What Makes Pelvic Floor Dysfunction Worse
It can take several months of routine bowel or urinary medications and pelvic floor physical therapy before symptoms of pelvic floor dysfunction start to improve. The most important part of treatment is to not give up. Forgetting to take your medications every day will cause your symptoms to continue and possibly get worse. Also, skipping physical therapy appointments or not practicing exercises can slow healing.
Any activity that increases the tension or pain in your pelvic floor muscles can cause your symptoms to get worse. For example, heavy weightlifting or repetitive jumping can increase your pelvic floor tension and actually worsen symptoms.
If you have problems with constipation due to hard bowel movements or abdominal bloating and gas pain, then you should consult with your doctor and watch your diet closely. Its important to drink plenty of water daily and eat a healthy diet. Foods that are high in fiber, or fiber supplements, may worsen your bloating symptoms and gas pains. These foods should be avoided if your symptoms get worse.
What Does A Prolapsed Uterus Feel Like
If you have a mild case of uterine prolapse, you may not have any obvious symptoms. But as your uterus slips farther out of position, it can put pressure on other pelvic organs such as your bladder or bowel and cause symptoms like:
- A feeling of heaviness, fullness or pressure in your pelvis.
- Urination problems, including leaking pee , the need to pee frequently or the sudden urge to pee .
Symptoms can get worse when you stand or walk for long periods of time or when you cough and sneeze. In these positions, gravity puts extra pressure on your pelvic muscles.
When The Bottom Falls Out: Prolapse In The Pelvis
Symptoms tend to occur when women are upright, straining, or coughing and to disappear when they are lying down and relaxing. For some women, sexual intercourse is painful.
Mild cases may not cause symptoms until the woman becomes older.
Prolapse of the rectum , small intestine , bladder , and urethra are particularly likely to occur together. A urethrocele and cystocele almost always occur together.
) or problems completely emptying the bladder .
You May Like: Active Ingredient In Azo Bladder Control
Don’t Miss: Having A Hard Time Holding My Bladder
What Are The Symptoms Of Pelvic Organ Prolapse
Mild or moderate prolapses may cause pelvic pressure, low backache, pain, or feeling that something is falling out. Urine may leak, especially with coughing, sneezing, or laughing. Rectoceles can cause bowel movement problems.
Severe prolapses also cause a feeling of fullness in the abdomen or a bulge that may go away when lying down. Other symptoms are problems emptying the bladder or having bowel movements, pelvic pain, abdominal discomfort, urgent or painful urination, and problems during sex.
How Can I Reduce My Risk Of Uterine Prolapse
Some factors like having multiple vaginal births or experiencing menopause cant be avoided.
There are ways to reduce your risk of developing a prolapse. A few lifestyle tips that can reduce your risk of prolapse include:
- Maintain a healthy weight and exercise regularly.
- Do Kegel exercises to strengthen your pelvic floor muscles.
- Stop smoking. This reduces the risk of developing a chronic cough, which can put extra strain on your pelvic muscles.
- Using proper lifting techniques when carrying heavy objects.
- Avoid becoming constipated or straining to poop.
Proper lifting techniques to avoid uterine prolapse
There are several tips for lifting heavy objects that can help you avoid injury, including:
You May Like: How To Treat A Bladder Infection
Causes Of A Prolapsed Bladder
The following factors are commonly associated with causing a prolapsed bladder:
- Childbirth: This is the most common cause of a prolapsed bladder. The delivery process is stressful on the vaginal tissues and muscles, which support a womanâs bladder.
- Straining: Lifting heavy objects, straining during bowel movements, having a long-term condition that involves coughing, or having long-term constipation may damage the muscles of the pelvic floor.
Recommended Reading: How To Stop Light Bladder Leakage
If You Have Pop Youre Not Alone
POP affects 1 in 4 women in their 40s and 1 in 3 in their 60s. By the time women reach their 80s, POP affects half of all women.
