Is Bowel Cancer Hereditary
If you develop bowel cancer before the age of 50, there is a chance you have Lynch syndrome. The medical name for Lynch syndrome is hereditary non-polyposis colorectal cancer . It is thought this is a result of several potential inherited gene mutations. Alternatively, if there are a cluster of cases of bowel cancer in a family if could be a condition called familial adenomatous polyposis .
However, hereditary bowel cancers are relatively uncommon. The NHS note that these two inherited conditions are considered rare.
Also Check: Bladder Infection Without Painful Urination
Chris Was Grateful To Have His Own Room The Hospital Was Clean And Bright And Was A Good
EMBED CODEYou say cleanliness, were the loos fairly clean?So you were lucky enough to have your own room?But this was National Health Service?
In a few cases recovery was disrupted by a major setback. Usually this was a medical complication but one woman had an unfortunate experience when her wound broke down and hospital staff failed to respond promptly.
After Surgery Chris Had A Catheter When It Was Removed He Found It Impossible To Pass Urine So
EMBED CODEWhat did you do? Did you strap the catheter and the bag to you, under your trousers to your leg? EMBED CODEEMBED CODE
A number of people developed adhesions after surgery and experienced extreme distress in addition to physical pain because they did not understand what was happening to them. One man’s adhesions caused a blockage of the bowel which required emergency surgery. One woman had learned to detect the signs of an attack in its early stages and used steroids to prevent it coming on. The majority of people who discussed adhesions felt they should have been warned about them in advance. One woman felt that her consultant had downplayed discussion of adhesions and that this had been unhelpful to her.One man experienced sexual dysfunction as a result of his surgery and had to seek counselling to help him deal with it. He felt strongly that this risk should have been discussed with him before surgery.
Read Also: Is Bladder Incontinence A Disability
What Are The Risks Of A Laminectomy
As with any surgical procedure, complications can occur. Some possible complications may include:
- Blood clots in the legs or lungs
- Spinal cord or nerve root injury
- Risks linked to the use of general anesthesia
Nerve or blood vessels in the area of surgery may be injured. This can cause weakness or numbness. The pain may not be eased by the surgery or may become worse, although this is rare.
There may be other risks depending on your specific health condition. Be sure to discuss any concerns with your healthcare provider before the surgery.
Why Might A Person With Cauda Equina Syndrome Become Incontinent
The cauda equina nerves supply muscle sensation to the bladder, bowel and legs. When these nerves become suppressed from Cauda Equina Syndrome then muscle sensation becomes lost which can result in loss of bladder and/ or bowel control.
Common incontinence conditions include
- Urinary retention
- Loss of bladder and bowel sensation
Most cases of Cauda Equina Syndrome require emergency surgery to decompress the nerves and prevent permanent damage and loss of sensation to the bladder and bowel.
If you are experiencing symptoms of Cauda Equina Syndrome it is important to seek help straight away in order to receive treatment as soon as possible. It has been proven that if surgery takes places within 48 hours of symptoms that for many sensation and bladder and bowel control can be restored.
Further information and downloads can be found in the help & information section. Living with a bladder or bowel condition or caring for someone with a bladder and bowel condition can affect you emotionally and socially sometimes it can help to speak to others who understand your situation.
There are many ways you can find help on this site, including our which is a moderated space for peer support and discussion.
Also Check: How Many Radiation Treatments For Bladder Cancer
Surgery For A Colovesical Fistula
When conservative therapy is not appropriate or effective, youll need surgery. A surgeon can remove or repair the fistula and stop the exchange of fluids between the colon and bladder.
The cause, severity, and location of the fistula will determine which type of surgery is used to treat it. Since colovesicular fistulas are found most commonly between the sigmoid colon and bladder, doctors often perform a kind of surgery known as a sigmoid colectomy.
This surgery involves the removal of part of the sigmoid colon, the last section of the colon. The procedure also includes removal of the fistula itself and a patching up of the colon and bladder.
