Medications For Overactive Bladder
Medications for overactive bladder target muscles that control bladder function. These drugs can be used alone or in combination, and include:
- Anticholinergics such as trospium , darifenacin and oxybutynin relax bladder muscles. They are the most commonly prescribed medications for overactive bladder and are well tolerated. Side effects include constipation and dry mouth.
- Tricyclic antidepressants, such as imipramine and doxepin, stop contractions in the smooth muscle of the bladder. Side effects include dizziness, fatigue, changes in vision, nausea, insomnia, and dry mouth.
Drugs For Overactive Bladder
In people with overactive bladder, muscles in the bladder wall contract at the wrong time. A group of drugs called anticholinergics combat this problem by blocking the nerve signals related to bladder muscle contractions. Research suggests that these drugs also might increase bladder capacity and decrease the urge to go.
Anticholinergic drugs include:
Oxytrol for women is the only drug available over the counter. Overall, these drugs work about the same in treating overactive bladder, and generally people tolerate all of them well. The main side effect is dry mouth, but anticholinergics also can cause constipation, blurred vision, and increased heartbeat.
Anticholinergics aren’t right for everyone. Some people with glaucoma, urinary retention, or gastrointestinal disease should avoid using anticholinergic drugs.
The drugs mirabegron and vibegron called beta-3 adrenergic agonists. These medications work by activating a protein receptor in bladder muscles that relaxes them and helps the bladder fill and store urine.
Another type of drug for overactive bladder is the tricyclic antidepressantimipramine hydrochloride , which also relaxes bladder muscles.
Doctors also treat men with drugs that relax a muscle at the bladder neck and prostate to help with emptying. They include:
Evaluation Of Efficacy And Safety
The therapeutic outcomes were evaluated using the OABSS questionnaire . The OABSS questionnaire was completed during the initial examination and at 1 year following treatment initiation. Residual urine was measured through ultrasound. The Vaginal Health Index Scale was used and safety was examined. For VHIS, a system widely used in the field of gynecology, the appearance of vaginal epithelium was evaluated via internal examination performed by a physician. Each parameter was graded on a scale of 15 , with a total score of15 indicating an atrophic condition. Constipation was evaluated using the Constipation Assessment Scale , including eight items scored on a scale of 02 points, with a higher score indicating severe constipation. The degree of mouth dryness was evaluated according to a five-point scale . All other adverse events were recorded by free description. All treatments and examination were administered by a single physician accompanied by professional nurses. The pill counts were not used and the adherence to medication was assessed via interviews with the patient and the family.
Read Also: What Can Help Overactive Bladder
Some Tips To Prevent An Overactive Bladder
-Maintain a healthy weight.
-Do physical activities and exercises.
-Reduce your consumption of caffeine and alcohol.
-Stop smoking: smoking is irritating to the bladder muscle.
-Treat your chronic conditions, such as diabetes, that might lead to overactive bladder symptoms.
-Do Kegel exercises for the pelvic muscles.
Overactive Bladder Treatment In Atlanta Ga

Dr. Rita Sharma provides a variety of treatment options for overactive bladder in Atlanta, GA. IncontiLase® is non-invasive laser therapy for the treatment of mild and moderate stress urinary incontinence, based on non-ablative photothermal stimulation of collagen neogenesis, shrinking and tightening of vaginal mucosa tissue, and collagen-rich endopelvic fascia, and subsequently greater support to the bladder. Call Dr. Sharma today at to find the best OAB treatment option for you!
Don’t Miss: Intravesical Treatments Of Bladder Cancer Review
The Use Of Vaginal Lasers In The Treatment Of Urinary Incontinence And Overactive Bladder Systematic Review
To evaluate the available literature to assess the safety, efficacy, and outcomes of lasers in the treatment of female stress urinary incontinence and overactive bladder .
Pubmed search was conducted up to May 2020, including observational and investigational human studies that documented the effects on laser treatment in SUI and OAB.