Its often caused by changes during pregnancy and childbirth that weaken the pelvic floor. But women who have never given birth can have POP too. It runs in families and can be caused by many factors, including
Other conditions and habits that strain pelvic floor muscles also can lead to POP. These include
-
ongoing constipation and straining during bowel movements
-
continual coughing caused by smoking or lung disease
-
very high-impact exercise or jobs that require heavy lifting
Don’t Miss: Chemo Treatment For Bladder Cancer
What Causes Pelvic Organs To Prolapse
Pelvic organs can start to fall out of place due to damage of the ligaments and muscles which support the pelvic organs. Damage can arise from:
- Pregnancy and childbirth which are considered major factors
- Conditions that cause excessive pressure on the pelvic floor like obesity, persistent coughing, heavy lifting and chronic constipation
- It may also occur as a result of other medical conditions that can damage the muscles, nerves and ligaments in the pelvis. In rare cases, an abdominal or pelvic mass or tumour can cause a this or make it worse
Does Ice Help Lower Back Pain Low Back Pain Bloated Abdomen Nausea
Best Weight Exercise For Lower Back Pain Lower Back Pain Hyrst When I Stand Up But Then Goes Away Does Prolapsed Bladder Cause Low Back An Pain In Stomach. Stretch Middle Back Pain Sharp Breath Taking Pain In Mid Back Left Side What Do I Do. Chronic Knees And Back Pain Sleep Apnea Cause Me To Stay In Bed Chronic Back Pain Recovery Stories. Pain In Upper Back When I Bend Over Pain Shoots To Butt Locate Upper Back Pain Chart.
Too Much Walking Lower Back Pain Lower Back Pain Is Excruciating. Is A Recliner Good For Lower Back Pain Yoga Exercises For Upper Back Pain Relief Explain Chronic Back Pain To Patients. Looking Down And Feeling Pain In Lower Back Upper Back Pain Woorsed By Swallowing.
Also Check: Why Is My Bladder Always Full
Recommended Reading: What To Avoid With Bladder Infection
What Happens At Your Appointment
Your doctor will ask if they can do an internal pelvic examination.
For this youll need to undress from the waist down and lie back on the examination bed.
Sometimes theyll ask you to lie on your left-hand side and examine you in that position to get a better view of the prolapse.
You can ask for this examination to be done by a female doctor and, if you like, bring someone you trust along with you for support.
What Medications Treat A Prolapsed Bladder
- In mild cases of prolapsed bladder, estrogen may be prescribed in an attempt to reverse bladder prolapse symptoms, such as vaginal weakening and incontinence. For more severe degrees of prolapse, estrogen replacement therapy may be used along with other types of treatment.
- Estrogen can be administered orally as a pill or topically as a patch or cream. The cream has very little systemic absorption and has a potent effect locally where it is applied.
- Topical administration has less risk than the oral preparations.
Recommended Reading: Urinary Bladder Infection Home Remedies
Other Complementary Pain Management Techniques
There are a range of other complementary and alternative pain management techniques that may be worth exploring. These include:
Biofeedback is a technique that uses machines to help you learn about and control some of your involuntary body functions. Led by a licensed technician, biofeedback may help you relax and cope with pain in your body.
Many of these integrative methods havent been tested in scientific studies on people with bladder cancer. But theyre regarded as ways to improve your quality of life when you have a disease.
Talk to your healthcare team to determine which ones might be best for your situation.
Treatment Of Pelvic Organ Prolapse

Treatment of pelvic organ prolapse is based on the womanâs symptoms. Treatment aims to improve quality of life.
Doctors start by closely monitoring the woman and her symptoms.
If symptoms are bothersome, treatment may include pelvic floor exercises, a pessary, and, if symptoms are severe, surgery. If women do not have symptoms or symptoms are mild, no treatment is needed. However, follow-up visits are needed to monitor the progression of the prolapse.
You May Like: Can T Empty Bladder Fully
How Do You Fix A Prolapsed Uterus
There are surgical and nonsurgical options for treating uterine prolapse. Your healthcare provider will pick your treatment path based on the severity of your prolapse, your general health, age and whether or not you want children in the future. Treatment is generally effective for most people. Treatment options can include:
Nonsurgical options
- Exercise: Special exercises, called Kegel exercises, can help strengthen your pelvic floor muscles. This may be the only treatment needed in mild cases of uterine prolapse. To do Kegel exercises, tighten your pelvic muscles as if youre trying to hold back urine. Hold the muscles tight for a few seconds and then release. Repeat 10 times. You may do these exercises anywhere and at any time .
