Treatment Strategy For Newly Diagnosed T1 High
- Zachary KlaassenAffiliationsDivision of Urology, Department of Surgery, University Health Network, Princess Margaret Cancer Centre, University of Toronto, Toronto, ON, Canada
- Bas W.G. van RhijnAffiliationsDepartment of Surgical Oncology, Division of Urology, Netherlands Cancer Institute Antoni van Leeuwenhoek Hospital, Amsterdam, The Netherlands
- These authors share co-senior authorship.James W.F. Catto These authors share co-senior authorship.Affiliations
- These authors share co-senior authorship.Girish S. KulkarniCorrespondenceCorresponding author. Division of Urology, Department of Surgery, Institute for Clinical Evaluative Sciences, University Health Network, Princess Margaret Hospital, 610 University Avenue, Suite 3-130, Toronto, ON M5G 2M9, Canada. Tel. +1 416 946 2246. These authors share co-senior authorship.AffiliationsDivision of Urology, Department of Surgery, University Health Network, Princess Margaret Cancer Centre, University of Toronto, Toronto, ON, Canada
- These authors share co-senior authorship.
What To Do Before And After Treatment
Talk with your doctors about whether you need to do anything to prepare for treatment and help your recovery. Some things they may suggest are to:
- Stop smoking if you smoke, aim to quit before starting treatment. If you keep smoking, you may not respond as well to treatment and you may have more treatment-related side effects. Continuing to smoke also increases your risk of cancer returning.
- Begin or continue an exercise program exercise will help build up your strength for treatment and recovery. It can also help you deal with side effects of treatment.
- Improve diet aim to eat a balanced diet with a variety of fruit, vegetables, wholegrains and protein. Eating well can improve your strength and you may respond better to treatment.
- See a physiotherapist they can teach you exercises to strengthen your pelvic floor muscles, which help control how your bladder and bowel work. These exercises are useful if you have a neobladder, a partial cystectomy, or radiation therapy.
You May Like: How To Fix Bladder Leakage After Pregnancy
Questions To Ask The Doctor
- What treatment do you think is best for me?
