Posttreatment Of Recurrent Or Persistent Disease
Treatment of Patients With Positive Cystoscopy
Patients under observation after initial TURBT who show a documented recurrence using positive cystoscopy should undergo another TURBT and then adjuvant intravesical therapy or cystectomy based on the stage and grade of the recurrent lesion. Patients should be followed up as indicated based on the risk of their disease .
Recurrence After Intravesical Treatment
After the initial intravesical treatment and 12-week evaluation, patients with persistent cTa, cT1, or Tis disease tumors can be given a second induction course of induction therapy . No more than 2 consecutive induction courses should be given. If a second course is given, TURBT is performed to determine the presence of residual disease at the second 12-week follow-up. If no residual disease is found, maintenance BCG is recommended for patients who received prior BCG.
Treatment of Patients With Positive Cytology
In patients without a documented recurrence but with positive cytology and negative cystoscopy and imaging, selected mapping biopsies, including TUR of the prostate, are indicated. In addition, the upper tract must be evaluated and ureteroscopy may be considered for detecting tumors of the upper tract. If available, enhanced cystoscopy should be considered .
Treatment Of Ct1 Tumors
Based on the histologic differentiation, most cT1 lesions are high grade and considered to be potentially dangerous, with a higher risk for recurrence and progression. These tumors may occur as solitary lesions or as multifocal tumors with or without an associated Tis component.
These tumors are treated with a complete endoscopic resection, and repeat TURBT is strongly advised.83 This is supported by a trial that prospectively randomized 142 patients with pT1 tumors to a second TURBT within 2 to 6 weeks of the initial TURBT or no repeat TURBT.84 All patients received adjuvant intravesical therapy. Although OS was similar, the 3-year recurrence-free survival was significantly higher in the repeat TURBT arm versus the control arm , especially among patients with high-grade tumors.
If residual cT1 disease is found at repeat TURBT, treatment should consist of BCG or cystectomy. Within T1 disease, a particularly high-risk stratum can be identified: multifocal lesions, tumors associated with CIS or lymphovascular invasion, variant histology , or lesions that recur after BCG treatment. Some data suggest that early cystectomy may be preferred in these patients because of the high risk for progression to a more advanced stage.85,86
Keeping Personal Health Records
You and your doctor should work together to develop a personalized follow-up care plan. Be sure to discuss any concerns you have about your future physical or emotional health. ASCO offers forms to help keep track of the cancer treatment you received and develop a survivorship care plan when treatment is completed.
This is also a good time to talk with your doctor about who will lead your follow-up care. Some survivors continue to see their oncologist or urologist, while others transition back to the care of their primary care doctor or another health care professional. This decision depends on several factors, including the type and stage of bladder cancer, side effects, health insurance rules, and your personal preferences, expectations, and beliefs.
If a doctor who was not directly involved in your cancer care will lead your follow-up care, be sure to share your cancer treatment summary and survivorship care plan forms with them and with all future health care providers. Details about your cancer treatment and communication preferences are very valuable to the health care professionals who will care for you throughout your lifetime.
The next section in this guide is Survivorship. It describes how to cope with challenges in everyday life after a cancer diagnosis. Use the menu to choose a different section to read in this guide.
Read Also: Foods To Strengthen Bladder Muscles
Chemotherapy For Metastatic Disease
The specific chemotherapy regimen recommended partially depends on the presence or absence of medical comorbidities, such as cardiac disease and renal dysfunction, along with the risk classification of the patient based on disease extent. In general, long-term survival with combination chemotherapy alone has been reported only in good-risk patients, defined as those with good performance status, no visceral or bone disease, and normal alkaline phosphatase or lactic dehydrogenase levels. Poor-risk patients, defined as those with poor performance status or visceral disease, have consistently shown very poor tolerance to multiagent combination programs and few complete remissions, which are prerequisites for cure.
Although current data are insufficient to recommend the previously noted alternative regimens as routine first-line options, noncisplatin-containing regimens may be considered in patients who cannot tolerate cisplatin because of renal impairment or other comorbidities . Additionally, 2 checkpoint inhibitors, atezolizumab and pembrolizumab, have been FDA approved for use as a first-line therapy in certain patients. Consideration of checkpoint inhibitors must be integrated into the therapeutic planning for all patients with locally advanced and metastatic disease . The panel recommends enrollment in clinical trials of potentially less toxic therapies.
