Treating Bladder Cancer That Progresses Or Recurs
If cancer continues to grow during treatment or comes back after treatment , treatment options will depend on where and how much the cancer has spread, what treatments have already been used, and the patient’s overall health and desire for more treatment. Its important to understand the goal of any further treatment if its to try to cure the cancer, to slow its growth, or to help relieve symptoms as well as the likely benefits and risks.
For instance, non-invasive bladder cancer often comes back in the bladder. The new cancer may be found either in the same place as the original cancer or in other parts of the bladder. These tumors are often treated the same way as the first tumor. But if the cancer keeps coming back, a cystectomy may be needed. For some non-invasive tumors that keep growing even with BCG treatment, and where a cystectomy is not an option, immunotherapy with pembrolizumab might be recommended.
Cancers that recur in distant parts of the body can be harder to remove with surgery, so other treatments, such as chemotherapy, immunotherapy, targeted therapy, or radiation therapy, might be needed. For more on dealing with a recurrence, see Understanding Recurrence.
Locally Advanced Bladder Cancer
Locally advanced bladder cancer means your cancer has grown through the muscle layer of your bladder into the fat layer. Or it has spread to nearby lymph nodes. It hasnt spread to other parts of your body.
You usually have a combination of chemotherapy drugs.
You might have surgery or radiotherapy after your chemotherapy if your doctor thinks these treatments are suitable. Your team will talk to you before you start treatment and discuss whether they think this might be a possibility.
Localised Invasive Bladder Cancer
Localised invasive bladder cancer means your cancer has grown into, but not through, the muscle layer of your bladder. It hasnt spread to your lymph nodes or to other parts of your body.
Your doctor will offer you chemotherapy with a combination of drugs if its suitable for you. This is called neoadjuvant chemotherapy. You then have either:
- surgery to remove your bladder
- radiotherapy combined with drugs that make it work better
You might have chemotherapy after surgery if you didnt have it before and your doctor thinks there is a high risk of your cancer coming back.
Read Also: I Have A Weak Bladder Help
What Is Bladder Cancer
The bladder, a hollow organ in the lower part of the abdomen, serves as a reservoir for urine until it is discharged out of the body through the urethra.
There are different types of bladder cancer. The cancer cell type can be transitional cell carcinoma, squamous cell carcinoma or adenocarcinomaeach named for the types of cells that line the wall of the bladder where the cancer originates.
- Most bladder cancers start from the transitional cells, which occupy the innermost lining of the bladder wall. The cancers, which originate in these cells lining the bladder can, in some instances, invade into the deeper layers of the bladder , the thick muscle layer of the bladder, or through the bladder wall into the fatty tissues that surround the bladder.
- Squamous cells are thin flat cells that line the urethra and can form in the bladder after long bouts of bladder inflammation or irritation. Squamous cell carcinoma makes up about 5 percent of bladder cancers.
- Adenocarcinoma is a very rare type of bladder cancer that begins in glandular cells in the lining of the bladder. Only 1 percent to 2 percent of bladder cancers are adenocarcinoma.
After Bladder Cancer Has Been Diagnosed Tests Are Done To Find Out If Cancer Cells Have Spread Within The Bladder Or To Other Parts Of The Body
The process used to find out if cancer has spread within thebladder lining and muscle or to other parts of the body is called staging. The information gathered from the staging process determines the stage of the disease. It is important to know the stage in order to plan treatment. The following tests and procedures may be used in the staging process:
You May Like: Intravesical Chemotherapy For Bladder Cancer
Clinical Trials To Improve Treatment
Your doctor might ask if youd like to take part in a clinical trial. Doctors and researchers do trials to make existing treatments better and develop new treatments.
-
BMJ Best Practice. Bladder CancerD Lamm and others
-
National Institute for Health and Care Excellence , February 2015
-
EAU Guidelines on Muscle-invasive and Metastatic Bladder CancerJ A Witjes and othersEuropean Association of Urology, 2017
-
Bladder cancer: ESMO Practice Guidelines for diagnosis, treatment and follow-up J Bellmunt and others
Carcinoma In Situ Of The Bladder
Carcinoma in situ of the bladder was first described in 1952 by Melicow . The diffuse nature of CIS was demonstrated in a subsequent report of 30 cases in which CIS extended from the renal pelvis to the penile urethra . Carcinoma in situ may occur as a primary disease, in association with papillary or solid tumors, or following tumor resection.
