What Causes Rectal Prolapse
- Anything that increases the pressure inside your tummy can make you more likely to develop a rectal prolapse. This can include:
- Constipation.
- Straining to pass urine due to a swollen prostate gland.
- Pregnancy.
- Damage to the back passage or pelvis from previous surgery.
- Damage to the muscle on the floor of the pelvis.
- Infections of the bowel with certain types of microbes called parasites .
- Diseases of the nervous system such as multiple sclerosis.
- Damage to the nerves from back surgery, a slipped disc, or an accident injuring the pelvic nerves.
- Mental health conditions associated with constipation, such as:
- Depression.
- Anxiety .
- A side-effect of medicines used to treat psychiatric disorders.
In children, rectal prolapse can occur in:
- Ehlers-Danlos syndrome.
- Hirschsprung’s disease .
- Malnutrition .
Prolapse of the bladder or womb doesn’t cause rectal prolapse but is sometimes associated with it.
How To Avoid Lower Back Pain
Back pain can occur because of a bad move, overloading, etc. It can be interesting to take a few minutes to analyze pain:
- Does it appear in the morning? During the night? In the evening, after a long workday?
- Is it caused by a particular move? A special posture?
- Is it improved by massage? Heat? Stretching?
These indications will help you identify what causes the pain and what relieves it.
In any case, the back likes and has to move! But be careful not to do painful movements, because the worst is not moving, being immobilized. Lets not forget that the word physiotherapist comes from the old Greek and means heal by movement.
Sports we recommend are soft sports like walking, swimming, gym, and you can try yoga or pilates as well.
Treatment Options For A Prolapsed Bladder
There are many treatment options for a prolapsed bladder. One of the most common forms of treatment, and one that many people opt for first, is physical therapy. The pelvic floor is a muscle, and just like other muscles in the body, it can be strengthened with the appropriate exercises.
A physical therapist who specializes in pelvic floor therapy can work with you to determine the extent of your prolapse, gauge the strength of your pelvic floor muscles, and set you up on a routine to ensure the pelvic floor is working as it should.
Another option for treatment is a pessary. A pessary is a small disc-shaped device that is inserted into the vagina and helps to hold things up, relieving some of the pressure and other symptoms of prolapse. A pessary may be used in conjunction with physical therapy and may be ideal for those who experience symptoms during specific activities, such as when working.
If you have a prolapsed bladder, know that you can still live a very full and active life, doing many of the same things you did prior to having a prolapse. Talk to your doctor about treatment options. A pelvic floor physical therapist is a good first step and can help you try to strengthen your muscles naturally. Beyond that, a urogynecologist is a good option for more advanced treatments.
You May Like: Can Bladder Infection Clear Up On Its Own
What Is Uterine And Bladder Prolapse
The uterus and the bladder are held in their normal positions just above the inside end of the vagina by a “hammock” made up of supportive muscles and ligaments. Wear and tear on these supportive structures in the pelvis can allow the bottom of the uterus, the floor of the bladder or both to sag through the muscle and ligament layers.
When this occurs, the uterus or bladder can create a bulge into the vagina. In severe cases, it is possible for the sagging uterus or bladder to work its way down far enough that the bulge can appear at the vagina’s opening or even protrude from the opening.
When the uterus sags downward, it is called uterine prolapse. When the bladder sags, it is called bladder prolapse, also known as a cystocele.
Various stresses can cause the pelvic muscles and ligaments to weaken and lead to uterine or bladder prolapse. The most significant stress on these muscles and ligaments is childbirth. Women who have had multiple pregnancies and vaginal delivery are more likely to develop prolapse.
Other stresses that can lead to prolapse include constipation with a habit of frequent straining to pass stool and a chronic cough. Obesity also can strain the pelvic muscles.
Support problems in the pelvis become worse after menopause because the pelvic tissues depend on estrogen to help them keep their tone, and estrogen levels drop after menopause.
Normal Positions Of Pelvic Organs
Image: Thinkstock
In pelvic organ prolapse, the pelvic floormuscles weaken, causing one or more of thepelvic organs to fall downward into or out ofthe vagina.
What is pelvic organ prolapse?
How prolapse is named depends on which organ is affected:
- Cystocele is when the into the vagina, creating a bulge. It’s the most common form of prolapse.
- Rectocele is when the rectum bulges into the back wall of the vagina.
- Uterine prolapse involves the uterus dropping into the vagina.