A total of 27 studies, recording subjective or objective measures in SUI or OAB were included. Lasers used included Er:YAG and Fractional CO2 lasers. The overall quality of studies was poor, and 23/27 studies were case series . Er:YAG laser showed a modest reduction in mild SUI cases, with benefits lasting a maximum of 13-16 months. Er:YAG laser for OAB showed conflicting results, with a trend to improve OAB symptoms for up to 12 months. Fractional CO2 laser showed an improvement of mild SUI in few studies however, no long-term data are available. For OAB symptoms, studies showed minimal improvement that was evaluated in short term studies. When reported, adverse events were insignificant, however, they were not reported systematically. Several limitations have been noticed in the current literature of vaginal lasers, including large variation in laser settings and protocols, short term follow up, lack of urodynamic evaluation, and appropriate objective measures.
International urogynecology journal. 2020 Nov 11
Ali Alsulihem, Jacques Corcos
Evaluation Of Laser Therapy For Urgency Urinaryincontinence In Females
Ali Abid* and Emmanuel Karantanis
The University of New South Wales, Sydney, Australia
Ali Abid, The University of New South Wales, Sydney,Australia.
Received Date: February 26, 2021 April 06, 2021
Urgency urinary incontinence is a major health problem associated with detriments to the social, mental and economical spheres of an affectedindividuals life. It is a symptom that is implicated in many syndromes such as overactive bladder, genitourinary syndrome of menopause andmixed urinary incontinence. The exact cause of urgency urinary incontinence has not been elucidated however some theories point to detrusoroveractivity, poor bladder compliance and urothelial hypersensitivity as the culprits. The management of urgency urinary incontinence includes astepwise approach beginning with behavioural and lifestyle modifications and physical therapy followed by pharmacological agents and then, forsevere cases, surgical management. Laser therapy is a novel, non-hormonal, minimally invasive treatment approach that is rising in prominence inthe literature. In this review an evaluation of the literature is conducted, appraising any relevant studies to determine if laser therapy is a viablemanagement approach. Our finding is that at this current juncture there is not enough evidence to support the implementation of laser therapy forurgency urinary incontinence.
Urinary incontinence
Mechanism of urgency incontinence
Management
Laser therapy
Hypothesis
Don’t Miss: Can Spinal Stenosis Cause Bladder Problems
What Is Laser Therapy For Female Incontinence
Laser stands for light amplitude by stimulated emission of radiation . Fancy doctor term for changing light or electrical energy into a focused beam of energy. A âlaser beamâ.
Laser therapy for female incontinence is typically delivered in an office setting while you are awake. During the therapy sessions, the laser is directed to the vaginal lining to cause changes to the pelvic tissues supporting the urethra and bladder.
When Do You See Votiva Treatment Results
You may begin to experience good effects as soon as the day following the initial treatment. Your vaginal skin may appear tighter, and your labia may appear smaller. Additionally, you should find greater control over your bladder when you sneeze, cough, or laugh.
We want you to understand that you are not alone in your battle against urine incontinence. Call or book an appointment online with our Edmonton, Alberta location and prepare to experience nothing but bliss the next time you laugh.
Don’t Miss: Side Effects Of Bladder Cancer
Er: Yag Laser Therapy For Female Incontinence
Er:YAG or erbium-doped yttrium aluminium garnet refers to the crystal used in the laser device. It is strongly absorbed by water and has numerous applications in dentistry and cosmetics.
The primary Er:YAG laser therapy for female incontinence is the:
- Fotona SMOOTH® IncontiLase®.
When Er:YAG laser therapy is used for female incontinence, it causes a controlled heating of the collagen in the deeper vaginal layers without harming the delicate inner lining or mucosa. This causes new collagen formation and tightening of the surrounding pelvic tissues.
Laser therapy sessions are delivered in the office in about 20 minutes. Usually no anesthesia is required and most women report little to no pain. Other women report more of a âwarmâ sensation during the treatments and local anesthesia creams can be used.
