Box : Prognostic Factors For Recurrence
-
Number of tumours more tumours mean more frequent recurrences.
-
Previous recurrence rate* or a recurrence at three months.
-
Size of the tumour those > 3 cm carry a worse prognosis.
-
Grade of anaplasia.
-
Presence of CIS.
*The recurrence rate being the number of positive cystoscopies per year over the number of cystoscopies performed per year.
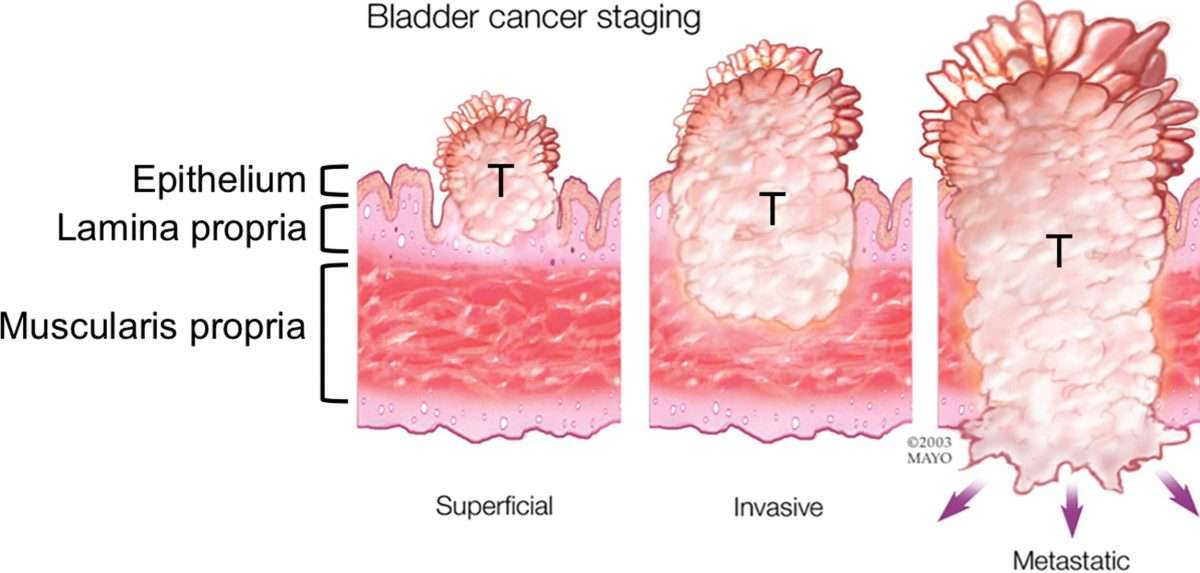
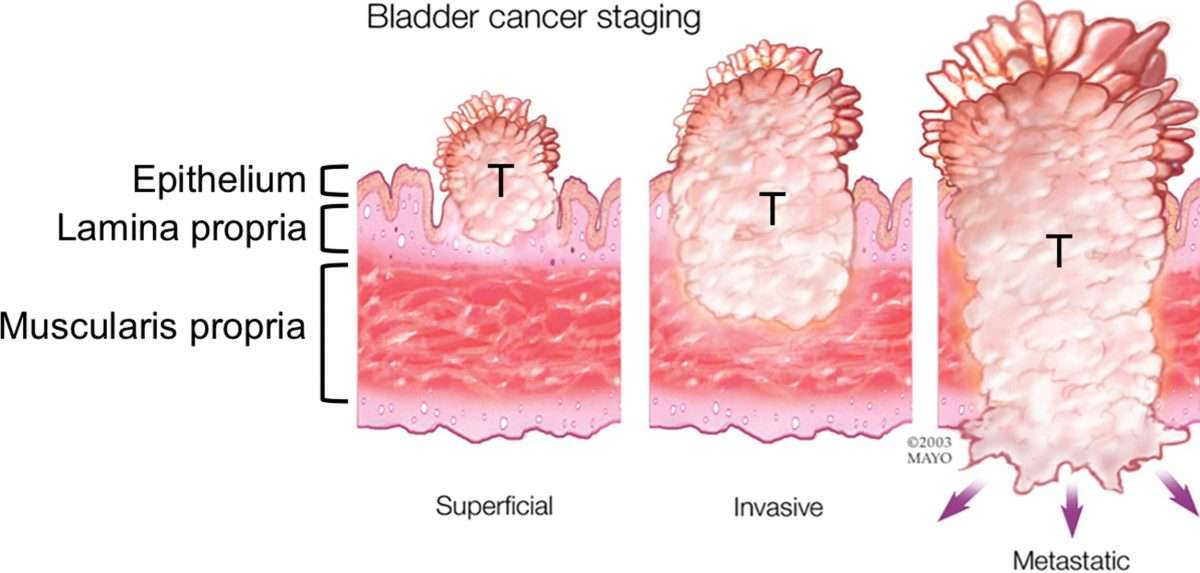
For progression, tumour grade is the most important factor. It is also known that T1 tumours have a worse prognosis than Ta tumours. Using these factors patients with superficial bladder cancer can be divided into three groups: the lowest risk group with a single less than 3 cm Ta G1 tumour, and a recurrence rate of less than one tumour per year a high risk tumour of T1 G3, multifocal, large, highly recurrent, and CIS and other tumours of intermediate risk. Recent studies further confirm these criteria.
How Is Bcg Given
The combination of BCG and TURBT is the most effective treatment for high-risk non-muscle-invasive bladder cancer. BCG is given once a week for six weeks, starting 24 weeks after TURBT surgery. It is put directly into the bladder through a catheter. You may be asked to change position every 15 minutes so the vaccine washes over the entire bladder. This is usually done as a day procedure in hospital, and each treatment session takes up to two hours.
Your treatment team will tell you what safety measures to follow after you go home. This is because BCG is a vaccine that contains live bacteria, which can harm healthy people.
Let your doctor know of any other medicines or complementary therapies you are using, as they may interfere with how well the bladder cancer responds to BCG. For example, the drug warfarin is known to interact with BCG.
How To Take Bacillus Calmette
BCG is given directly into the bladder through a catheter. The medicine is left in the bladder for 1-2 hours. The dosage and schedule is determined by your healthcare provider. It is not uncommon to have urinary frequency or painful urination for 48 hours after treatment. If this continues after 48 hours, call your doctor or nurse.