Most of the time, pelvic organ prolapse is the result of carryingand vaginally deliveringchildren, which weakens the pelvic floor. “The baby’s head going through the vaginal canal stretches out the connective tissues,” says Dr. May Wakamatsu, assistant professor at Harvard Medical School and division director of Female Pelvic Medicine and Reconstructive Surgery at Massachusetts General Hospital.
Getting older, being overweight, and having a condition that involves frequent coughing also make a woman vulnerable to prolapse.
In pelvic organ prolapse, the pelvic floor muscles weaken, causing one or more of the pelvic organs to fall downward into or out of the vagina.
Don’t Miss: Whats The Difference Between Uti And Bladder Infection
What Happens At Your Appointment
Your doctor will ask if they can do an internal pelvic examination.
For this you’ll need to undress from the waist down and lie back on the examination bed.
Your doctor will then feel for any lumps in your pelvic area and inside your vagina.
They may gently put an instrument called a speculum into your vagina to hold the walls of it open so they can see if there’s a prolapse.
Sometimes they’ll ask you to lie on your left-hand side and examine you in that position to get a better view of the prolapse.
You can ask for this examination to be done by a female doctor and, if you like, bring someone you trust along with you for support.
Diagnosis Of Bladder Prolapse
Bladder prolapse is diagnosed by:
- medical history including checking for possible risk factors
- physical vaginal examination to allow assessment of the degree of prolapse, pelvic floor muscle function, presence of any other prolapse and other abnormalities in the pelvis, such as tumours or masses.
You May Like: Can Azo Cure A Bladder Infection
What Causes A Prolapsed Bladder
Factors commonly associated with causing a prolapsed bladder are those that weaken the pelvic floor muscles and ligaments that support the bladder, urethra, uterus, and rectum, which can lead to detachment from the ligaments or pelvic bone where the muscles attach:
- Pregnancy and childbirth: This is the most common cause of a prolapsed bladder. The delivery process is stressful on the vaginal tissues and muscles, which support a woman’s bladder.
- Aging can lead to weakening of the muscles.
- Menopause: Estrogen, a hormone that helps maintain the strength and health of supporting tissues in the vagina, is not produced after menopause.
- Previous pelvic surgery: such as hysterectomy
- Other risk factors that increase the pressure within the abdomen, leading to increased pressure on the pelvic floor muscles include chronic obstructive pulmonary disease , obesity, constipation, and heavy manual labor .
Can A Prolapse Be Prevented
There are several things you can do to reduce your risk of prolapse, including:
- doing regular pelvic floor exercises
- maintaining a healthy weight or losing weight if you’re overweight
- eating a high-fibre diet with plenty of fresh fruit, vegetables, and wholegrain bread and cereal to avoid constipation and straining when going to the toilet
- avoiding heavy lifting
If you smoke, stopping smoking may also help to reduce your risk of a prolapse.
You May Like: Period Underwear For Bladder Leakage
Prolapse Of The Vagina
In prolapse of the vagina, the upper part of the vagina drops down into the lower part, so that the vagina turns inside out. The upper part may drop part way through the vagina or all the way through, protruding outside the body and causing total vaginal prolapse. Usually, a cystocele or rectocele is also present.
Total vaginal prolapse may cause pain while sitting or walking. Sores may develop on the protruding vagina and cause bleeding and a discharge. Like prolapse of the uterus, prolapse of the vagina can cause problems with urination. Having a bowel movement may also be difficult.
Other Therapy For Prolapsed Bladder
Physical therapy such as electrical stimulation and biofeedback may be used for a prolapsed bladder to help strengthen the muscles in the pelvis.
- Electrical stimulation: A doctor can apply a probe to targeted muscles within the vagina or on the pelvic floor. The probe is attached to a device that measures and delivers small electrical currents that contract the muscles. These contractions help strengthen the muscles. A less intrusive type of electrical stimulation is available that magnetically stimulates the pudendal nerve from outside the body. This activates the muscles of the pelvic floor and may help treat incontinence.
- Biofeedback: A sensor is used to monitor muscle activity in the vagina and on the pelvic floor. The doctor can recommend exercises that can strengthen these muscles. These exercises may help strengthen the muscles to reverse or relieve some symptoms related to a prolapsed bladder. The sensor can monitor the muscular contractions during the exercises, and the doctor may be able to determine if the targeted muscles would benefit from the exercises.