Expect a quick recovery with this non-invasive, non-ablative laser therapy for female incontinence. Anywhere from 2 to 3 sessions are typically delivered.
Side Effects And Complications From Treatment For Enlarged Prostate With Greenlight Laser Surgery
Some men develop side effects and complications after treatment for BPH with Greenlight laser or other lasers used for the treatment of enlarged prostate.
These complications are not unique to the Greenlight laser procedure and can occur after any transurethral procedure performed on the prostate .
There several side effects and complications that could occur after laser treatment of a large prostate. The most common side effects and complications include persistent hematuria or bleeding, persistent frequent urination and urgency to urinate, urinary incontinence or leakage, and burning with urination.
Read Also: Can Candida Cause Bladder Infection
Botulinum Toxin Injections For Oab
You might be wondering, “Botox? Like movie stars use on their forehead?” Yes, the same substance that dermatologists use to smooth out wrinkles can also be used to relax an overactive bladder.
To treat incontinence, doctors inject botulinum toxininto the bladder muscle. This is done with a needle that is inserted via a long tube called a cystoscope that goes up into the bladder. “The goal is to reduce the over-activity of the bladder muscle so that the patient has better control, but still allow enough muscle contraction to empty the bladder,” Rames says. The effects generally last for about 9 months. So far there don’t seem to be any major side effects from botulinum toxin, although it’s only recommended if your symptoms aren’t controlled with behavioral therapies, medications, or a combination of both.
Show Sources
Linda Brubaker, MD, professor, department of obstetrics & gynecology and urology, Loyola University Chicago Stritch School of Medicine, Chicago.
Ross Rames, MD, associate professor of urology, Medical University of South Carolina, Charleston.
UpToDate: “Treatment of Urinary Incontinence.”
National Association for Continence: “Overactive Bladder Treatment.”
Duthie JB. Cochrane Summaries, Dec. 7, 2011.
National Association for Continence: “Urgency Urinary Incontinence/Overactive Bladder.”
News release, FDA.
Monalisa Touch For Urinary Incontinence
If you suffer from urinary incontinence, you understand the impact it can have on a womans life. Many women are unable to play sport, run, jump, sneeze or cough without the embarrassment of being incontinent. Others find that a sudden urgent need to use the toilet affects daily activities and undermines their confidence. Its a problem that is not only limited to post-menopausal women or those who have had babies it can affect women of all ages and life situations.
Dr Ljiljana understands the impact incontinence has on womens lives and is committed to providing the best health care possible. She was the first gynaecologist in Newcastle to offer MonaLisa Touch, a treatment which is effective in treating urinary incontinence.
What Is Urinary Incontinence?
Urinary incontinence is when urine leaks involuntarily from the bladder. The urinary sphincter should enable control over urination, but when it is weak or damaged, the flow of urine is uncontrolled.
Symptoms of Urinary Incontinence
The symptoms of urinary incontinence include:
- An urgent need to urinate, followed by involuntary urination
- Small amounts of urine leakage
- Bladder may completely empty involuntarily
- Urine leakage from exertion such as running, jumping, sneezing, coughing or lifting heavy objects
- A frequent or constant dribbling of urine from the bladder not emptying completely
Types of Urinary Incontinence
There are two main types of urinary incontinence that affect women. They are:
Benefits of Mona Lisa Touch
Read Also: Bcg Dose For Bladder Cancer
Percutaneous Tibial Nerve Stimulation
If your overactive bladder hasn’t improved with lifestyle changes and medicines and you don’t want to have surgery, percutaneous tibial nerve stimulation is an option. During this technique, the doctor inserts a fine-needle electrode into the nerve just above your ankle. A mild electrical impulse is passed along the needle to nerves of the spine that control bladder function.
