What Can I Do If I Have Urinary Incontinence
Your urinary incontinence may have come on slowly, building over the years to the point you now feel youre ready to treat it. Or, you may have just started experiencing incontinence.
Either way, treatments are available. Incontinence is a condition that is very common, but its not normal, and its something no one should have to live with.
Here are some first steps you can take to start working toward a treatment plan:
What Kind Of Surgeries Are There
In either case, though, the goals of the surgery are the same to create a strong support to prevent the organs from falling down. Many surgeons use plastic material called mesh to support the tissue, but this may result in serious complications . Dr. Blaivas does not do these mesh surgeries they use only your own natural tissue for the repair.
If the uterus is prolapsed it may be necessary to have a hysterectomy as well. In addition, it may be necessary to repair incontinence.
So if you are considering surgery, be sure that you do your homework and learn a lot about the different surgical possibilities, the potential risks and benefits, and most importantly, about how to select your doctor.
Blood And Urine Tests
The following tests are routinely performed in the evaluation of a patient with suspected Sjogrens syndrome:
Also Check: What Does A Tumor In The Bladder Mean
Prolapsed Bladder Care At Home
For mild-to-moderate cases of prolapsed bladder, the doctor may recommend activity modification such as avoiding heavy lifting or straining. The doctor may also recommend Kegel exercises. These are exercises used to tighten the muscles of the pelvic floor. Kegel exercises might be used to treat mild-to-moderate prolapses or to supplement other treatments for prolapses that are more serious.
Managing Bladder And Bowel Incontinence
Some common treatments are:
-
Changes in food or drink. Increasing your fiber intake can help manage diarrhea and constipation. Drinking plenty of fluids can also ease constipation. Not drinking fluids at certain times can help manage overactive bladder and urinary incontinence.
-
Exercises. Kegel exercises can strengthen the sphincter muscles and pelvic floor. This can help you have better control.
-
Medicines. Some medicines can help control bowel incontinence. Antidiarrheal medicines can help manage diarrhea. And medicine can help bladder muscles relax to give you better control.
-
Keeping a bathroom schedule. Setting a regular schedule for using the toilet can give you better control. This includes attempting to urinate or move your bowels at the same time each day.
-
Electrical stimulation. This therapy can stimulate damaged nerves. This may give you better muscle control in your bladder or bowel.
-
Surgery. In rare cases, you may need surgery to repair damage to muscles or nerves.
Your healthcare provider will work with you to create a treatment plan.
Read Also: Foods That Help Overactive Bladder
Risks Of Oab And Bps/ic
Compared with the comparison cohort, pSS patients exhibited significantly increased risks of OAB and BPS/IC . shows the disease-free survival curves of OAB and BPS/IC using the KaplanMeier method. The five-year OAB and BPS/IC-free survival rates for the pSS cohort were significantly lower compared to the control cohort .
Comparisons of probabilities of OAB and BPS/IC-free, OAB-free, BPS/IC-free survival between pSS and comparison cohorts. pSS: Primary Sjögren syndrome OAB: overactive bladder BPS: bladder pain syndrome IC: interstitial cystitis.
What Other Neuropathies Can Occur With Sjgrens Syndrome
1. Autonomic Neuropathy
Sjögrens syndrome can cause nerve damage which regulates the coordination of heartbeat, respiration, and gastric motility. This is called an autonomic neuropathy. Examples of symptoms include lightheadedness when standing, decreased or increased sweating, and feeling full despite eating small meals. The diagnosis of autonomic neuropathy should be made by a neuromuscular specialist.
2. Trigeminal Neuralgia and Glossopharyngeal Neuralgia
Sjögrens syndrome can cause a numbness or burning of the face, called trigeminal neuralgia. Pain in the back of the throat, which may worsen while swallowing, is called glossopharyngeal neuralgia. Patients with trigeminal or glossopharyngeal neuralgia can have agonizing mouth and facial pain. These neuropathies may co-exist with other neuropathies in different parts of the body. For example, up to 20% of patients with a small-fiber neuropathy may also have trigeminal neuropathy.
3. Mononeuritis Multiplex
The pace of recovery from mononeuritis multiplex can be frustratingly slow. In some cases, it may be difficult to determine whether the slow pace of recovery is a manifestation of the slow process of healing and rewiring, or is due to ongoing and ineffectively treated inflammation. In such cases, repeat nerve-conduction tests may be important. Immunosuppressant medications which may be used in the pattern of mononeuritis multiplex includes cyclophosphamide, azathioprine, as well as prednisone.