What Causes Cauda Equina Syndrome
Cauda equina syndrome is caused by significant narrowing of the spinal canal that compresses the nerve roots below the level of the spinal cord. Numerous causes of cauda equina syndrome have been reported, including traumatic injury, disk herniation, spinal stenosis, spinal tumors , such as metastatic tumors, meningiomas, schwannomas, and ependymomas, inflammatory conditions, infectious conditions, and accidental causes by medical intervention .
Trauma
- Traumatic events leading to fracture or partial dislocation of the low back result in compression of the cauda equina.
- A collection of blood surrounding the nerves following trauma in the low back area can lead to compression of the cauda equina.
- Penetrating trauma can cause damage or compression of the cauda equina.
- A rare complication of spinal manipulation is partial dislocation of the low back that can cause cauda equina syndrome.
Herniated Disk
Spinal Stenosis
- Spinal stenosis is any narrowing of the normal front to back distance of the spinal canal.
- Narrowing of the spinal canal can be caused by a developmental abnormality or degenerative process.
- The abnormal forward slip of one vertebral body on another is called spondylolisthesis. Severe cases can cause a narrowing of the spinal canal and lead to cauda equina syndrome .
Tumors
Dont Miss: How To Prevent Bladder Infection After Intercourse
Don’t Miss: What Does The Start Of A Bladder Infection Feel Like
How Is A Pinched Nerve Diagnosed
Weakness, tingling and numbness, and pain are all warning signs that you may be suffering from a pinched nerve. Constant pain is very unpleasant and can stop you from going to work or engaging in your day-to-day activities.The symptoms tend to worsen without treatment, so make sure to contact the experts at NJSO to help you take charge of your health with a custom-tailored treatment plan.
Anastomotic Leakage: Risk Factors Diagnosis And Treatment
Anastomotic leakage is the most serious complication specific to intestinal surgery and ranges from 2.9% to as high as 15.3%. At least one third of the mortality after colorectal surgery is attributed to leaks. Within this context, knowledge of factors influencing anastomotic healing appear even more important . However, there is lack of a clear definition for what constitutes an anastomotic leak .
Another multivariate analysis showed that American Society of Anaesthesiologists Grade III to V and emergency operation were independent factors associated with anastomotic leakage. The risk of anastomotic leakage was 8.1% if both factors were present .
There seems to be no significant difference in leakage when comparing a handsewn and a stapled technique regardless of the level of anastomosis . Intraoperative problems and postoperative strictures seem to be more frequent in stapled anastomosis . However, in a recent Cochrane review ileocolic stapler anastomoses were associated with fewer leaks than handsewn anastomoses .
The available data comparing the anastomotic leakage rate in laparoscopic or open operated patients showed no difference regardless of the level of the anastomosis . In cancer patients anastomotic leakage is associated with poor survival and a higher recurrence rate after curative resection .
Recommended Reading: Can Breast Cancer Metastasis To Bladder
Diagnosis Of Anastomotic Leakage
Because of the severity of the complications associated with an anastomotic leak, it is imperative to identify the problem and act as early as possible. Most groups base the diagnosis on clinical symptomatic leakage, manifested as gas, purulent or fecal discharge from the drain, purulent discharge from the rectum, pelvic abscess or peritonitis. It is usually necessary to obtain objective tests of anastomotic integrity because of the non-specific clinical signs. Water soluble enemas or CT scans are widely used for diagnosis of anastomotic leak. Interestingly, in two recent studies anastomotic leaks were more often diagnosed late in the postoperative period and more often after hospital discharge, or 12 days postoperatively .
Bowel Changes After Treatment
Treatment for bowel cancer can cause changes to how your bowels work. Changes can include how often you poo, how urgently you need to go, and difficulty emptying your bowel completely.
These effects usually improve in the weeks and months after you finish treatment. But sometimes they might go on for longer and can be difficult to live with. There are things you can do to help you manage these changes.
