A Briefhistory Of Mesh: Slings Vs Transvaginal
Inthe aftermath of the FDA ruling, mesh has become a four-letter word to most patients.But its important to remembernot all procedures that employ surgical mesh are created equal.
The FDA ban only applies to transvaginal mesh for prolapse repairs, which means there are still safe surgical options for treating POP and incontinence. These include:
- Bladder orvaginal slings: Theyve been around since the 1990s and are still consideredthe gold standard for treatment for stress urinary incontinence. Made of synthetic mesh or humantissue, the sling acts like a hammock around the urethra, preventing it fromopening during stresses on the bladder, like a laugh or a sneeze. Its placedthrough a small incision in the vagina and for women worried about leaking, its an effective option. Mostimportantly, the FDA did not ban bladder or vaginal mesh slings and it isendorsed by most female urology specialists and urogynecologists.
Vaginal Extrusion And Erosion
One of the main concerns with bladder slings has been mesh extrusion or erosion. Extrusion and erosion both refer to mesh forcing its way into the vagina, bladder, urethra or other organ. In these cases, the mesh wears through the tissues.
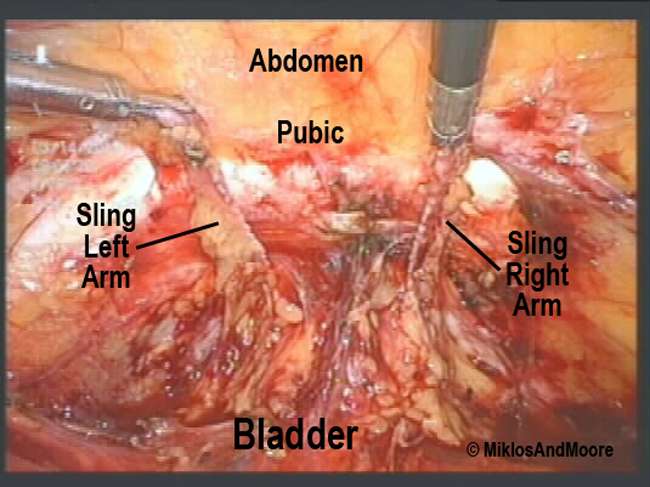
According to a paper by Dr. Cristiano Mendes Gomes and colleagues, vaginal extrusion rates vary from 0 percent to 1.5 percent for retropubic slings, which are inserted through an incision in the vagina and positioned in a U shape around the urethra. The ends of retropubic slings are maneuvered between the bladder and pubic bone and brought out through incisions above the pubic bone.
For transobturator slings, the vaginal extrusion rates vary from 0 percent to 10.9 percent, according to the paper published in Internal Brazilian Journal of Urology. Known as TOT, this procedure avoids the space between the pubic bone and the bladder. Mesh is inserted through the vagina and the ends are brought out through incisions between the labia and the creases of the thighs.
Additionally, Gomes and colleagues found urethral erosion happened after less than 1 percent of sling surgeries.
Three months postoperatively, she stated that her husband felt teeth in her vagina during sexual intercourse, Siegel wrote.
A pelvic exam revealed mesh extrusion.
In some cases, conservative management of erosion may be possible. For example, some surgeons may prescribe topical estrogen cream to help vaginal tissues heal.
Risks Of Bladder Sling Surgery
There are known risks associated with the mesh implants used in sling surgery. One of the main concerns is that pelvic meshes can break into fragments that embed into your tissue, become dislodged, and potentially perforate neighboring organs. When this happens, not only does the incontinence continue, but women experience intense pain and discomfort, often ending up worse than before the surgery. These complications frequently require followup surgeries to fix the mesh or even remove the device entirely.
In 2019, the FDA ordered a halt to the sale of transvaginal surgical mesh implants for certain pelvic procedures, and in many countries, pelvic meshes have been outlawed completely. Recently, in-depth media coverage and large class-action lawsuits have shed light on the dangers of bladder sling surgery. However, many women dont know about the alternative, nonsurgical treatment options.
Recommended Reading: Best Way To Treat Bladder Infection
Background And General Principles
In gynecologic surgery, grafts or mesh may be used when the surgical procedure requires the use of bridging material to reinforce native structures. The term graft refers to a biological material that comes from either a human or an animal . Autologous grafts can be harvested from the same person, whereas allografts come from human donors or cadavers. In gynecologic surgery, mesh refers to synthetic material . Because of complications attributed to multifilament and small-pore-size synthetic mesh, type 1 synthetic meshes currently are used in the United States. This document focuses on the management of complications related to mesh used to correct stress urinary incontinence or pelvic organ prolapse .
