cost-effective because of the high costs of treating the cancer, says Dr. Chang.
Vaginal Repair For Anterior And Posterior Vaginal Wall Prolapse
A vaginal prolapse happens when the supporting sling which holds the womb and other organs in their position, is no longer strong enough to do this . The womb can drop down into different positions and cause different types of prolapse. A prolapse may be described as something coming down or a dragging sensation. The vagina is a hollow muscle which supports both the bladder and the bowel. Prolapse of the bladder wall may cause symptoms involving the passing of urine, for example the frequency, urge and stress incontinence. Prolapse of the bowel may cause symptoms of constipation and other bowel symptoms.
Recommended Reading: Why Is My Bladder Always Full
Prolapse Surgery Success Rates
The success of prolapse surgery depends on many different factors, including:
- how bad your prolapse is,
- what parts of your pelvic floor is affected,
- what type of surgery you get, and
- lifestyle or genetic factors that could increase the risk of another prolapse in the future.
Studies show that about 80 percent of prolapse surgeries are still successful after 10 years. About 10 to 20 percent of women will have some movement or bulging again, but its usually not enough to need another surgery. Only about two to three percent of women will need a repeat prolapse surgery.
How Do I Prepare For The Surgery
Please read the information leaflet. Share the information it contains with your partner and family so that they can be of help and support. There may be information they need to know, especially if they are taking care of you following this examination.
Make sure that all of your questions have been answered to your satisfaction and that you fully understand what is going to happen to you.
Read Also: Difference Between Bladder And Urinary Tract Infection
Uterine Prolapse & Hysterectomy Surgery
Uterine prolapse is a condition that occurs when the uterus slips down into, or protrudes out of, the vaginal canal. Normally, the uterus is supported by a network of muscles and ligaments. When the pelvic floor muscles and ligaments stretch and weaken, they provide inadequate support for the uterus, causing the uterus to prolapse from its normal position. Uterine prolapse affects women of all ages, but most commonly affects postmenopausal women who have had vaginal deliveries during childbirth. Depending on the severity of the prolapse, treatment may or may not be necessary. For cases in which uterine prolapse does impact daily life, effective treatments are available. Uterine prolapse is estimated to account for approximately 200,000 prolapse surgeries each year in the United States.
Causes Uterine prolapse is a condition that has a number of causes and risk factors. Most often, pregnancy and trauma during childbirth, especially with larger newborns and difficult labor or delivery, cause muscle weakness and stretching of the supporting tissues and ligaments of the uterus. The effects of aging, including decreased muscle tone and reduced amounts of estrogen, are also believed to contribute to uterine prolapse. Other risk factors for uterine prolapse include tumors in the pelvic cavity, collagen quality, smoking, and obesity.
Key Points For Preventing Prolapse After Hysterectomy
There are a number of ways you can reduce your risk of prolapse after hysterectomy.
To reduce your risk of prolapse:
- Speak with your surgeon to better understand the hysterectomy procedure youre undergoing and know your risks
- Manage your general health and lifestyle factors that can influence your risk of prolapse.
Read Also: What Does Overactive Bladder Feel Like
What Can You Do If Intercourse Is Painful
One way to reduce discomfort during intercourse is to use a lubricant. Ask the pharmacist to recommend a good lubricant or try a few to see which one works well for you. Try to avoid using Vaseline or hand lotion, as these tend to dry out quickly. If vaginal dryness is a longstanding problem, consider asking your doctor about vaginal estrogen. Estrogen makes the vagina more elastic and increases natural lubrication. Local forms of estrogen, available as creams, estrogen-containing silastic rings or small pills inserted into the vagina can improve vaginal health without any significant absorption of the estrogen into the bloodstream and the body.
Women With Previous Hysterectomy
Laparoscopic Sacrocolpopexy
This is the most common operation performed with access from the abdomen for women who do not have the uterus and present with apical prolapse or prolapse of the top part of the vagina.
After entering the abdomen through small laparoscopic incisions and inserting a camera to be able to see inside the abdomen and pelvis, the surgeon dissects the vagina from the bladder anteriorly and the rectum posteriorly.
A graft fashioned in a Y shape is then sutured to the anterior and posterior aspects of the vagina.
The surgeon then opens the membrane that covers the sacral bone and exposed the promontory which is the uppermost part of the sacrum below the lumbar spine. The graft is the sutured to ligaments over the bone providing support and aiming to bring the top of the vagina to its natural elevated position.
Don’t Miss: Bladder Cancer Symptoms Mayo Clinic
Day 1 4 After Leaving Hospital
- No domestic chores whatsoever. Lie down for at least one hour a day.
- Listen to your body/mind/spirit if it wants to go to sleep then do so for you will have less energy than you thought.
- No stretching or lifting anything heavier than a kettle with water in it for one cup/mug full.
- Try to maintain your gentle mobility exercises.
- Enjoy a daily bath/shower.
Operative Steps Of Tlh
Step 1.
The operation starts with the placement of the Hohl uterine manipulator .17 The patient is placed in the Trendelenburg position to allow easy vaginal access for insertion of the uterine manipulator. In addition, a transurethral pelvic catheter is inserted. The arms of the patient are positioned alongside the body to give ample room for the first and second surgeons to operate. The first surgeon stands on the left side of the patient the second surgeon stands on the right side. An assistant sits between the legs of the patient and can manipulate the uterus with the uterine manipulator.
The operation begins by positioning the Veress cannula, which is later replaced by a 10-mm optic trocar. After introduction of the High Definition Television video optic, an exploration of the entire abdominal cavity, focusing on the minor pelvis, is performed. The bladder, rectum, pelvic vessels, and both ureters are identified and displayed.