Irritative symptoms are common in patients with primary or concurrent CIS . Hematuria also is a frequent presenting feature. Urinary cytology is positive in more than 90% of patients with CIS and is an important diagnostic procedure because cystoscopic findings and even bladder biopsy may be falsely negative.
Clinical Course
The clinical course of CIS is highly variable, but overall, prior to the advent of BCG immunotherapy, 54% of patients progressed to muscle-invasive disease . Extensive, diffuse disease is considered to pose an increased risk for progression, whereas focal disease may exist for years and has a reported incidence of progression as low as 8% .
Focal CIS is the earliest stage in the evolution of invasive bladder cancer, and although its course is often protracted, regression virtually never occurs. Patients with focal disease are optimal candidates for intravesical therapy.
Radiation and Systemic Chemotherapy
Intravesical Chemotherapy
Don’t Miss: Home Remedies For Bladder Infection In Women
Permission To Use This Summary
PDQ is a registered trademark. The content of PDQ documents can be used freely as text. It cannot be identified as an NCI PDQ cancer information summary unless the whole summary is shown and it is updated regularly. However, a user would be allowed to write a sentence such as NCIs PDQ cancer information summary about breast cancer prevention states the risks in the following way: .
The best way to cite this PDQ summary is:
PDQ® Adult Treatment Editorial Board. PDQ Bladder Cancer Treatment. Bethesda, MD: National Cancer Institute. Updated < MM/DD/YYYY> . Available at: . Accessed < MM/DD/YYYY> .
Images in this summary are used with permission of the author, artist, and/or publisher for use in the PDQ summaries only. If you want to use an image from a PDQ summary and you are not using the whole summary, you must get permission from the owner. It cannot be given by the National Cancer Institute. Information about using the images in this summary, along with many other images related to cancer can be found in Visuals Online. Visuals Online is a collection of more than 3,000 scientific images.
Bcg Immunotherapy For Transitional
Donald L. Lamm, MDOncology
Prior to the advent of BCG immunotherapy, bladder carcinoma in situ often progressed to muscle invasion. Intravesical chemotherapy completely eradicates the disease in 50% of patients, but fewer than 20% remain disease free after 5 years. Complete responses have been reported in 70% or more of BCG treated patients, nearly two-thirds of which are durable.
Prior to the advent of BCG immunotherapy, bladder carcinoma in situ often progressed to muscle invasion. Intravesical chemotherapy completely eradicates the disease in 50% of patients, but fewer than 20% remain disease free after 5 years. Complete responses have been reported in 70% or more of BCG treated patients, nearly two-thirds of which are durable. Controversy over the optimal induction and maintenance regimens for BCG immunotherapy remain, but SWOG investigators have demonstrated that complete response rates can be increased from the expected 73% to 87% with just three additional BCG instillations given at 3 months. In complete responders, maintenance BCG using three weekly treatments at 6-month intervals improves long-term complete response rates from 65% to nearly 90%. Caution must be exercised to avoid serious side effects.
Recommended Reading: Complete Loss Of Bladder Control
Choosing Between Surgery And Radiotherapy
Your doctor might ask you to choose between surgery to remove your bladder or radiotherapy if both treatments are suitable for you.
But they might not recommend radiotherapy if:
- you have squamous cell bladder cancer
- there is carcinoma in situ in much of the bladder lining as well as invasive cancer
- initial chemotherapy is not working
- the cancer is blocking one or both of the tubes that carry urine into the bladder from the kidneys
Talk to your specialist about the risks and benefits of surgery or radiotherapy for you. They will discuss your treatment options with the multidisciplinary team.
You may need to meet with one or more of the specialists in the team to discuss your options. You make the final decision about which treatment you have.
Relevance Of The International Bcg Shortage To The Aua Guidelines
The global shortages in TICE BCG that occurred in 2014 and 2019 led the AUA to recommend several management strategies to maintain high quality care for patients with NMIBC. These recommendations may supersede the guideline statements below. In particular, the BCG shortage impacts guideline statements 17, 20, and 21. The AUA Statement on the BCG Shortage is available at .