What Happens When A Mesh Surgery Gets Complicated
Carol, a 77-year-old Ohioan, told me that her transvaginal mesh surgery worked, but only for about 2 years. Ten years ago, when Carol met with her uro-gynecologist for an exam before the surgery, she didn’t feel like he had the best bedside manner. Still, she proceeded with the surgery. After having a hysterectomy over 30 years ago and coping with pelvic organ prolapse, Carol said her leaking problems got worse. She was tired of wearing disposables to deal with dribbles and didn’t want her prolapse to get worse. “Wearing pads got so expensive and frustrating,” she said. “I wanted to improve this problem because nothing else was working.”
But then, two years after surgery, Carol felt pain in her pelvic region. Then, she realized that she was bleeding vaginally. “The pain was excruciating,” she said. When she saw the mesh coming out, she realized that it was the source of her sudden pain.
Some women like Carol who have had transvaginal mesh have also experienced pain, bleeding, or erosion . The FDA issued warnings about it in 2008 and 2011. Finally in 2014, they released another notice stating that surgical mesh for transvaginal pelvic organ prolapse should be reclassified from a moderate-risk to high-risk surgery.
Thankfully, Carol had no scarring from her transvaginal mesh surgery, but she still copes with leakage.
Also Check: Natural Remedies For Cystitis Bladder Infection
What Is A Bladder Lift
A bladder lift involves cutting into the abdomen and lifting the neck of the bladder to return it to its typical position. This procedure corrects sagging in the urethra and bladder, so youre less likely to leak urine.
When a surgeon stitches the neck of the bladder in this lifted position to secure it to nearby structures, the procedure is referred to as colposuspension.
The surgeon may also place a midurethral sling under the urethra during the surgery. The sling acts like a hammock to support the urethra and the bladder and provide increased bladder outlet resistance.
There are two types of slings:
- Artificial sling: involves a small strap made of mesh
- Traditional sling: uses a small piece of tissue taken from your own abdomen or thigh
Bladder lift surgery typically has a high success rate, and the effects can last for several years. However, urine leakage may come back over time.
A 2019 review of studies found that overall cure rates were as high as 88 percent for colposuspension following surgery.
However, cure rate declined steadily to about 70 percent of people by 10 years after surgery. The cure rate appears to reach a plateau at 65 to 70 percent of patients at a 20-year followup.
Sling surgery is a newer procedure that seems to have similar or slightly better effectiveness as colposuspension, according to a 2021 study. More research is need on longterm performance, though.
Clinical Presentations Of Complications
Vaginal mesh exposure may be entirely asymptomatic. Alternatively, vaginal mesh exposure can produce symptoms such as spotting or bleeding, discharge, pain, or pain with sex . Persistent vaginal bleeding, vaginal discharge, or recurrent UTIs after mesh placement should prompt an examination and possible further evaluation for exposure or erosion. Pain can be constant or associated only with activity . Furthermore, pain often is complex and multifactorial and may require a multidisciplinary approach.
Don’t Miss: Homemade Cat Food For Bladder Stones
What Kind Of Surgery Is Done For Bladder Incontinence
What is sling surgery? Bladder sling surgery, also known as vaginal sling surgery or urethral sling surgery, is widely used to treat severe stress urinary incontinence . The procedure often involves implanting a piece of plastic mesh below your urethra or bladder neck in order to provide extra support.
What Happens If Your Bladder Sling Is Too Tight
If a synthetic sling is used, there is a risk that the body will reject it. Occasionally, the sling material can erode through the vaginal tissue. If this complication occurs, surgery can be done to correct the problem. With some sling procedures, more surgery may be needed to adjust the sling if it is too tight.
Don’t Miss: Best Supplements For Bladder Infection
‘scandal’ Of Vaginal Mesh Removal Rates Revealed By Nhs Records
Traumatic complications mean one in 15 women fitted with the most common type of mesh support will require surgery to extract it, figures suggest
Thousands of women have undergone surgery to have vaginal mesh implants removed during the past decade, according to NHS records that reveal the scale of traumatic complications linked to the devices.