Step 2: technique 1primary uterine artery ligation.
A, Separation of round ligament with NightKNIFE . B, Division of ovarian ligament. C, Preparation of uterine wall/broad ligament parallel to ascending branch of uterine artery under safe distance to ureter . D, Cutting after coagulation of skeletonized uterine artery.
Ibrahim Alkatout, Department of Gynecology and Obstetrics, University Hospitals Schleswig-Holstein, Kiel, Germany.
Günter Noé, Department of Gynecology and Obstetrics, Dormagen Hospital, Dormagen, Germany.
Read Also: Botox Dose For Overactive Bladder
What Should I Avoid After Pelvic Prolapse Surgery
Theres a few things you should steer clear of while youre still healing:
- Limit tea, coffee and alcohol as these can make you urinate more often
- Steer clear of strenuous tasks, standing still for long periods and lifting anything heavier than half a kettle of water – some surgeons may advise avoiding heavy lifting in the long-term, too
- Avoid smoking, as a smokers cough can strain your pelvic floor muscles
- Restrict weight gain as this can put pressure on your pelvic region
- Hold off from sex until youve healed completely . Even when youre ready, sex may cause a little discomfort. A specialist pelvic health physiotherapist can recommend vaginal lubricants and positions for reducing pain.
Addition Information About Vaginal Surgery When A Synthetic Or Biologic Graft Is Used
In Australia, in January 2018 the TGA withdrew approval for the used of synthetic and biologic mesh for trans-vaginal prolapse repair. The TGA continues to approve synthetic and biological mesh for prolapse when placed using laparoscopy, robot assisted and through an abdominal incision.
In the USA, the Food and Drug Administration has issued the following safety communication regarding the use of mesh.
The FDA wants to inform you about the complications that can occur when surgical mesh is used to treat Pelvic Organ Prolapse and Stress Urinary Incontinence , and provide you with questions to ask your surgeon before having these procedures. This is part of our commitment to keep healthcare professionals and the public informed about the medical products we regulate.
FDA has received reports of complications associated with the placement of mesh through an incision made in the wall of the vagina. Although rare, these complications can have serious consequences. The reports have not been linked to a single brand or model of mesh.
The most frequent complications included erosion through the vagina, infection, pain, urinary problems and recurrence of the prolapse and/or incontinence.
Background
Pelvic organ prolapse can cause pain or problems with bowel and bladder functions or interfere with sexual activity.
Stress urinary incontinence is a type of incontinence caused by leakage of urine during moments of physical stress.
Talking to your doctor
Recommended Reading: Herbal Supplements For Overactive Bladder
Treatment Of A Vault Prolapse
A vaginal vault prolapse is a defect that occur highs in the vagina, entailing a surgical approach through either the vagina or the abdomen. Generally, the abdomen is the entry of choice for a severe vaginal vault prolapse.
The surgical procedure for correction of vault prolapse is a sacrocolpopexy, in which the surgeon attaches the vagina to a strong ligament over the backbone using a special mesh. This procedure can be performed either as a keyhole operation or as an open procedure.
Oxford is one of few centres in the UK that can offer the laparoscopic technique, as it requires a high level of laparoscopic skills and special equipment. We perform many laparoscopic sacrocolpopexy operations and have published our results in peer-reviewed journals.
Can Prolapse Cause Problems With Sex
Prolapse does not usually cause problems with sex. If prolapse results in bulging of the bladder or rectum into the vagina, the bulge can be easily pushed back into place before intercourse, and most women with prolapse say they don’t notice it during intercourse. Also, if you have a prolapse, you should know that intercourse will not cause any harm to whatever is bulging: your bladder, vagina, uterus or rectum.
Don’t Miss: What Can Be Done For Bladder Leakage
When To Call A Professional
Prolapse of the pelvic organs is generally a nonthreatening problem. You should contact your physician for an evaluation if you are having bothersome symptoms, and you suspect you might have this problem. It is also important to report changes in urinary symptoms to your doctor, since urinary infections are a possible complication of prolapse.
What Is Pelvic Organ Prolapse Surgery
Perhaps youve had a pelvic organ prolapse, and non-surgical treatments arent helping? Or maybe your prolapse is more severe? If so, your surgeon may recommend, pelvic organ prolapse surgery.
This surgery involves lifting the pelvic organs, such as the bladder, bowel and uterus, and stitching the tissues around them to give you more support.
Also Check: Does Beer Help Bladder Infections
How Effective Is Vaginal Wall Repair Surgery
Vaginal wall repair surgery can stabilize the affected organs. This can reduce bladder and bowel problems, pain and feelings of pressure. After the procedure, about 80 to 90 out of 100 women no longer have problems such as urine leakage or pain during sex at least for a while. There is a lack of research on how well this surgery works compared to pelvic floor exercises and pessaries.
The previously prolapsed organs may slip down again following initially successful vaginal wall repair surgery. Studies have shown that this happens within three years in about 38 out of 100 women who have operations using their own tissue. Using a synthetic mesh reduces this risk.
Can Uterine Prolapse Be Prevented
You may not be able to prevent all cases of uterine prolapse, but there are ways to cut back on your risk of developing a prolapse. A few lifestyle tips that can reduce your risk of prolapse include:
- Maintaining a healthy body weight.
- Exercising regularly. In addition, do Kegel exercises to strengthen your pelvic floor muscles. Remember, check with your healthcare provider before starting any new exercise program.
- Eating a healthy diet. Talk to your healthcare provider or a nutritionist about the best diet for you.
- Stop smoking. This reduces the risk of developing a chronic cough, which can put extra strain on the pelvic muscles.
- Using proper lifting techniques.
Read Also: Bladder Infection And Back Pain