Don’t Miss: What Is The Best Treatment For Bladder Cancer
Bladder Reconstructions And Stomas
If you have had your bladder removed, the way you pass urine will change. There are several options that your treatment team will talk to you about:
- Urostomy is where doctors create a new hole in your abdomen called a stoma. Urine drains from the stoma to the outside of your abdomen into a special bag.
- Neobladder is where a new bladder made from your small bowel forms a pouch inside your body to store urine. You will pass urine by squeezing your abdominal muscles. You will also pass a small tube into the neobladder each day to help drain the urine.
- Continent urinary diversion is a pouch made from your small bowel inside your body to store urine. The urine empties through a hole called a stoma to the outside of your abdomen into a special bag.
A bladder reconstruction is a big change in your life. You can speak with a continence or stomal therapy nurse for help, support and information. You can also call Cancer Council . You may be able to speak with a trained Cancer Council volunteer who has had cancer for tips and support.
If you find it difficult to adjust after your bladder reconstruction, it may help to be referred to a psychologist or counsellor.
Note: If you have a stoma, you can join a stoma association for support and free supplies. For more information about stoma associations, visit the Australian Council of Stoma Associations.
Advances In Diagnosis Of Cis
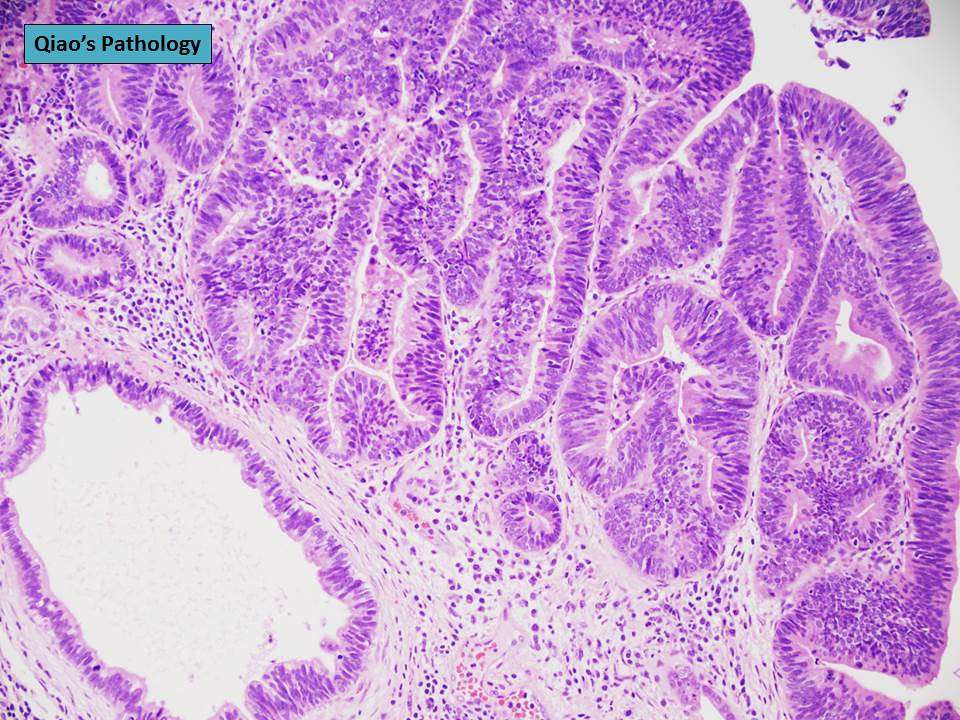
There have been new developments in the diagnosis of CIS that parallel the molecular understanding of the disease. Bladder cancer has been traditionally diagnosed with WL cystoscopy. A recent study by Nkwam et al. evaluated the cancer detection rate of WL flexible and rigid cystoscopy in patients with a previous diagnosis of NMIBC . They found a 23.5% cancer detection rate in intermediate and high risk NMIBC when performing biopsies of isolated red patches seen on WL cystoscopy.