The figures, obtained by the Guardian, suggest that around one in 15 women fitted with the most common type of mesh support later require surgery to have it extracted due to complications.
Sohier Elneil, a consultant urogynaecological surgeon at University College Hospital, London, who has carried out hundreds of removal procedures, described the removal rate as a scandal, adding that these patients were likely to represent those with more serious complications.
Another surgeon, Mark Slack, a consultant gynaecologist at Addenbrookes Hospital Cambridge, who has previously defended the benefits of mesh surgery, said he was absolutely shocked by the failure rate, although he questioned whether the figures for complete removals could be an overestimate.
The implants have been widely used as a simple, less invasive alternative to traditional surgical approaches for treating urinary incontinence and prolapse, conditions that can commonly occur after childbirth. For the majority of women the operation is successful.
My Bladder Sling Failed Now What
Bladder leakage must rank as one of the most frustrating of problems. The gradual worsening and escalation from panty liners to pads to diapers feels like a most unwelcome sign of the body breaking down.
Paying attention to the nearest bathroom at all times becomes exhausting. And waking up during the night because the bladder needs attention means a distinct drop in quality of life.
Ive shared before that many doctors are unaware of the most effective treatment for incontinence. Instead, their patients get recommendations to manage fluids, practice pelvic floor exercises, take daily medications, or undergo surgical procedures like the bladder sling. But what happens when it fails?
Read Also: What Do They Do For Bladder Cancer
Can Bladder Slings Be Removed
If women start to experience complications from their transvaginal mesh products, they may be able to have the mesh removed.
According to the University of Colorado, transvaginal mesh is intended to be a permanent implant and is often difficult to remove. After implanting the mesh, the body heals by growing tissue into and around the implant. This can reportedly make it difficult to remove the mesh entirely without damaging a womans pelvic organs or tissue.
Mesh erosion is reportedly one of the most common complications associated with bladder slings, but may be treated with removal. If the erosion is minor, the procedure may be able to be conducted in an outpatient setting. However, if mesh exposure is more than 5 mm, a full operation may be required.
Unfortunately, it may take more than one surgery to remove the mesh. As mentioned above, bladder slings may become integrated with pelvic tissue which can make it difficult to remove. The type of surgical approach used to implant the mesh is also important as this can dictate what parts of the mesh can be removed effectively.
Although mesh removal can help women when they are experiencing bladder sling complications, there are always risks associated with the procedure or surgery. Due to these risks, doctors may instead advocate for a observational approach unless severe complications occur such as infection, fistula, or chronic pain.
What You Should Know About The Reversal Of Transvaginal Mesh Surgery

Transvaginal mesh is often offered as a solution for women who suffer from urinary incontinence. This procedure entails the implanting of mesh made from synthetic propylene to fix pelvic floor prolapse and stress urinary incontinence.
Although the procedure sounds non-invasive and simple on paper, the statistics tell an entirely different story. During the past couple of years, the transvaginal mesh procedure has come under the spotlight and several lawsuits have been filed.
Common complaints were that it caused severe pain and discomfort, didnt stop urinary incontinence despite being a costly procedure, and that it causes damage to the nerves around the bladder and the urethra.
Severe side effects
Other frequently reported side effects include infection, bleeding, pain during intercourse and the exposure of the mesh through the vagina. Vaginal scarring was also reported by the FDA.
Because of the severity of these side effects, many patients who underwent transvaginal mesh implants wish to reverse the surgery. Luckily, a procedure named transvaginal mesh excision makes this possible.
According to The Guardian, thousands of women who underwent the surgery have had their transvaginal mesh implants removed. According to the publication, this means that one in 15 women who opted for transvaginal mesh implants will eventually opt to reverse the procedure.
What does the procedure entail?
What makes this procedure difficult?
Is the removal safe?
R75 per month
Also Check: What Causes Weak Bladder In Females
Do Bladder Slings Need To Be Replaced
If your bladder sling is placed improperly or shifts over time, it may need to be removed or replaced. As with any operation, its important to weigh the pros and cons, and consult your doctor for advice. For many women, bladder sling surgery provides powerful relief to chronic stress-induced incontinence, and can be a safe, minimally invasive procedure.