How the Intravesicular Treatment is Given
- You should limit your fluid intake starting the night prior to the procedure and have no fluids for 4 hours before. This is so you will be able to hold your urine in during the procedure for the full treatment time. In addition, the area receives more concentrated doses of the medicine with less urine output during the procedure.
- If you take a diuretic , you will be told to not take this for at least 4 hours before the procedure.
- A urinary catheter is inserted into the bladder and any urine is drained.
- The BCG is given through the catheter, into the bladder. The catheter may be removed or clamped and remain in place based on your providers recommendation.
- You will need to hold the BCG in your bladder for 1-2 hours. You may need to change positions every 15 minutes to be sure the medicine reaches all areas of the bladder. Do this by rolling on your side, back, other side, and stomach.
Precautions After Treatment
Don’t Miss: What Causes Constant Bladder Infections
What Happens During Treatment
A urinary catheter is inserted through your urethra and into your bladder. Then the BCG solution is injected into the catheter. The catheter is clamped off so the solution stays in your bladder. Some doctors may remove the catheter at this time.
You have to hold the medicine in your bladder. Youll be instructed to lie on your back and to roll from side to side to make sure the solution reaches your entire bladder.
After about two hours, the catheter is unclamped so the fluid can be drained. If the catheter was already removed, youll be asked to empty your bladder at this time.
How Bcg Treatment Is Performed
BCG treatment is administered in a liquid form using a catheter inserted into the urethra so the BCG enters directly into the bladder.
Once the BCG has reached the bladder, the patient needs to avoid going to the bathroom for at least two hours in order for the BCG to have time to reach the cancer in the bladders lining.