Huang et al. published a systematic review and meta-analysis of 9 articles including 402 patients regarding optical coherence tomography in bladder cancer . This technology works as an optical biopsy ultrasound is used to provide cross-sectional images at a magnification of 10m, which is similar to histopathology slides. The authors report that this technology has a 96% sensitivity and 82% specificity for the diagnosis of early stage bladder cancer, including CIS, when compared to histopathology as the gold standard. These technologies are still in development and are not currently used in clinical practice for the diagnosis of bladder cancer.
Read Also: Diet After Bladder Cancer Surgery
Bcg Relapse And Salvage Regimens
Guideline Statement 22
22. In an intermediate- or high-risk patient with persistent or recurrent disease or positive cytology following intravesical therapy, a clinician should consider performing prostatic urethral biopsy and an upper tract evaluation prior to administration of additional intravesical therapy.
Discussion
Urothelial carcinoma, particularly CIS, is considered a field-change disease with the entire urothelium at risk in affected individuals. Clinicians should remain aware of sites outside the bladder as potential sources for metachronous tumors. While the initial diagnostic evaluation includes radiographic/endoscopic visualization of the entire urinary tract, the extra-vesical urothelium remains at long-term risk for subsequent tumor development. Moreover, these sites may harbor disease and contribute to cancer recurrence within the bladder.
Of note, the Panel recognizes that evaluation of the upper urinary tract and urethra may be withheld in select patients who have received a single induction course of intravesical BCG and subsequently have persistent evidence of disease and are to undergo a second course of BCG.
Guideline Statement 23
23. In an intermediate- or high-risk patient with persistent or recurrent Ta or CIS disease after a single course of induction intravesical BCG, a clinician should offer a second course of BCG.
Discussion
Guideline Statement 24
Discussion
Guideline Statement 25
Discussion
Guideline Statement 26
Risk Adjusted Surveillance And Follow
Guideline Statement 32
32. After completion of the initial evaluation and treatment of a patient with NMIBC, a clinician should perform the first surveillance cystoscopy within three to four months.
Discussion
The natural history of NMIBC is often characterized by recurrence, even for solitary, small, low-grade papillary tumors. At the time of first evaluation and treatment, none of the existent risk stratification tools or urinary biomarkers is sufficiently sensitive and specific to predict which patient will have an early tumor recurrence. Therefore, the only reliable way to know in a particular patient whether they are at risk for early recurrence is by cystoscopic visualization of the urothelium at a relatively early interval after the first treatment/resection. In addition, visualization at a relatively early interval allows the treating urologist to verify that the initial resection was complete. The Panel, therefore, felt that the first repeat cystoscopic evaluation should occur three to four months after the initial treatment and evaluation, regardless of the patient’s overall risk.
Guideline Statement 33
33. For a low-risk patient whose first surveillance cystoscopy is negative for tumor, a clinician should perform subsequent surveillance cystoscopy six to nine months later, and then annually thereafter surveillance after five years in the absence of recurrence should be based on shared-decision making between the patient and clinician.
Discussion
Discussion
Read Also: Unable To Empty Bladder Female
Prognosis And Survival For Bladder Cancer
If you have bladder cancer, you may have questions about your prognosis. A prognosis is the doctors best estimate of how cancer will affect someone and how it will respond to treatment. Prognosis and survival depend on many factors. Only a doctor familiar with your medical history, the type and stage and other features of the cancer, the treatments chosen and the response to treatment can put all of this information together with survival statistics to arrive at a prognosis.
A prognostic factor is an aspect of the cancer or a characteristic of the person that the doctor will consider when making a prognosis. A predictive factor influences how a cancer will respond to a certain treatment. Prognostic and predictive factors are often discussed together. They both play a part in deciding on a treatment plan and a prognosis.
The following are prognostic and predictive factors for bladder cancer.
Whos At Risk For Bladder Cancer
There are 70,000 new cases of bladder cancer each year in the United States. The male-to-female incidence ratio is about 3 to 1. Your chances of developing bladder cancer increase with age.