- Whats the goal of this treatment? Do you think it could cure the cancer?
- Will treatment include surgery? If so, who will do the surgery?
- What will the surgery be like?
- How will I pee after surgery?
- Will I have other types of treatment, too?
- Whats the goal of these treatments?
- What side effects could I have from these treatments?
- Is there a clinical trial that might be right for me?
- What about treatments like special vitamins or diets that friends tell me about? How will I know if they are safe?
- What should I do to be ready for treatment?
- Is there anything I can do to help the treatment work better?
- Whats the next step?
You May Like: Can A Prolapsed Bladder Cause Back Pain
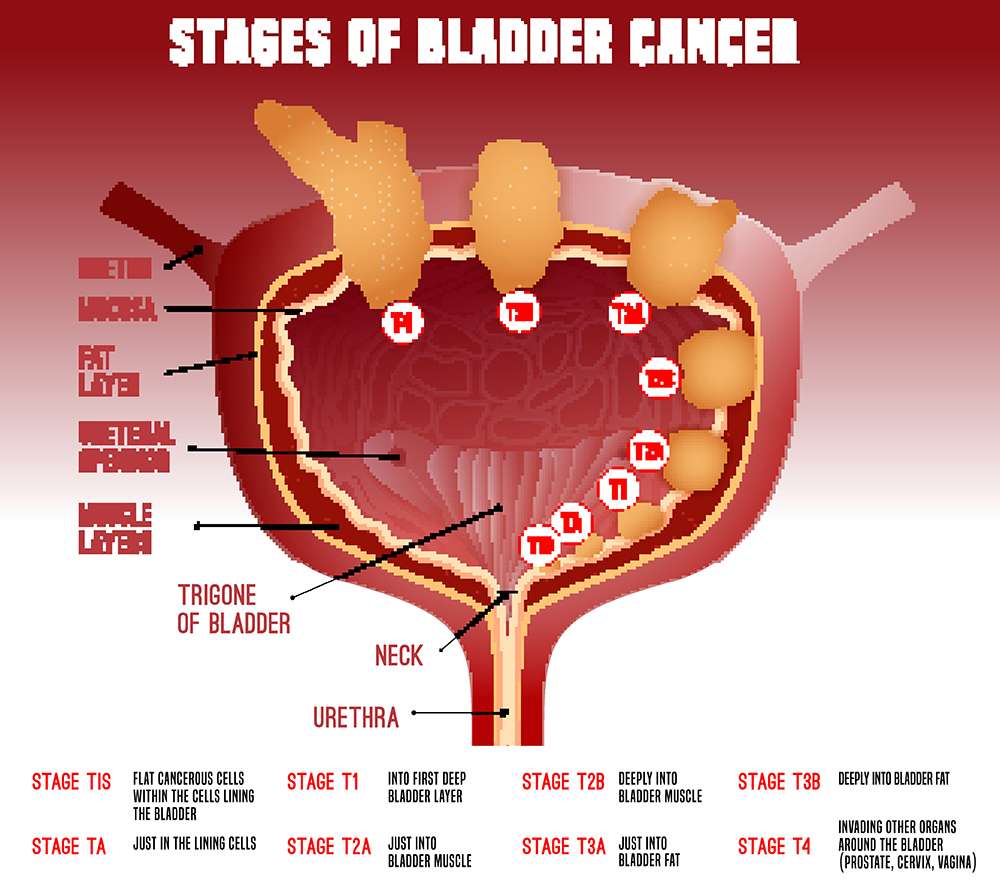
Where Does Bladder Cancer Start
Bladder cancer is a growth that starts in the inner wall of the bladder, the organ that collects and expels urine created by the kidneys. The bladder has three layers of muscular walls that make up its structure. 1 A cancerous growth in the bladder can grow uncontrollably and start spreading to other parts of the body.
Bladder Cancer: Stage 2 High Grade
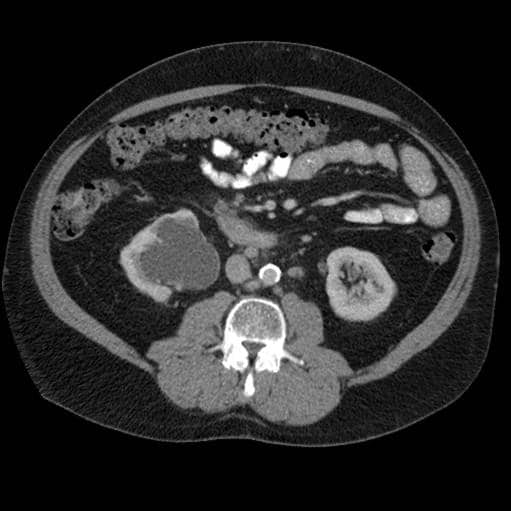
My husband was just diagnosed with Stage 2 high grade bladder cancer. The cancer has invaded the muscle wall but had not gone though it. He had a cat scan which showed no spreading of the disease, in particular, lymph nodes unremarkable. We made the trip to the Mayo Clinic and the urologist noticed what he thought was an enlarged lymph node. The doctor suggested a pet scan. The pet scan was conducted and shows 4 suspicious hypermetobolic lymph nodes in the abdomen. Needless to say we are scared and very confused as we though it was stage 2 and could be cured. We are going through the process of starting chemo, doing all tests, insurance approval, etc. As we understand it, at this point, surgery can not be done to remove these nodes, since they are too deep in the abdomen. We were supposed do 4 chemo cycles and then have bladder and prostate removed. We have a follow up with oncologist in two days . Since this is the weekend and we found this out on Friday afternoon, we are left with so many questions. Has anyone experienced something similar?