“It’s a fairly simple procedure, done in the office,” says Ross Rames, MD, associate professor of urology at the Medical University of South Carolina. Rames works with the university’s Bladder and Pelvic Health Center. “Often, we’ll see improvement within the first couple of weeks after the patient starts PTNS treatments.” With PTNS, you’ll need a series of 12 treatments, scheduled about a week apart. You may need more than one treatment to keep seeing results.
Pelvic Floor Muscle Training
Your pelvic floor muscles surround the bladder and urethra and control the flow of urine as you pee.
Weak or damaged pelvic floor muscles can cause urinary incontinence, so exercising these muscles is often recommended.
A GP may refer you to a specialist to start a programme of pelvic floor muscle training.
The specialist will assess whether you’re able to squeeze your pelvic floor muscles and by how much.
If you can contract your pelvic floor muscles, you’ll be given an exercise programme based on your assessment.
Your programme should include a minimum of 8 muscle contractions at least 3 times a day and last for at least 3 months. If the exercises are helping after this time, you can keep on doing them.
Research has shown that pelvic floor muscle training can benefit everyone with urinary incontinence.
Find out more about pelvic floor exercises.
Recommended Reading: Does Overactive Bladder Come On Suddenly
Vaginal Co2 Laser In Postmenopausal Women With Overactive Bladder Syndrome
| The safety and scientific validity of this study is the responsibility of the study sponsor and investigators. Listing a study does not mean it has been evaluated by the U.S. Federal Government. Read our disclaimer for details. |
| Verified June 2020 by Themos Grigoriadis, National and Kapodistrian University of Athens. Recruitment status was: RecruitingFirst Posted : February 20, 2019Last Update Posted : July 1, 2020 |
- Study Details
| Device: Microablative Fractional CO2 laser | Not Applicable |
| Study Type : |
| Quadruple |
| Primary Purpose: |
| The Role of the Micro-ablative Fractional CO2 Laser in Postmenopausal Women With Overactive Bladder Syndrome. |
| Actual Study Start Date : |
Microablative Fractional CO2 laser therapy at monthly intervals.
The laser parameters that will be used are the following:
Placebo CO2 laser therapies at monthly intervals.
The laser parameters that will be used are the following:
What Is Urinary Incontinence
Urinary Incontinence is involuntary loss of urine. The person will have no control on urine leakage. Vaginal birth is a leading cause of Urinary Incontinence in women. Along with that, age related changes such as the drop in estrogen levels that manage the tissues in the pelvis region also contribute to incontinence post menopause.
Recommended Reading: Loss Of Bladder Control When Running
Is Urinary Incontinence Treatment Painful
This is a frequently asked question, and we are pleased to inform you that the answer is no. A mild anesthetic gel will be applied around the opening of your vagina, and you should have no sensations save for minor warmth. If you have severe vaginal dryness, you may experience some discomfort when the handheld device is placed into your vagina for the first time.
Following the treatment, you may experience sensitivity when wiping after using the restroom. However, you will feel no pain during or after the surgery. You must abstain from sexual activity and avoid hot baths, pools, and bathtubs for three days following the therapy.
What Is The Mechanism Of Action Of Incontilase
IncontiLase is a non-invasive, painless laser therapy that is extremely successful. During the operation, a specific attachment is put into the vagina, comparable to a speculum used during a pap test. The vaginal area is treated with brief laser pulses delivered via a tiny handpiece. Photothermal heating has an effect on the collagen in both the vaginal and urethral walls. This results in collagen remodeling and regeneration. As a result, the vaginal walls and urethra become thicker and tighter, preventing urine loss. Additionally, it will help to tighten the vagina.
Clinical trials have demonstrated that IncontiLase is an effective, safe, and pleasant therapy option for people with mild to severe SUI.Ninety-four percent of women reported considerable improvement in Stress Urinary Incontinence. After 120 days, 68% were entirely rid of Stress Urinary Incontinence SUI.