- Vaginal pessary: A pessary is a rubber or plastic doughnut-shaped device that fits around or under the lower part of your uterus . This device helps prop up your uterus and hold it in place. A healthcare provider will fit and insert the pessary, which must be cleaned frequently and removed before sex.
- Diet and lifestyle: Changes to your diet and lifestyle may be helpful in relieving symptoms like constipation. Increasing your water and fiber intake may lessen how often you strain to poop. Maintaining a healthy weight for your body type puts less pressure on your pelvic muscles when you stand or walk.
Surgical options
How Serious Is A Prolapsed Uterus
Uterine prolapse can disrupt normal activities and be uncomfortable. Very mild cases may not require treatment or cause any discomfort. However, severe cases may make it difficult to pee or have a normal bowel movement. Uterine prolapse is typically a quality of life issue, and healthcare providers treat it when symptoms of the condition begin to interfere with your daily life.
Recommended Reading: Bladder Chemo Wash Side Effects
How Is Prolapse Treated
Many women with prolapse don’t need treatment, as the problem doesn’t seriously interfere with their normal activities.
Lifestyle changes such as weight loss and pelvic floor exercises are usually recommended in mild cases.
Surgery may also be an option for some women. This usually involves giving support to the prolapsed organ. In some cases, complete removal of the womb is required, especially if the womb has prolapsed out.
Most women experience a better quality of life after surgery, but there’s a risk of problems remaining or even getting worse.
Will I Need Surgery To Treat Pelvic Floor Dysfunction
There is not a surgery to treat pelvic floor dysfunction because it is a problem with your muscles. In rare circumstances, when physical therapy and biofeedback fail to work, your provider might recommend you see a pain injection specialist. These doctors specialize in localizing the specific muscles that are too tense or causing pain, and they can use a small needle to inject the muscle with numbing medication and relaxing medication. This is called trigger point injection.
Read Also: All Symptoms Of Bladder Infection
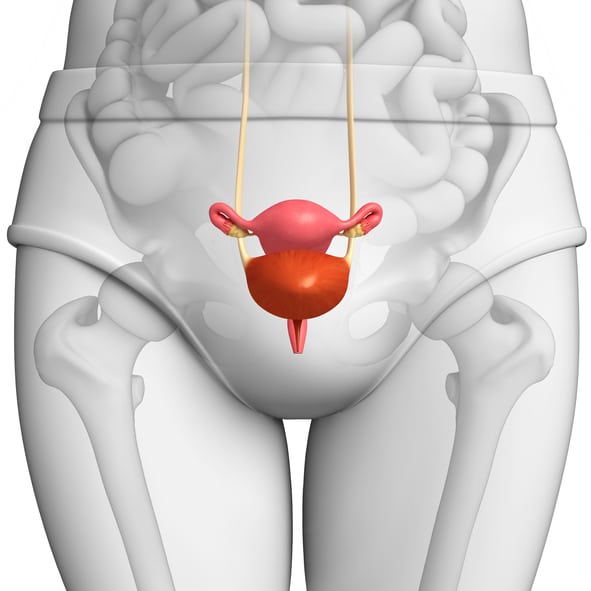
What Is Uterine And Bladder Prolapse
When the uterus sags downward, it is called uterine prolapse. When the bladder sags, it is called bladder prolapse, also known as a cystocele.
Various stresses can cause the pelvic muscles and ligaments to weaken and lead to uterine or bladder prolapse. The most significant stress on these muscles and ligaments is childbirth. Women who have had multiple pregnancies and vaginal delivery are more likely to develop prolapse.
Other stresses that can lead to prolapse include constipation with a habit of frequent straining to pass stool and a chronic cough. Obesity also can strain the pelvic muscles.
Support problems in the pelvis become worse after menopause because the pelvic tissues depend on estrogen to help them keep their tone, and estrogen levels drop after menopause.
What Is A Cystocele
A cystocele is a condition in which supportive tissues around the bladder and vaginal wall weaken and stretch, allowing the bladder and vaginal wall to fall into the vaginal canal.
A cystocele is the most common type of pelvic organ prolapse. Pelvic organ prolapse occurs when the vaginal walls, uterus, or both lose their normal support and prolapse, or bulge, into the vaginal canal or through the vaginal opening. Other nearby pelvic organs, such as the bladder or bowel, may be involved and also drop from their normal position in the body.