Don’t Miss: Natural Ways To Help Overactive Bladder
Is High Grade T1 A Bad Prognosis
High-grade T1 bladder cancer has a poor prognosis due to a higher incidence of recurrence and progression than other nonmuscle invasive bladder cancer thus patients with high-grade T1 have to be carefully monitored and managed. If patients are diagnosed with high-grade T1 at initial transurethral resection , a second TUR is strongly recommended regardless of whether muscle layer is present in the specimen because of the possibility of understating due to incomplete resection. Since high-grade T1 disease shows diverse clinical courses, individual approaches are recommended for treatment. In cases with low risk of progression, cystectomy could represent overtreatment and deteriorate quality of life irreversibly, while, in those with high risk, bacillus Calmette-Guérin therapy may worsen survival by delaying definitive therapy. Therefore, a strategy for predicting prognosis based on the risk of progression is needed for managing high-grade T1 disease. Molecular risk classifiers predicting the risk of progression and response to BCG may help identify the optimal management of high-grade T1 disease for each individual.
Newly Diagnosed With Bladder Cancer
Take a big breath. If you are like most people that are newly diagnosed, panic and fear are at least part of what you are experiencing. You may be asking yourself “What is my prognosis? How will this affect my life?”. This site was built for and by bladder cancer survivors and the people that care about them. No matter what path your bladder cancer journey takes, know that there are others here that will share the journey with you.
And to add even more complexity to this emotional storm is the fact that you have to learn enough about your diagnosis to make informed decisions. While knowledge is power, it needs to be the right information that fits your situation and is reliable. No matter your approach to learning while using the internet, please keep in mind the following:
Don’t Miss: Does Azo Bladder Control Cause Weight Gain
Localized Transitional Cell Cancer Of The Renal Pelvis And Ureter
Standard treatment options:
Treatment options under clinical evaluation:
The development of new instrumentation for endourological treatment of uppertract transitional cell cancer has provided new options for regional managementof these cancers. Introduction of electrofulguration and resection instrumentsor laser probes either transureterally or percutaneously may permit destructionof a primary cancer. Introduction of cytotoxic agents has also been employed. Although a biopsy can be taken for staging purposes, the accuracy of thisremains to be determined. The efficacy of treatment by these maneuvers has notbeen established.
Dose Modifications For Adverse Reactions1
- Withhold or discontinue TRODELVY to manage adverse reactions as described in the table below
- Do not re-escalate the TRODELVY dose after a dose reduction for adverse reactions has been made
- Slow or interrupt the infusion rate of TRODELVY if the patient develops an infusion-related reaction
- Permanently discontinue TRODELVY for life-threatening infusion-related reactions
- Severe hypersensitivity reaction to TRODELVY.
WARNINGS AND PRECAUTIONS
Neutropenia: Severe, life-threatening, or fatal neutropenia can occur and may require dose modification. Neutropenia occurred in 61% of patients treated with TRODELVY. Grade 3-4 neutropenia occurred in 47% of patients. Febrile neutropenia occurred in 7%. Withhold TRODELVY for absolute neutrophil count below 1500/mm3 on Day 1 of any cycle or neutrophil count below 1000/mm3 on Day 8 of any cycle. Withhold TRODELVY for neutropenic fever.
ADVERSE REACTIONS
In the ASCENT study , the most common adverse reactions were fatigue, neutropenia, diarrhea, nausea, alopecia, anemia, constipation, vomiting, abdominal pain, and decreased appetite. The most frequent serious adverse reactions were neutropenia , diarrhea , and pneumonia . SAR were reported in 27% of patients, and 5% discontinued therapy due to adverse reactions. The most common Grade 3-4 lab abnormalities in the ASCENT study were reduced neutrophils, leukocytes, and lymphocytes.
DRUG INTERACTIONS
Please see full Prescribing Information, including BOXED WARNING.
Read Also: Why Does My Bladder Burn
Prognosis And Life Expectancy
In general, papillary urothelial cancers have a better prognosis than other types of bladder cancer. Your specific outlook depends on the stage and grade of your cancer. High-grade cancers can spread. Low-grade papillary cancers are less likely to spread. Papillary cancers can also return after theyve been treated.
The most common treatments for muscle-invasive bladder cancer are radical cystectomy and radiation therapy. There is no strong evidence from randomized controlled trials to determine whether surgery or radiation therapy is more effective. There is strong evidence that both therapies become more effective when combined with chemotherapy. The treatments with the highest level of evidence supporting their effectiveness are radical cystectomy preceded by multiagent cisplatin-based chemotherapy and radiation therapy with concomitant chemotherapy.