The bowel changes you have after treatment will depend on a number of factors. These include what operation you have, which part of your bowel the surgeon removes and any other treatments you have. Your doctor or nurse will tell you more about what to expect after treatment and help you manage any bowel changes.
Read Also: Bladder Cancer Metastasis To Lung Symptoms
Treatment Options For A Colovesical Fistula
The preferred treatment for a colovesical fistula is surgery.
Conservative treatment, which is nonsurgical, may be reserved for people who cannot tolerate the surgical procedure or who have extensive unresectable cancer. If a cancer is unresectable, that means it cannot be removed through surgery.
Conservative treatment may include:
- antibiotics and corticosteroids
- having a catheter inserted into the bladder to drain fluid that may have seeped into it from the colon
The goal of conservative treatment is for the fistula to close and heal on its own. However, surgery may still be necessary in cases where the fistula does not heal on its own.
Because colovesical fistula may be a complication of diverticulitis, make sure you follow the doctors orders in treating diverticular disease. In some cases, medications are enough to stop the progression of diverticulitis.
Long Term And Late Side Effects
The side effects of treatment usually get better over time. But some people may have side effects that carry on for more than six months or that start months or years after theyve finished treatment .
Speak to your healthcare team if any side effects are not getting better or if you are having any new problems. The team can offer treatment and support.
People cope with side effects in different ways. Things that people with cancer say have helped them include:
- Changing their work-life balance
- Changes in bladder function
Read Also: Difference Uti And Bladder Infection
Urinary And Sexual Dysfunction
Autonomic nerves can be damaged during total mesorectal excision. Dissection along the avascular plane between presacral fascia and mesorectal fascia, the so called holy plane, preserves sacral vessels and autonomic nerves including the superior hypogastric plexus, the hypogastric nerves, the pelvic plexus, the pelvic splanchnic nerves, and the neurovascular bundle of Walsh. However, the presence of urinary and sexual dysfunction among patients who underwent an anterior resection, as a result of thermal and/or ischemic injury, tension or local inflammatory damage of autonomic nerves is well recognised. Special attention must be paid during dissection at the origin of the inferior mesenteric artery, during the posterior mobilization of the rectum and lateral and anterior dissection of the rectum to minimise risk of nerve injury.
Due to sympathetic and parasympathetic nerve damage, patients describe incomplete urination, frequency of urination, interrupted urination, incontinence and low-flow urination. Urinary dysfunction may be easily evaluated with the International Prostate Symptom Score, which includes assessment of urinary symptoms and patients QOL. Utilizing this scoring system, data suggest 12.7% of patients suffer from severe dysfunction after rectal resection.
She Failed To Receive Prompt Attention When Her Wound Broke Down After Surgery
The speed of recovery varied greatly from person to person. One man’s GP said he was ‘like Rasputin’, stick a knife in him and he jumps up again’. A woman described her consultant’s amazement at finding her ‘sitting bolt upright in bed with her heated rollers in and her make-up on 2 or 3 days after surgery. For another woman, however, recovery was a slow and painful process.
Also Check: What Foods Cause Bladder Infections
What Could Have Caused Her Incontinence Problems
Urinary incontinence after rectal cancer treatment may consist of urge, overflow, and/or stress incontinence. Urge incontinence may result from a reduced bladder capacity due to surgical disruption of the sympathetic nerve supply . Overflow incontinence may be caused by surgical damage to the sacral splanchnic nerves, resulting in bladder emptying problems . However, the present patient suffered from involuntary urine loss during increased abdominal pressure, which is a sign of urinary stress incontinence. Stress urinary incontinence may result from impaired support to the urethra and bladder neck. This support is regulated by surrounding structures, the most important being the pubourethral-vesical ligaments, the suburethral vaginal wall, the levator plate, the pubococcygeus muscles, and the connective tissue. These components can compensate for each other in case of inappropriate function. In post-menopausal female patients, many of these structures are impaired because their function is influenced by oestrogen receptors. Additional changed anatomical relations between bladder, urethra, and pelvic floor, and possibly damage to the innervation of the levator ani muscles during LAR, would further impair the continence mechanism and lead to urinary incontinence .