Recommended Reading: Can Bladder Leakage Be Fixed
As Pop Worsens You May Notice:
- A bulging, pressure or heavy sensation in the vagina that worsens by the end of the day or during bowel movements
- The feeling of “sitting on a ball”
- Needing to push stool out of the rectum by placing fingers into or around the vagina during a bowel movement
- Difficulty starting to urinate or a weak or spraying stream of urine
- Urinary frequency or the sensation that you are unable to empty the bladder well
- Lower back discomfort
- The need to lift up the bulging vagina or uterus to start urination
- Urinary leakage with intercourse. Though unusual, severe prolapse can block the flow of urine and cause recurrent urinary tract infections or even kidney damage.
When The Bottom Falls Out: Prolapse In The Pelvis
Symptoms tend to occur when women are upright, straining, or coughing and to disappear when they are lying down and relaxing. For some women, sexual intercourse is painful.
Mild cases may not cause symptoms until the woman becomes older.
Prolapse of the rectum , small intestine , bladder , and urethra are particularly likely to occur together. A urethrocele and cystocele almost always occur together.
) or problems completely emptying the bladder .
You May Like: How Fast Can A Bladder Infection Come On
Key Points For Uterine Prolapse
-
Uterine prolapse occurs when the muscles and tissue in your pelvis weaken.
-
This allows your uterus to drop down into your vagina.
-
Common symptoms include leakage of urine, fullness in your pelvis, bulging in your vagina, lower-back pain, and constipation.
-
Treatment for uterine prolapse includes lifestyle changes, a pessary, or surgery to remove the uterus.
-
You may be able to prevent this condition with weight loss, a high fiber diet, not smoking, and doing Kegel exercises.
Treating Pelvic Organ Prolapse
There are several treatment options that Dr. Swainston may suggest for pelvic prolapse, depending on your situation. In some cases, doing exercises to strengthen the muscles that hold your pelvic organs in place will correct the problem.
A small device called a pessary can be inserted into your vagina to support the organs that are dropping out of place.
You may need surgery to repair the tissues that are allowing the organs to prolapse, or in some cases to remove the prolapsed organ.
If you have unusual symptoms, even if theyre vague and difficult to describe, book an appointment online or by phone with Dr. Swainston. The sooner he can diagnose pelvic organ prolapse, the greater the chances you can strengthen your pelvic floor muscles with exercises and avoid more invasive treatments.
You Might Also Enjoy…
Don’t Miss: Surgical Treatment For Overactive Bladder
Symptoms Of Bladder Prolapse
The symptoms of bladder prolapse depend on the severity of the prolapse, your level of physical activity and the presence of any other type of prolapse.They include:
- urinary stress incontinence leaking urine when coughing, sneezing, laughing, running or walking, or urge incontinence, which is urgently needing to go and leaking on the way
- needing to empty your bladder more frequently
- inability to completely empty your bladder when going to the toilet
- recurrent urinary tract infections
- protrusion of the vaginal wall out through the vaginal entrance
- needing to go back to the toilet immediately after finishing passing urine.
Is Bladder Cancer Painful
When its in its earliest stages, bladder cancer doesnt usually cause much pain. Some people have no pain whatsoever, while others may experience pain or burning when they urinate. Blood in the urine, either microscopic or visible to the naked eye, is commonly the first sign of bladder cancer.
As the cancer grows and spreads to other areas of the body or during treatment for bladder cancer, pain may become a bigger issue. You may experience pain:
- in the pelvis
- in bones
- when having sex
Sometimes, the disease itself isnt the only source of pain in people with advanced bladder cancer. It can also be caused by treatment. Chemotherapy, a common treatment method for bladder cancer, can cause uncomfortable side effects, such as mouth sores.
Chemotherapy can also cause peripheral neuropathy, which may present as pain, numbness, tingling, or other sensations in the hands, arms, feet, or legs.
Surgery may be a part of treatment for bladder cancer. The pain associated with surgery depends on the operation.
Early bladder cancer can be managed with a minimally invasive surgery, during which the tumor is scraped off the bladder wall from within.
More advanced bladder cancer may require surgery to remove the entire bladder. This operation is much longer and usually has a more painful recovery.