Radical cystectomy
Evidence :
Segmental cystectomy
Treatment Of Stage Iv Bladder Cancer
For information about the treatments listed below, see the Treatment Option Overview section.
Treatment of stage IV bladder cancer that has not spread to other parts of the body may include the following:
- Urinary diversion or cystectomy as palliative therapy to relieve symptoms and improve quality of life.
Treatment of stage IV bladder cancer that has spread to other parts of the body, such as the lung, bone, or liver, may include the following:
- External radiation therapy as palliative therapy to relieve symptoms and improve quality of life.
- Urinary diversion or cystectomy as palliative therapy to relieve symptoms and improve quality of life.
- A clinical trial of new anticancer drugs.
Use our clinical trial search to find NCI-supported cancer clinical trials that are accepting patients. You can search for trials based on the type of cancer, the age of the patient, and where the trials are being done. General information about clinical trials is also available.
Also Check: Early Signs Of Bladder Infection
How Many People Will Die From Bladder Cancer In 2020
Bladder cancer is the sixth most common cancer in the United States, representing 4.5% of all new cancer cases in the country. 1 There were an estimated 81,400 new cases of bladder cancer in 2020. This form of cancer resulted in about 17,980 deaths in the same year. While bladder cancer is relatively common, the average five-year survival rate is quite high at 76.9%. This rate has improved over the past several years, and a persons chance of survival is influenced by many factors.
What Is The Prognostic Factor For T1
The European Organization for Research and Treatment of Cancer investigated 194 high-grade T1 patients with a median follow-up of 3.9 years and suggested that the most important prognostic factor in patients with high-grade T1 tumors is the presence of concomitant CIS . High-grade T1 patients without CIS had a probability of progression of 10% after 1 year and 29% after 5 years. By contrast, these rates for high-grade T1 patients with CIS were 29% and 74%, respectively. Denzinger et al. also reported that CIS was associated with recurrence, progression, and cancer-specific survival in 132 high-grade T1 patients who received BCG induction therapy. Palou et al. conducted a retrospective analysis of 146 patients with high-grade T1 detected in initial TUR over a median follow-up period of 8.7 years. None of the patients underwent a second TUR, and 44.5% of the patients had recurrence, 17.1% had progression, and 12.3% died of cancer. The authors suggested that female gender and the presence of CIS in the prostatic urethra were independent prognostic factors for progression and survival. Recently, Gontero et al. carried out a retrospective study with 2,451 high-grade T1 patients from 23 centers, and suggested that age 70 years, tumor 3 cm, and concomitant CIS were the most important factors for progression.
You May Like: Do You Need Antibiotics For Bladder Infection
What Other Types Of Bladder Cancer Are There
Several less common types of bladder cancer make up the remaining approximately 10% of bladder cancers. Some examples of the uncommon types include:
- Squamous cell carcinoma: Squamous cells develop in the lining of the bladder as a result of irritation or inflammation. These cells may eventually become cancerous. Although squamous cell carcinoma is uncommon, making up around 4% of all bladder cancers,2 it has a high likelihood of progression.
- Adenocarcinoma: This type of bladder cancer consists of glandular-type cells and is usually invasive. Overall, around 2% of bladder cancers are adenocarcinomas.2
- Small cell carcinoma: Small cell carcinomas of the bladder start in nerve-like cells. This bladder cancer type is rare, accounting for less than 1% of bladder cancers,4 but can grow rapidly and spread to other parts of the body.
- Sarcoma: A sarcoma is a type of cancer that begins in the bodys supporting tissues, such as bone, muscle, fibrous tissues, and fat. Very rarely, sarcomas may arise from the muscle or fat layers of the bladder.
Although the treatment for most bladder cancer types is similar for early-stage tumors, different drugs may be used if chemotherapy is undertaken.
The Effect Of Age At Diagnosis With Pancreatic Cancer Metastasis To Liver
The Kaplan Meier survival curve showed significant difference in overall survival for patients diagnosed at different age groups . The overall survival time was negatively correlated with the age at diagnosis. Among the three groups, the prognosis of patients diagnosed at age less than 52 years old was the best, and of which the median survival time was 1 year. .