You May Like: Malignant Neoplasm Of Overlapping Sites Of Bladder
The Emsella Chair: A Urinary Incontinence Treatment That Works
No one likes to talk about the unglamorous world ofbladder control. But did you know that urinaryincontinence affects a significant amount of women?One poll found that up to 43% of women over 50suffer from it to some degree.
So if its that common, what kind of advances havebeen made in the field of urinaryincontinence treatments? Surely theressomething easier than the prescribed 1,000+ Kegelexercises you need to keep up with every day, andsomething less invasive than surgical procedures orlaser treatments?
Behavioral Modification For The Treatment Of Overactive Bladder
Various types of behavioral modifications may also be recommended for the treatment of overactive bladder. Examples include:
- Dietary Changes: Decreasing water consumption throughout the day can help reduce leakage, as can avoiding substances that irritate the bladder, such as caffeine, fruit juices, and spicy foods.
- Bladder Retraining: This method uses a set schedule for urination throughout the day. Between these times, no urination is allowed, even if leaks occur. The goal is to increase the time between bathroom visits to three to four hours.
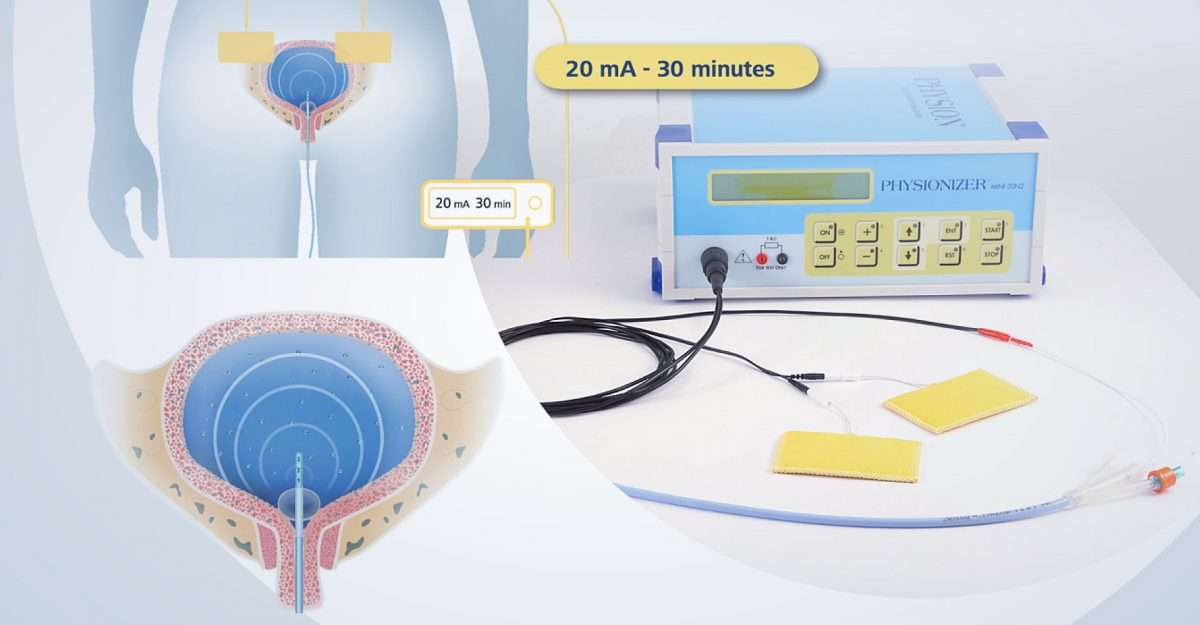
- Electrical Stimulation and Biofeedback: This technique provides information about when a patient is squeezing the muscles of her pelvic floor. A sensor is placed in the vagina or anus so that pelvic floor muscle contractions can be recorded. Exercises can help strengthen weak pelvic floor muscles, and if they don’t respond, electrical stimulation can activate the appropriate muscles.
You May Like: Bladder Cancer Spread To Lungs Life Expectancy