You May Like: What Causes Loss Of Bladder And Bowel Control
After Your Bcg Treatment
If thecatheter was left in the bladder during your treatment, the BCG will be drainedback into a bag before the catheter is removed.
If you wouldlike something to drink you can now do so.
Sex – youshould abstain from intercourse/oral sex for 2-3 days after each treatment. Theuse of condoms thereafter is advised and should continue to be used for severalweeks after your treatment has been completed.
Pregnancy -the effects on pregnancy are unknown. If you are planning to have children youshould discuss this with your doctor as female patients of child bearing ageare advised to use birth control during treatments and to wait at least 2 yearsbefore conceiving, longer if on maintenance treatment.
Breastfeeding is not advised when having BCG treatment
Definition Of Bcg Failure In Non
ABSTRACT
Bladder cancer is the fifth most commonly diagnosed cancer in the nation. Radical cystectomy is the most effective treatment for locally advanced bladder cancer and is a formidable operation. The perioperative mortality in high-volume centers ranges from 0.7 to 5.6%. Thus, when faced with this diagnosis, there is a desire to pursue a bladder-preserving strategy and avoid RC. One treatment for HG Ta/T1, and carcinoma in situ is intravesical bacillus Calmette-Guérin therapy. Many studies have confirmed its value in reducing tumor recurrence following transurethral resection of bladder tumors . After reviewing the various guidelines, we summarize our recommendations for defining BCG failure.
Mohamed H Kamel, Sarabeth L Bailey, John T Moore, Samy M Heshmat, Nabil K Bissada
Department of Urology, University of Arkansas for Medical Sciences, Little Rock, Arkansas
Submitted: September 9, 2011 – Accepted for Publication: November 9, 2011
KEYWORDS: Bladder Cancer BCG Guidelines
CORRESPONDENCE: Mohamed H Kamel, MD, Assistant Professor, Urologic Oncologist, University of Arkansas for Medical Sciences, 4301 West Markham, Little Rock, Arkansas, 72205 .
INTRODUCTION
Bladder cancer is the fifth most commonly diagnosed cancer in the nation. It is estimated that 70 980 men and women will be diagnosed with BC, and 14 330 patients will die of this disease in the United States in 2009. As of January 1, 2004, approximately 51 1790 individuals in the US have bladder cancer .
You May Like: Signs Of Bladder Cancer In Male
Treatment Of Bladder Cancer By Stage
Most of the time, treatment of bladder cancer is based on the tumors clinical stage when its first diagnosed. This includes how deep its thought to have grown into the bladder wall and whether it has spread beyond the bladder. Other factors, such as the size of the tumor, how fast the cancer cells are growing , and a persons overall health and preferences, also affect treatment options.
Dont Miss: Radiotherapy Success Rate For Bladder Cancer
When Do Doctors Use Bcg
Doctors most commonly use BCG to treat superficial bladder cancer. The vaccine stimulates the immune system to attack cancer cells in the bladder. It can be used with intravesical chemotherapy for advanced stages of bladder cancer.
It is not recommended for those who have weakened immune systems. While BCG treatment for bladder cancer can be effective, it is not a cure. It can help prevent cancer from recurring.
Don’t Miss: How To Get A Stronger Bladder
Sexuality And Feeling Good About Your Body
Bladder cancer treatment can often affect your sex life. Learning to be comfortable with your body during and after bladder cancer treatment is a personal journey, one that’s different for everyone. Information and support can help you cope with these changes over time. Learn more in Fertility and Sexual Side Effects in People with Cancer.
Treatment Of Cis Or Residual Papillary Tumours
Treatment of CIS
BCG is first line treatment for CIS. It has been shown by Akaza et al in 1995 that with BCG 84.4% of his 32 cases with CIS showed a complete response. These results were better than the previously reported figures by Harland et al, which revealed a complete response in only 53% of their 53 patients. Although it should be noted that the Harland group used a lower dose of BCG.