Yellow: hypogastric nerves green: pelvic splanchnic nerves red: pelvic plexus blue: levator ani nerve. Adapted from: Lange JF Surgical anatomy of the abdomen. Maarssen : Elsevier. p. 178.
When To Contact Your Healthcare Provider
Contact your healthcare provider if:
- You have a fever of 100.5 °F or higher.
- You have pain in your abdomen, nausea, and vomiting.
- You have any of the following signs of infection in your incision:
After 5:00 p.m., during the weekend, and on holidays, call and ask to speak to the person on call for your healthcare provider.
Don’t Miss: Urine Test For Bladder Infection
Lower Back Pain May Be Caused By Bowel Problems
Problems of the lower back may be related to bowel problems or painful and swollen bowels. Back pain and piercing or nagging pain in the abdomen may be attributable to swollen bowels and flatulence.
For all kinds of reasons, the stomach may feel uncomfortable and cause back problems at the same time. In turn, back problems may cause abdominal pain. The nerves of both regions run lumbar . So, they have considerable impact on each other.
Living With Bowel Changes
Being prepared when you go out
One of the hardest things about having diarrhoea is that it can sometimes happen very suddenly. To avoid or cope with accidents when you go out, you can help to prepare yourself:
- know exactly where the toilets are in the place you are going
- contact the Bladder and Bowel Community or Pelvic Radiation Disease Association for a ‘Just can’t wait’ card to give you quick access to public toilets
- take spare underwear, pads, soothing creams and a plastic bag with you, just in case
Gentle exercise
Regular exercise helps to keep your bowel working normally.
Side effects from your cancer and its treatment can make it difficult to exercise. You might feel that you dont have the energy for it. But a little exercise is better than none.
A short walk each day may make all the difference to keeping your bowel motions soft and regular. Exercise has also been shown to increase energy levels, so you may gradually feel better and be able to do a little more.
Support and information
You may feel quite isolated and find it difficult to talk to people. Our bowels and going to the toilet are very private matters for many people. But the staff at the hospital or clinic are very used to talking about these things and so you don’t need to feel embarrassed. It is up to you who you decide to talk to.
They might refer you to a specialist such as a continence specialist or doctor who specialises in the digestive system .
Also Check: Heal Bladder Infection Without Antibiotics
Causes Of Bladder And Bowel Problems
Some types of cancer treatment can cause bladder and bowel side effects. These side effects are common after pelvic radiotherapy or treatment for bowel cancer. They may also be caused by the drugs you are taking as part of your treatment for cancer.
- passing urine more often than usual
- passing urine during the night
- a burning feeling when you pass urine
- a feeling that you are not able to wait when you need to pass urine
- blood in your urine
- leaking small amounts of urine .
Contact the hospital straight away if:
- your symptoms get worse
- you have a high temperature
- you feel you cannot pass urine.
Your healthcare team may ask you for a urine sample to check if you have an infection. An infection is a common cause of symptoms and is easy to treat. If the problems do not improve within a few weeks, they may arrange tests. Or they may get more advice for you from a continence specialist.
People often feel embarrassed talking about bladder problems. But if you tell your team, they can help, and it is usually possible to improve it.
- loose stools or diarrhoea
- hard stools or constipation
- needing to empty your bowel urgently
- cramping pains in your tummy or back passage
- passing a lot of wind.