Treating Stage I Bladder Cancer
Stage I bladder cancers have grown into the connective tissue layer of the bladder wall , but have not reached the muscle layer.
Transurethral resection with fulguration is usually the first treatment for these cancers. But it’s done to help determine the extent of the cancer rather than to try to cure it. If no other treatment is given, many people will later get a new bladder cancer, which often will be more advanced. This is more likely to happen if the first cancer is high-grade .
Even if the cancer is found to be low grade , a second TURBT is often recommended several weeks later. If the doctor then feels that all of the cancer has been removed, intravesical BCG or intravesical chemo is usually given. If all of the cancer wasn’t removed, options are intravesical BCG or cystectomy .
If the cancer is high grade, if many tumors are present, or if the tumor is very large when it’s first found, radical cystectomy may be recommended.
For people who arent healthy enough for a cystectomy, radiation therapy might be an option, but the chances for cure are not as good.
Recommended Reading: Can Chewing Tobacco Cause Bladder Cancer
Can I Lower My Risk Of The Bladder Cancer Progressing Or Coming Back
If you have bladder cancer, you probably want to know if there are things you can do that might lower your risk of the cancer growing or coming back, such as exercising, eating a certain type of diet, or taking nutritional supplements.
While there are some things you can do that might be helpful, more research is needed to know for sure.
Radiotherapy With A Radiosensitiser
Radiotherapy is given by a machine that beams the radiation at the bladder . Sessions are usually given on a daily basis for 5 days a week over the course of 4 to 7 weeks. Each session lasts for about 10 to 15 minutes.
A medicine called a radiosensitiser should also be given alongside radiotherapy for muscle-invasive bladder cancer. This medicine affects the cells of a tumour, to enhance the effect of radiotherapy. It has a much smaller effect on normal tissue.
As well as destroying cancerous cells, radiotherapy can also damage healthy cells, which means it can cause a number of side effects. These include:
- diarrhoea
- tightening of the vagina , which can make having sex painful
- erectile dysfunction
- tiredness
- difficulty passing urine
Most of these side effects should pass a few weeks after your treatment finishes, although there’s a small chance they’ll be permanent.
Having radiotherapy directed at your pelvis usually means you’ll be infertile .
After having radiotherapy for bladder cancer, you should be offered follow-up appointments every 3 months for the first 2 years, then every 6 months for the next 2 years, and every year after that. At these appointments, your bladder will be checked using a cystoscopy.
You may also be offered CT scans of your chest, abdomen and pelvis after 6 months, 1 year and 2 years. A CT scan of your urinary tract may be offered every year for 5 years.
Don’t Miss: Why Does My Bladder Feel Irritated
Palliative Or Supportive Care
If your cancer is at an advanced stage and can’t be cured, your medical team should discuss how the cancer will progress and which treatments are available to ease the symptoms.
You can be referred to a palliative care team, who can provide support and practical help, including pain relief.
Page last reviewed: 01 July 2021 Next review due: 01 July 2024
Cellular Classification Of Bladder Cancer
More than 90% of bladder cancers are transitional cell carcinomas derived from the uroepithelium. About 2% to 7% are squamous cell carcinomas, and 2% are adenocarcinomas. Adenocarcinomas may be of urachal origin or nonurachal origin the latter type is generally thought to arise from metaplasia of chronically irritated transitional epithelium. Small cell carcinomas also may develop in the bladder. Sarcomas of the bladder are very rare.
Pathologic grade of transitional cell carcinomas, which is based on cellular atypia, nuclear abnormalities, and the number of mitotic figures, is of great prognostic importance.
References
Read Also: How To Relax The Bladder Naturally
Metastasectomy For Oligometastatic Disease
Highly select patients with oligometastatic disease who are without evidence of rapid progression may benefit from metastasectomy after response to systemic therapy. While there are limited prospective data supporting the role of metastasectomy for treatment of urothelial bladder cancer, several retrospective studies have demonstrated that metastasectomy can be a valid treatment option for certain patients with metastatic bladder cancer, particularly those with favorable response to systemic therapy, solitary metastatic lesions, and lung or lymph node sites of disease.