Merz et al, in 1995 looked at 115 patients with CIS, 25 of these had primary CIS and 90 had secondary CIS . They found that 88% of those with primary CIS had responded completely, with negative cytology and cystoscopic findings . Of those with secondary CIS, 78% had a complete response after treatment with BCG . These results are summarised in table 1.
Summary of results for CIS and papillary tumours treated with BCG
Treatment of papillary tumours
As an indication for BCG treatment, this is less common and is usually utilised when endoscopic control is not possible, either because the sheer volume of bladder tumour makes complete resection difficult or because the patient is not medically fit for an operative procedure. Akaza et al used BCG as a primary treatment for 125 cases of Ta or T1 tumours, and they were able to achieve a 66.4% complete response. A partial response was achieved in a further 20.8% of their patients.
Read Also: Bladder Infection Or Kidney Infection
What Are The Side Effects
Some patients have difficulty completing long-term BCG therapy because of irritation in the bladder.2 To help with this irritation, the treatment frequency may be adjusted to give you a longer break between treatments. You may not notice any reaction after the first few BCG treatments. After the third treatment, patients usually start to experience bladder irritation pain or burning during urination, joint pain, fatigue, and flu-like symptoms that can last a few days. Most symptoms and side effects can be treated with over-the-counter pain medicines.
While BCG is a fairly common treatment for bladder cancer, every person has different experiences. Itâs important to talk to your doctor about any questions or concerns you may have at any point during your treatment. Being mentally prepared for what to expect can help to reduce stress or uncertainty about treatment or help you think of additional questions for your healthcare team.
Association Between Antibiotic Treatment And The Efficacy Of Intravesical Bcg Therapy In Patients With High
- 1Department of Urology, Center for Urologic Cancer, National Cancer Center, Goyang, South Korea
- 2Department of Urology, Hallym University Kangnam Sacred Heart Hospital, Hallym University College of Medicine, Seoul, South Korea
- 3Biometrics Research Branch, Research Institute, National Cancer Center, Goyang, South Korea
- 4Division of Tumor Immunology, Research Institute, National Cancer Center, Goyang, South Korea
- 5Department of Pathology, National Cancer Center, Goyang, South Korea
Objective: To investigate the association between antibiotic therapy and the efficacy of intravesical BCG therapy in patients with high-risk non-muscle invasive bladder cancer .
Methods: This study involved the retrospective review of medical records of patients who underwent transurethral resection of bladder tumors for high-risk NMIBC followed by intravesical BCG therapy between 2008 and 2017. Patients were categorized as none, short- , and long-course use based on the duration of antibiotic treatment concurrent with or initiated 30 days before BCG therapy. Oncologic outcomes, including recurrence-free survival and progression-free survival, were analyzed.
Long-course antibiotic treatment concurrently with or prior to intravesical BCG adversely influenced disease recurrence and progression outcomes in patients with high-risk NMIBC. Careful use of antibiotics may be required to enhance the efficacy of intravesical BCG therapy. Further mechanistic and prospective studies are warranted.
Don’t Miss: Is Urothelial Cancer The Same As Bladder Cancer
Surgery After Bcg Failure
The EAU guidelines recommend cystectomy as the treatment of choice for CIS failing adequate BCG and as an option in other high-risk tumours.3 Similarly, the Canadian guidelines state that in patients with high-risk NMIBC with BCG failure, the option of radical cystectomy should be recommended and discussed with the patient .22 The guidelines also suggest that immediate cystectomy may be initially offered to patients with T1G3/T1HG and to patients with high-grade tumours with concomitant CIS or multiple recurrent high-grade tumours . The advantage of cystectomy in superficial tumours that failed BCG treatment is obvious. Tumour-specific survival is between 80% and 90% at 5 years, and thereby approaches the 5-year tumour-specific survival of patients with superficial bladder cancer.11
However, cystectomy for high-risk superficial disease is not only an invasive procedure linked to significant morbidity, but also has a number of other problems associated with it. When patients with NMIBC have a recurrence with invasive disease, a window of opportunity may be overlooked. For instance, in 62 patients with a high-grade recurrence and treated with cystectomy who had failed adequate BCG treatment, the 5-year disease-specific survival rate of progressive patients was only 38%, significantly lower than in those patients without invasive tumour. The authors identified the presence of a tumour in the prostatic urethra before cystectomy as a factor associated with shorter survival.48
Who Can Have This Treatment
BCG is appropriate for noninvasive and minimally invasive bladder cancers. It usually follows a procedure called transurethral resection of bladder tumor . Its intended to help prevent recurrence.