You May Like: Can Fibroids Cause Bladder Leakage
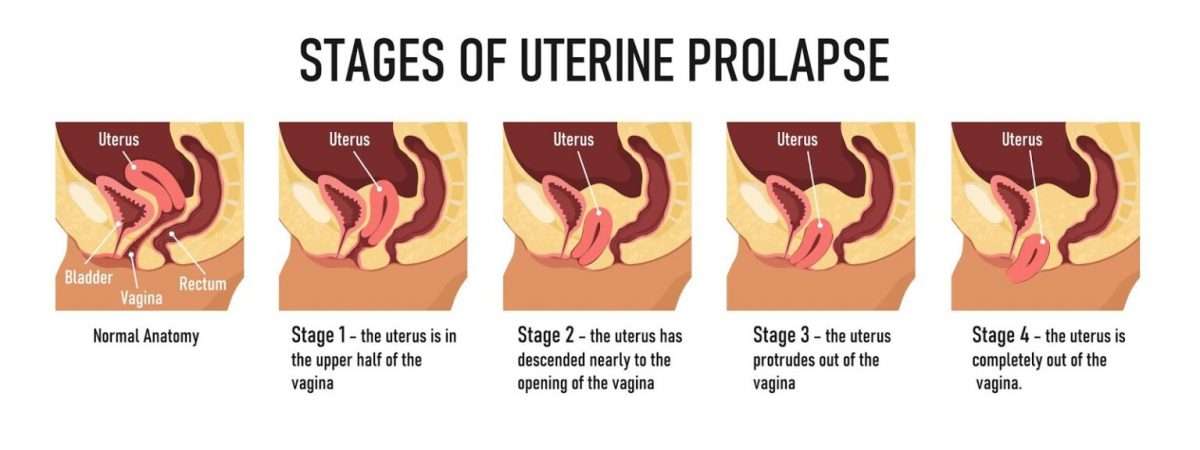
Prolapse Of The Uterus
In prolapse of the uterus, the uterus drops down into the vagina. It usually results from weakening of the connective tissue and ligaments supporting the uterus. The uterus may bulge in the following ways:
-
Only into the upper part of the vagina
-
Down to the opening of the vagina
-
Partly through the opening
-
All the way through the opening, resulting in total uterine prolapse
How far down the uterus drops down determines how severe symptoms are.
At first, prolapse of the uterus may cause mild or no symptoms. When prolapses worsens, the first symptom most women report is feeling a bulge at the opening of the vagina. They may also have pain in the lower back or over the tailbone, difficulty having a bowel movement, and pain during sexual intercourse, as well as a feeling of heaviness or pressureâa feeling that pelvic organs are dropping out.
Total uterine prolapse can cause pain during walking. Sores may develop on the protruding cervix and cause bleeding, a discharge, and infection.
Constipation Constipation in Adults Constipation is difficult or infrequent bowel movements, hard stool, or a feeling that the rectum is not totally empty after a bowel movement . (See also Constipation… read more can occur.
Are There Risk Factors
The risk of having a prolapsed uterus increases as a woman ages and her estrogen levels decrease. Estrogen is the hormone that helps keep the pelvic muscles strong. Damage to pelvic muscles and tissues during pregnancy and childbirth may also lead to prolapse. Women whove had more than one vaginal birth or are postmenopausal are at the highest risk.
Any activity that puts pressure on the pelvic muscles can increase your risk of a uterine prolapse. Other factors that can increase your risk for the condition include:
Also Check: Overactive Bladder Over Counter Medication
An Idea Of Franoise Mzires
The muscle chains were described by Françoise Mézières, a French physiotherapist. She has developed a care concept based on stretching. According to her, muscular retractions can provoke pain or further complications elsewhere in the muscle chains.
Consequently, for example, too much or insufficient flexibility can severely affect the pelvic floor and vice versa.
This list of links between the pelvic floor and the lower back pain is a non-complete list, but it helps to understand that the body is more than just a complex of independent organs. Each organ is influenced by others and the body must be seen as a whole.
What You Need To Know
- When pelvic muscle, tissue and ligaments weaken, the uterus can drop down into the vaginal canal, causing uterine prolapse.
- Nearly one-half of all women between ages 50 and 79 have some degree of uterine or vaginal vault prolapse, or some other form of pelvic organ prolapse.
- Factors that increase your risk of uterine prolapse include childbirth, age, obesity, chronic constipation and having a hysterectomy.
- Many women with uterine prolapse have no symptoms. If symptoms are present, they may include bulging in the vagina, feeling pressure in the pelvis or vagina, and lower back pain accompanied by bulging in the vagina.
- There is no definitive way to prevent uterine prolapse. Losing weight, eating a fiber-rich diet, quitting smoking and performing pelvic floor exercises can help to reduce the risk of this condition.
Don’t Miss: Natural Remedies For Cystitis Bladder Infection