Rectovaginal And Colovesical Fistulas
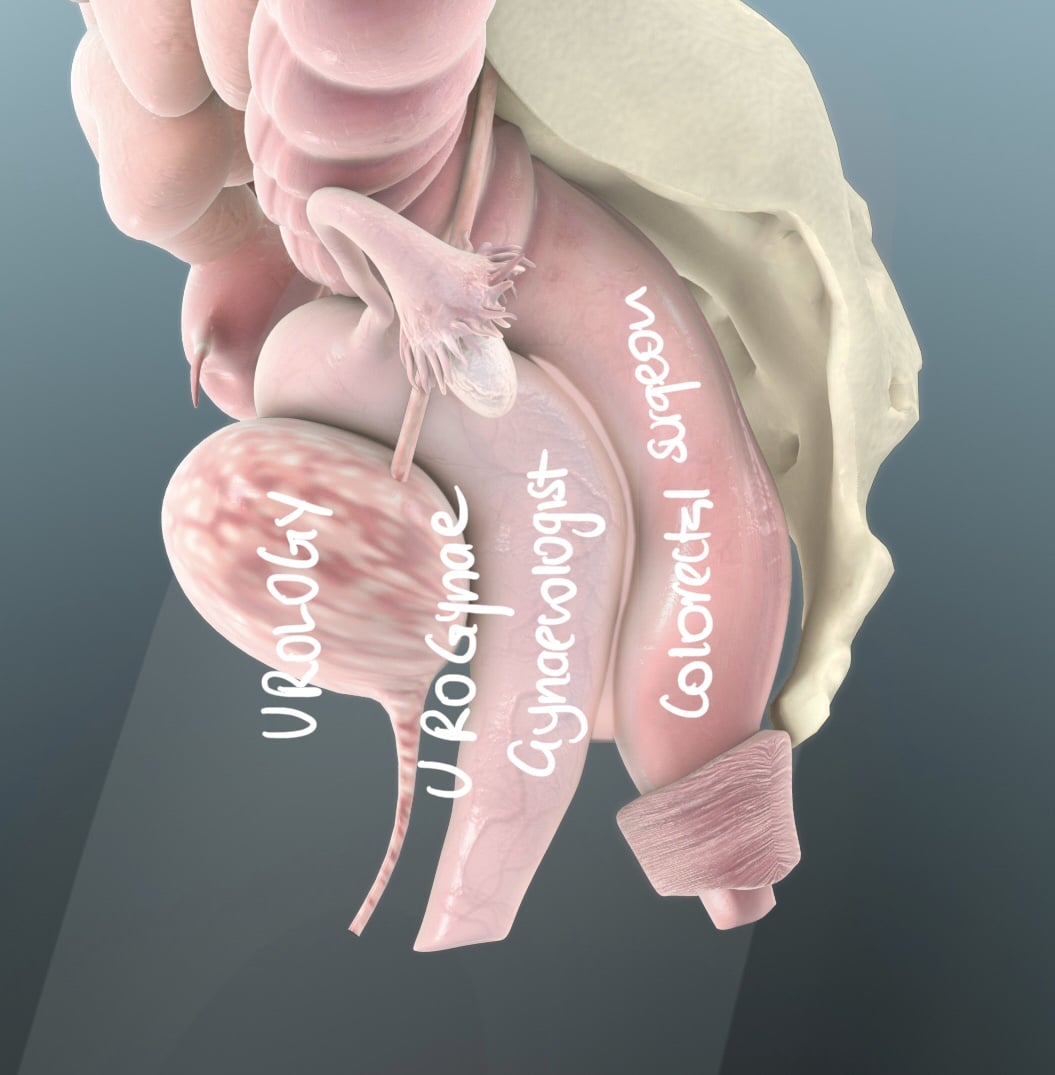
Some authors suggest that the persistence of an AL, even when there is a discrete sinus could be associated to a rectovaginal/rectourethral/colovesical fistula, or also to some degree of stenosis, recommending early repair of AL in order to avoid these complications. Urinary sepsis and the presence of gas in the bladder in absence of catheterisation raise suspicion of colovesical fistula .
Figure 2. Colovesical fistula in a patient undergoing laparoscopic anterior resection. Air in the bladder in the absence of catheterisation
Don’t Miss: Is Cystitis A Bladder Infection