This treatment only affects cells inside the bladder. Its not useful for later stage bladder cancer that has spread into or beyond the bladder lining, or to other tissues and organs.
Also Check: Bladder Infection And Lower Back Pain
Keeping Personal Health Records
You and your doctor should work together to develop a personalized follow-up care plan. Be sure to discuss any concerns you have about your future physical or emotional health. ASCO offers forms to help keep track of the cancer treatment you received and develop a survivorship care plan when treatment is completed.
This is also a good time to talk with your doctor about who will lead your follow-up care. Some survivors continue to see their oncologist or urologist, while others transition back to the care of their family/primary care doctor or another health care professional. This decision depends on several factors, including the type and stage of bladder cancer, side effects, health insurance rules, and your personal preferences, expectations, and beliefs.
If a doctor who was not directly involved in your cancer care will lead your follow-up care, be sure to share your cancer treatment summary and survivorship care plan forms with them and with all future health care providers. Details about your cancer treatment and communication preferences are very valuable to the health care professionals who will care for you throughout your lifetime.
The next section in this guide is Survivorship. It describes how to cope with challenges in everyday life after a cancer diagnosis. Use the menu to choose a different section to read in this guide.
Read Also: Do You Bleed With A Bladder Infection
Is Using Less Bcg Okay
Researchers are investigating another potential solution to the BCG shortage: using a lower dose of BCG per treatment. Several studies have suggested that using a lower dose may be a suitable option, including a study published last year showing that, in people with high-risk NMIBC, using one-third of the standard dose of BCG didnt appear to be any less effective than the standard full dose.
The study had a large population of people with high-risk tumors that are often resistant to BCG and they are still getting very good numbers, he said.
Nevertheless, evaluating how the combination performs in people from different racial and ethnic backgrounds will be important.
Weve seen time and again that something can perform well in , but once it gets to the community, we can see differing results, Dr. Gurram said.
The need to travel to the hospital monthly to get the maintenance treatment is a challenge of this particular regimen, Dr. Packiam noted. Thats particularly true in rural areas and for people without easy access to transportation.
It does produce some logistical burdens for patients, he said.
Along those lines, Dr. Meeks and his colleagues wondered about the extent to which maintenance therapy is even needed. As with BCG treatment, over time, many patients stop taking it. So it will be important to determine if 6, 12 or 24 months of is necessary, they wrote.
But, honestly, revisiting old chemotherapies that give promising results is great to see.
Recommended Reading: How To Strengthen Bladder Wall
Radiotherapy With A Radiosensitiser
Radiotherapy is given by a machine that beams the radiation at the bladder . Sessions are usually given on a daily basis for 5 days a week over the course of 4 to 7 weeks. Each session lasts for about 10 to 15 minutes.
A medicine called a radiosensitiser should also be given alongside radiotherapy for muscle-invasive bladder cancer. This medicine affects the cells of a tumour, to enhance the effect of radiotherapy. It has a much smaller effect on normal tissue.
As well as destroying cancerous cells, radiotherapy can also damage healthy cells, which means it can cause a number of side effects. These include:
- difficulty passing urine
Most of these side effects should pass a few weeks after your treatment finishes, although theres a small chance theyll be permanent.
Having radiotherapy directed at your pelvis usually means youll be infertile .
After having radiotherapy for bladder cancer, you should be offered follow-up appointments every 3 months for the first 2 years, then every 6 months for the next 2 years, and every year after that. At these appointments, your bladder will be checked using a cystoscopy.
You may also be offered CT scans of your chest, abdomen and pelvis after 6 months, 1 year and 2 years. A CT scan of your urinary tract may be offered every year for 5 years.