A phase II trial of 11 patients with bladder primary urothelial carcinoma metastatic to the retroperitoneal lymph nodes who underwent complete bilateral retroperitoneal lymph node dissection reported 4-year DSS and RFS rates of 36% and 27%. Patients with viable tumor in no more than 2 lymph nodes and/or excellent response to presurgical systemic chemotherapy showed the best survival rates, indicating that a low burden of disease or good response to presurgical chemotherapy may be important in achieving benefit from metastastectomy.93 Another phase II trial of 70 patients who underwent complete surgical resection of bladder cancer metastases investigated survival, performance status, and quality of life after surgery. This study reported no survival advantage from surgery, although the quality of life and performance status were improved for symptomatic patients.94
Enhanced Cystoscopy And Imaging For Follow
As mentioned above, white light cystoscopy has limitations with sensitivity for papillary tumors of 7080%, which is lower in case of CIS . These numbers are in trials, and for the studies performed with blue light in the setting of a transurethral resection, so in the operating room. Can we also use these techniques to improve our performance during outpatient follow-up, which usually is done with flexible instruments.
NBI is easy to perform in an outpatient setting, since it does not require additional preparation and the specific equipment can be used both in the clinical as well as in the outpatient setting. The real advantage of NBI, however, remains to be proven, since published data are limited and not in agreement. Mukherjee et al. showed in a randomized controlled trial NBI to be better in tumor detection and resection as compared to white light , whereas an earlier and larger study did not show a difference in recurrence rate after 1 year of follow-up .
The consequence of better tools in follow-up, in this case better cystoscopy, has been shown to result in more confidence and less anxiety among patients and urologists, resulting in longer intervals between cystoscopies . Another way to improve the sensitivity of cystoscopy might be the use of artificial intelligence , which was shown to improve both sensitivity and specificity resulting in a better bladder cancer detection and resection .
Also Check: Where Does Bladder Cancer Usually Spread To
Organizations And Recommendation Approaches
Guidelines for the diagnosis and management of bladder cancer have been issued by the following organizations:
- American Urological Association/Society of Urological Oncology
- European Association of Urology
- European Society for Medical Oncology
- National Comprehensive Cancer Network
Each organization uses a different methodology to determine levels of evidence and grades for recommendations, as follows:
Treatment Of Stage Iv Bladder Cancer
In This Section
Chemotherapy alone or as an adjunct to local treatment
Cisplatin-based combination chemotherapy regimens are the standard of care for first-line therapy for stage IV bladder cancer in patients who can tolerate it. The only chemotherapy regimens that have been shown to result in longer survival in randomized controlled trials are MVAC, dose-dense MVAC, and CMV. GC was compared with MVAC in a randomized controlled trial and neither regimen was associated with a statistically significant difference in response rate or survival. The two regimens are generally considered equivalent, but they have never been compared in a noninferiority trial. Of note, patients with good performance status and lymph node-only disease have a low but significant rate of achieving a durable complete remission with MVAC or GC. In the large, randomized, controlled trial comparing MVAC with GC, for example, 5-year OS in patients with lymph node-only disease was 20.9%. Dose-dense MVAC and standard-dose MVAC were compared in a randomized controlled trial, and dose-dense MVAC was associated with longer survival.
Ongoing studies are evaluating new chemotherapy combinations.
Evidence :
Immunotherapy
Pembrolizumab
Evidence :
Evidence :
Don’t Miss: Can Acupuncture Help With Bladder Problems
Clinical Presentation And Workup
The most common presenting symptom in patients with bladder cancer is microscopic or gross hematuria, although urinary frequency due to irritation or a reduced bladder capacity can also develop. Less commonly, the presenting symptom is a urinary tract infection. Upper tract obstruction or pain may occur in patients with a more advanced lesion. Patients presenting with these symptoms should be evaluated with office cystoscopy to determine if a lesion is present. If one is documented, the patient should be scheduled for a transurethral resection of the bladder tumor to confirm the diagnosis and determine the extent of disease within the bladder. Urine cytology may also be obtained around the time of cystoscopy. Being that smoking is a major risk factor for bladder cancer,8 screening for smoking and initiation of treatment for smoking cessation, if appropriate, is recommended during the initial evaluation .
Although selected mapping biopsies may be indicated in specific situations for lesions that are solid or if Tis or high-grade disease is suspected , random biopsies rarely yield positive results, especially for low-risk tumors.12 Therefore, mapping biopsies of normal-appearing urothelium are not necessary for most patients.