What Are The Side Effects Of A Bladder Sling
While most patients experience few side effects, there are always risks involved with any surgery. If you experience bloating after bladder sling surgery, the placement may be off, and you should consult your doctor. Other complications include prolonged abdominal pain, painful intercourse and urinary tract infection. There is also a small chance that the mesh material could begin to erode through your tissue or become exposed.
You May Like: Can Candida Cause Bladder Infection
General Principles Of Management Of Mesh And Graft Complications
Approaches to management of mesh-related complications in pelvic floor surgery include observation, physical therapy, medications, and surgery. Table 1 presents an overview of specific mesh and graft complications and management options. There may be settings in which observation of exposed mesh is reasonable 4. Surgical intervention or referral is not always necessary for type 1 mesh exposures into the vagina. Asymptomatic exposures of monofilament macroporous meshes can be managed expectantly. For women with symptoms, a trial of vaginal estrogen can be attempted for small mesh exposures. Topical estrogen may improve or resolve the mesh exposure, though there is little prospective, comparative evidence supporting this approach. A period of 612 weeks is a reasonable period to try topical estrogen.
One multicenter study of mesh complications after reconstructive surgery found that 60% of women required two or more interventions and that the first intervention was surgical in approximately one half of cases 5. These procedures are complex and should be approached with caution. Surgeons who are unfamiliar with the original index procedure or the management issues that follow should refer the patient to a surgeon who is familiar with these types of repairs.
Frequently Asked Questions About Slings
Q: What is stress urinary incontinence and is it a common problem?A: Stress urinary incontinence is loss of urine that occurs at the same time as physical activities that increase abdominal pressure . These activities can increase the pressure within the bladder, which behaves like a balloon filled with liquid. The rise in pressure can push urine out through the urethra, especially when the support to the urethra has been weakened this is what we call stress urinary incontinence. Approximately 1 out of 3 women over the age of 45, and 1 out of every 2 women over 65 have SUI.
Q: What are surgical treatment options for stress urinary incontinence?A: Surgeons have developed different techniques for supporting the bladder back to its normal position. The three main types of surgery are: retropubic suspension and two types of sling procedures.
Retropubic suspension uses surgical threads called sutures to support the bladder neck. In this operation, the surgeon makes an incision in the abdomen a few inches below the navel and then secures the threads to strong ligaments within the pelvis to support the urethral sphincter. This common procedure is often done at the time of an abdominal procedure, such as a hysterectomy.
Q: Has the FDA recalled slings?A: No, the FDA has not recalled slings.
You May Like: How To Take Care Of A Bladder Infection At Home
What Are The Different Types Of Sling Surgery
The two most common types of bladder slings are midurethral and traditional. Midurethral: This sling is inserted during an outpatient procedure that only takes about 30 minutes. Typically, a strip of synthetic mesh is inserted through a single incision in your vagina, and cradles the urethra like a hammock. The procedure may also involve a retropubic method in which two additional incisions are made near the pubic bone to secure the mesh.The transobturator method is another midurethral option in which small incisions are made in the vagina and the labia to secure your sling.Traditional: A traditional, or conventional, bladder sling is inserted during an inpatient procedure, which means you will likely spend a night in the hospital afterward. Traditional bladder sling surgery may use synthetic mesh, or tissue from your own body . With this method, one incision is made in your vagina and one in your belly, in order to connect the sling using tension under the bladder neck. Conventional bladder sling recovery can take longer and may involve more complications.
How Painful Is Bladder Lift Surgery
Bladder lift surgery is often done laparoscopically.
This means that a surgeon will make just a few small cuts in the abdomen during the surgery. To perform the surgery, theyll use a small camera and tools inserted through tubes placed in the cuts.
Laparoscopic procedures are less invasive than open surgery. Recovery time for midurethral sling surgery and colposuspension performed laparoscopically is often much quicker than for open surgery.
Youll most likely leave the hospital after your surgery to recover at home. In some cases, though, you may need to stay overnight.
On the other hand, a traditional sling surgery and colposuspension with abdominal surgery usually require that you stay in the hospital to recover for a few days.
You may feel some pain or cramping in your lower abdomen and may need to take pain medications for 1 or 2 weeks. Most people fully recover from this procedure in about 6 weeks.
As with any surgery, bladder lift surgery comes with some risks. These include:
- bleeding
Don’t Miss: How Do Doctors Test For Bladder Infection