The most common risk factor is smoking, which accounts for at least half of all new cases. Other risk factors include:
- abuse of phenacetin, an analgesic
- long-term use of cyclophosphamide , a chemotherapy drug and immune suppressant
- chronic irritation due to a parasitic disease called schistosomiasis
- chronic irritation from long-term catheterization
- exposure to certain industrial chemicals used in the dye, rubber, electric, cable, paint, and textile industries
Read Also: How Do They Diagnose Bladder Cancer
What To Do Before And After Treatment
Talk with your doctors about whether you need to do anything to prepare for treatment and help your recovery. Some things they may suggest are to:
- Stop smoking if you smoke, aim to quit before starting treatment. If you keep smoking, you may not respond as well to treatment and you may have more treatment-related side effects. Continuing to smoke also increases your risk of cancer returning.
- Begin or continue an exercise program exercise will help build up your strength for treatment and recovery. It can also help you deal with side effects of treatment.
- Improve diet aim to eat a balanced diet with a variety of fruit, vegetables, wholegrains and protein. Eating well can improve your strength and you may respond better to treatment.
- See a physiotherapist they can teach you exercises to strengthen your pelvic floor muscles, which help control how your bladder and bowel work. These exercises are useful if you have a neobladder, a partial cystectomy, or radiation therapy.
What Are The Stages Of Bladder Cancer
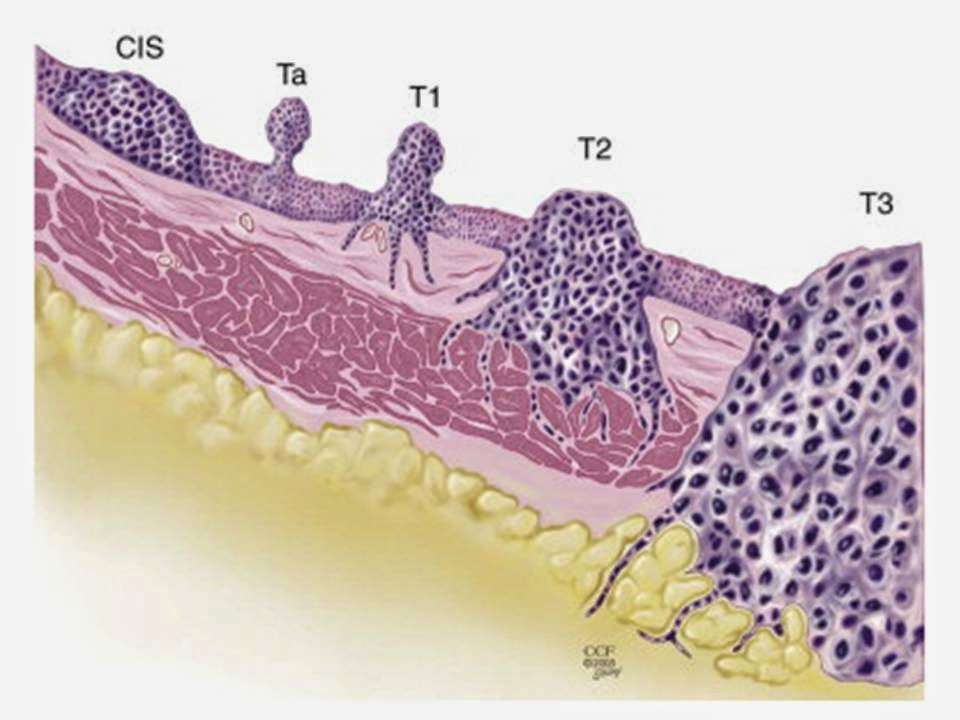
Bladder cancer can be either early stage or invasive .
The stages range from TA to IV . In the earliest stages , the cancer is confined to the lining of the bladder or in the connective tissue just below the lining, but has not invaded into the main muscle wall of the bladder.
Stages II to IV denote invasive cancer:
- In Stage II, cancer has spread to the muscle wall of the bladder.
- In Stage III, the cancer has spread to the fatty tissue outside the bladder muscle.
- In Stage IV, the cancer has metastasized from the bladder to the lymph nodes or to other organs or bones.
A more sophisticated and preferred staging system is known as TNM, which stands for tumor, node involvement and metastases. In this system:
- Invasive bladder tumors can range from T2 all the way to T4 .
- Lymph node involvement ranges from N0 to N3 .
- M0 means that there is no metastasis outside of the pelvis. M1 means that it has metastasized outside of the pelvis.
Don’t Miss: What Is The Best Medicine For Bladder Control