Positive urinary cytology may indicate urothelial tumor anywhere in the urinary tract. In the presence of a positive cytology and a normal cystoscopy, the upper tracts and the prostate in men must be evaluated and ureteroscopy may be considered.
Tumor Recurrence And Worsening Progression Rate In Entire Patient Population
The mean age of the patients was 62.9 years and the median follow-up interval was 101.5 months . Solitary/multiple tumors were seen in 114/76 patients, respectively. Tumor recurrence occurred in 82 patients . Most patients who had tumor recurrence could be diagnosed by the routine follow-up cystoscopic examination except for 3 patients who were detected due to gross hematuria. When we divided the patients into two groups, those with or without tumor recurrence, there were no significant differences in age, gender, IVI or smoking status between the two groups . The recurrence rate in multiple tumors was significantly higher than that in solitary tumors . Univariate and multivariate analyses demonstrated that multiple tumor and absence of IVI were significant risk factors for tumor recurrence . Kaplan-Meier curves demonstrated that the 5-year recurrence free survival rate for solitary tumors was significantly higher than that for multiple tumors , and also higher for patients receiving intravesical instillation .
Table 1 Clinical characteristics of all 190 patientsFigure 2
Also Check: How To Remove Bladder Cancer
Contact The Guideline Resource Unit
The role of the Guideline Resource Unit is to support the PTTs in activities related to clinical practice guideline development and implementation. Through review, selection, synthesis, evaluation, interpretation, and reporting of evidence, GURU facilitates communication and collaboration among PTT members. If you have any questions or concerns about these guidelines, please contact .
Treatment Of Stage 0 Bladder Cancer
In This Section
Transurethral resection with fulguration followed by an immediate postoperative instillation of intravesical chemotherapy
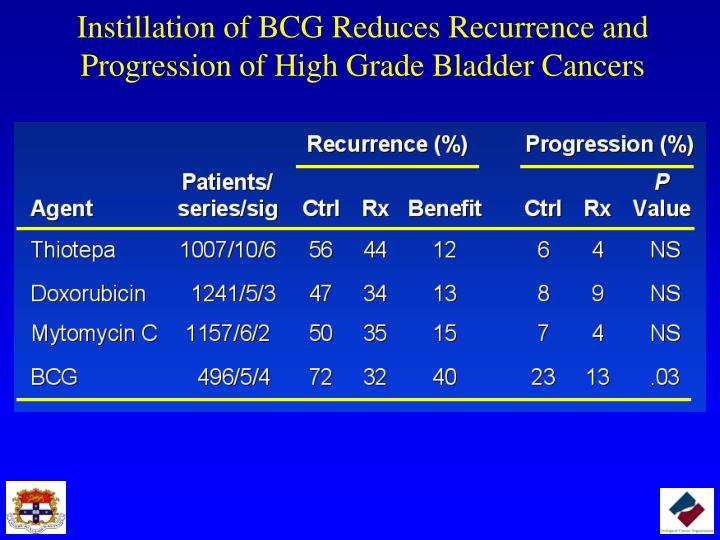
TUR and fulguration are the most common and conservative forms of management. Careful surveillance of subsequent bladdertumor progression is important. Because most bladder cancers recur after TUR, one immediate intravesical instillation of chemotherapy after TUR is often administered. Numerous randomized controlled trials have evaluated this practice, and a meta-analysis of seven trials reported that a single intravesical treatment with chemotherapy reduced the odds of recurrence by 39% . However, although a single instillation of chemotherapy lowers the relapse rate in patients with multiple tumors, the majority still relapse. Such treatment is thus not sufficient by itself for these patients.
One retrospective series addressed the valueof performing a second TUR within 2 to 6 weeks of the first TUR. A second TUR performed on 38 patients with Tis or Tadisease revealed that nine patients had lamina propria invasion and threepatients had muscle invasion .
Such information may change thedefinitive management options in these individuals. Patients with extensive multifocal recurrent disease and/or other unfavorable prognostic features require moreaggressive forms of treatment.
Evidence :
Evidence :
Intravesical chemotherapy
Segmental cystectomy
Read Also: Foods To Prevent Bladder Cancer Recurrence