Kalpan Meier survival curve showing the effect of age at diagnosis with pancreatic cancer metastasis to liver.
Recommended Reading: Antibiotics For Bladder And Kidney Infection
What Is The Most Common Form Of Bladder Cancer
Urothelial bladder cancer is the most common form of bladder cancer in the United States. 1 It affects about 90% of people who are diagnosed with bladder cancer. Cancer is diagnosed based on where the cancer cells began to form. In most people with bladder cancer, the cancer cells started forming in a part of the bladder called the urothelium.
What Is The Most Common Type Of Bladder Cancer
The most common cell type of bladder cancer is urothelial cancer , and about 70%80% of these are nonmuscle invasive bladder cancers , while the other 20%30% are muscle invasive bladder cancers . MIBC has a poor prognosis due to invasion or metastasis to other organs. NMIBC has a high recurrence rate and progression , and thus is a great burden to patients . Moreover, T1 disease, which invades the lamina propria, and poorly differentiated high-grade disease have a poor prognosis due to a higher incidence of recurrence and progression than other NMIBC thus patients with high-grade T1 have to be carefully monitored or managed. Although bacillus Calmette-Guérin followed by transurethral resection is known as the gold standard treatment, controversies remain over whether BCG can reduce the progression rate of highgrade T1 . One third of high-grade T1 patients who receive intravesical BCG therapy progress to MIBC and are at risk of dying from bladder cancer because ineffective BCG therapy delays radical cystectomy . Nevertheless, there is no consensus about how to predict progression and manage high-grade T1 disease. Herein, this review describes how to stratify high-grade T1 disease to predict progression and how to manage it properly by reducing over or under treatment.
Recommended Reading: Antibiotics For Uti Bladder Infection
Molecular Risks For Progression And Survival In High
It is questionable whether the gene expression patterns of T1 with progression to MIBC on follow-up and those without progression are different from those of T2 cancer, since the gene expression patterns of T1 with progression at initial diagnosis should already show a T2 pattern. Therefore, we conducted unsupervised hierarchical clustering using 70 patients with T1 who did not experience progression, 10 T1 who experienced progression, and 26 with T2 disease . The result was interesting. T1 patients without progression and T2 patients were relatively well categorized separately. However, 4 of 10 patients with T1 who experienced progression belonged to the T1 without progression cluster, whereas the other 6 of 10 belonged to the T2 cluster . Interestingly, three of four patients with high-grade T1 who experienced progression were categorized as T2. This means that the gene expression patterns of high-grade T1 might already have MIBC characteristics at initial diagnosis. Similarly, Hurst et al. performed an integrated genomic analysis of 49 high-grade T1 tumors. The authors investigated the copy number alteration and mutations in tumor tissues and suggested that the high-grade T1 tumors separated into three major subgroups and one minor subgroup, although they did not clearly describe whether these clusters were associated with progression or survival.
Summary Ofevidence And Guidelines For Metastatic Disease
|
Summary of evidence |
|
In a first-line setting, performance status andthe presence or absence of visceral metastases are independent prognosticfactors for survival. |
|
In a second-line setting, negative prognostic factorsare: liver metastasis, PS 1 and low haemoglobin . |
|
Cisplatin-containing combination chemotherapy canachieve median survival of up to 14 months, with long-term disease-free survival reported in ~15% of patients with nodal disease and good PS. |
GC = gemcitabine plus cisplatin FGFR =fibroblast growth factor receptor HD-MVAC = high-dose intensity
methotrexate, vinblastine, adriamycin plus cisplatin.
Figure 7.2: Flow chart for the management of metastatic urothelialcancer*
*Treatment within clinical trials is highly encouraged.
BSC = best supportive care CR = complete response DD-MVAC = dose dense methotrexate vinblastine doxorubicin cisplatin EV = enfortumabvedotin FDA = US Food and Drug Administration FGFR = pan-fibroblast growth factorreceptor tyrosine kinase inhibitor GFR = glomerular filtration rate IO =immunotherapy PR = partial response PS = performance status SD = stable disease.
Read Also: How To Live With Overactive Bladder
Recommended Reading: What Does Overactive Bladder Mean