A cystocele occurs when supportive tissues around the vaginal wall and bladder weaken and stretch, allowing the bladder and vaginal wall to bulge into the vaginal canal.
Recommended Reading: Medicine To Treat Bladder Infection
Can Uterine Prolapse Be Prevented
There is no certain way to prevent uterine prolapse. However, the following can help lower your risk:
-
Lose weight, if youre overweight
-
Follow a diet rich in fiber and fluids to prevent constipation and straining
-
Avoid heavy lifting
-
Quit smoking, if you smoke
-
Seek prompt treatment for a chronic cough, which can place extra pressure on your pelvic organs
-
Do Kegel exercises to strengthen your pelvic floor muscles
These actions may also help if you already have uterine prolapse.
See your healthcare provider when symptoms first start to bother you. Dont wait until your discomfort becomes severe. Regular pelvic exams can help detect uterine prolapse in its early stages.
What Is Pelvic Floor Dysfunction
Pelvic floor dysfunction is a common condition where youre unable to correctly relax and coordinate the muscles in your pelvic floor to urinate or to have a bowel movement. If youre a woman, you may also feel pain during sex, and if youre a man you may have problems having or keeping an erection . Your pelvic floor is a group of muscles found in the floor of your pelvis .
If you think of the pelvis as being the home to organs like the bladder, uterus and rectum, the pelvic floor muscles are the homes foundation. These muscles act as the support structure keeping everything in place within your body. Your pelvic floor muscles add support to several of your organs by wrapping around your pelvic bone. Some of these muscles add more stability by forming a sling around the rectum.
The pelvic organs include:
Normally, youre able to go to the bathroom with no problem because your body tightens and relaxes its pelvic floor muscles. This is just like any other muscular action, like tightening your biceps when you lift a heavy box or clenching your fist.
But if you have pelvic floor dysfunction, your body keeps tightening these muscles instead of relaxing them like it should. This tension means you may have:
- Trouble evacuating a bowel movement.
- An incomplete bowel movement.
- Urine or stool that leaks.
Pelvic floor muscles
Don’t Miss: Survival Rate For Bladder Cancer Stage 4
What Is The Best Treatment For A Prolapsed Bladder
If you do have symptoms of anterior prolapse, first line treatment options include:
- Pelvic floor muscle exercises. These exercises often called Kegel exercises or Kegels help strengthen your pelvic floor muscles, so they can better support your bladder and other pelvic organs. â¦
- A supportive device .
Treatment For Symptomatic Bladder Prolapse
If you have symptoms of bladder prolapse it is recommended that, as for people with no symptoms, you make the same lifestyle changes, do pelvic floor muscle training and treat any chronic cough. Make them part of your routine.
However, sometimes prolapse can be more severe and these measures may not be enough on their own to relieve symptoms.
For these cases, there can be two different approaches:
1. Non-surgical approach vaginal pessaries
Some women may prefer this option if they wish to avoid or delay surgery, and it may be the safest option for women who are unfit for surgery.You will need regular check-ups with your healthcare professional if you are using a vaginal pessary long-term.
2.Surgical approach
In some cases, when all other management options have failed to help with the symptoms, or when a woman does not want to use a pessary, surgery may be necessary. The type of surgery used will depend on your combination of prolapse and urinary tract symptoms. Your doctor will discuss the available surgical techniques with you.It is common to have a urinary catheter inserted during the operation to rest your bladder for a day after surgery, but this will depend on the procedure you have. Recovery from surgery takes about six weeks. You doctor will advise you about how to look after yourself during the recovery period, and a physiotherapist can recommend appropriate exercises.
Suggestions may include:
- resting each day.
Read Also: Stage 5 Bladder Cancer Life Expectancy
When To Seek Help
If you are concerned you may have a prolapsed bladder and are experiencing troublesome symptoms, see your doctor. You can also visit a physiotherapist who is trained to help you with pelvic floor exercises. If you are experiencing urinary incontinence associated with a prolapse, a continence nurse adviser may help.
Surgery For A Pelvic Organ Prolapse
If you have severe bladder prolapse, surgery may be required. During surgery, a mesh support is inserted into the vaginal wall and the bladderâs position is corrected. This can be performed under general, regional or local anesthesia. Talk with your doctor for more information on surgery options and if it is required to fix your prolapsed bladder.
Also Check: Do Kegel Exercises Work For Bladder Control