Also Check: How Does Azo Bladder Control Work
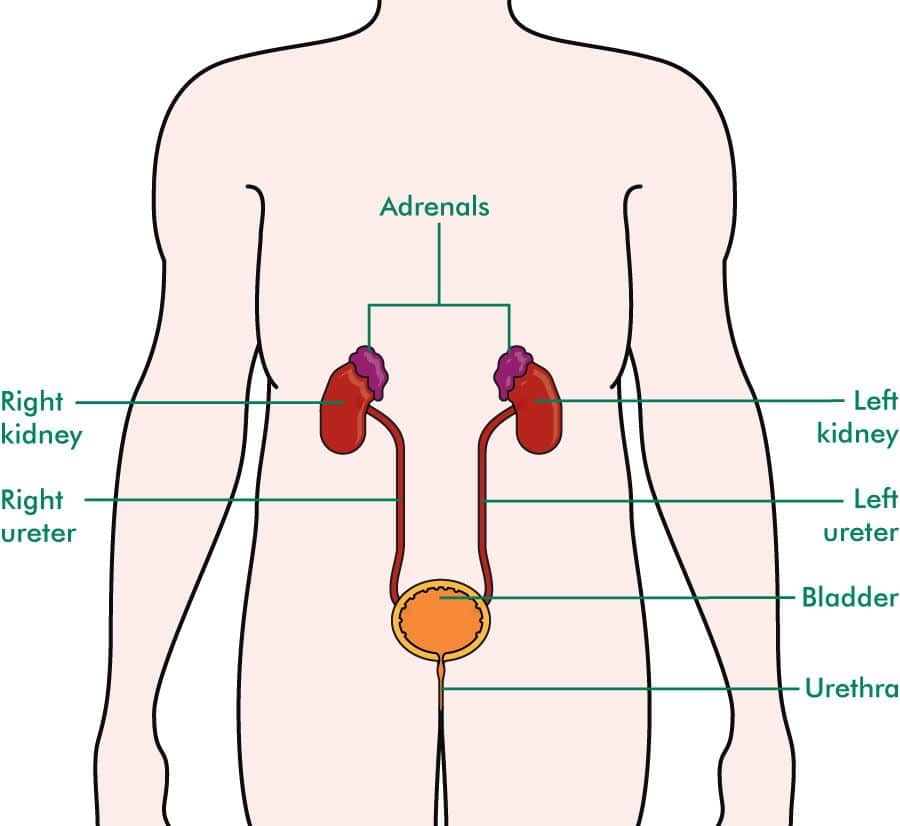
What Are Urinary Tract Infections
A urinary tract infection is an infection anywhere in the urinary tract. Normal urine is sterile. It contains fluids, salts, and waste products, but it is free of bacteria, viruses, and fungi. An infection occurs when microorganisms, usually bacteria from the digestive tract, cling to the urethra, or opening to the urinary tract, and begin to multiply.
Instructions For Modified Kegel Exercises
Vaginal muscle control is best obtained when sitting. While sitting, tighten the vaginal and abdominal muscles, then quickly release them. Repeat ten times, quickly tightening and then releasing the vaginal and abdominal muscles. Next, tighten the vaginal and abdominal muscles, but this time hold it for ten seconds. Repeat ten times, tightening and holding the muscles for ten seconds each time. Completing both exercises takes about ten minutes. Perform these exercises three times a day, morning, noon, and night. If you are using a pessary, remove it before starting the exercises. The exercises cannot be done effectively while wearing a pessary.
Most women see an improvement from these simple exercises within a couple of weeks, or, with a more significant prolapse, within a couple of months. They can be done while sitting at a desk, sitting on a couch, or while commuting. And because exercise is non-invasive and there is a good chance it will improve or reverse a first-degree or second degree prolapse, it is well worth the minimal time and effort to do them three times a day.
It is important that these exercises be performed for 10 minutes three times a day, every day. If you do not experience significant improvement within two to three months, the modified Kegel exercises are probably not going to resolve your prolapse.
You May Like: Difference Between Uti And Bladder Infection Symptoms
Risk Factors For Bladder Prolapse
Risk factors for bladder prolapse include anything that puts pressure on the pelvic floor and affects its function, such as:
- pregnancy and childbirth
- regularly straining on the toilet to pass bowel motions or empty the bladder
- being overweight
- chronic cough secondary to smokers cough or chronic lung diseases
- repetitive lifting of children or heavy weights at work or in the gym, or any exercises where there is excessive downward pressure on the pelvic floor
- pelvic or gynaecological surgery
- strong family history
- connective tissue disease, in which the tissues in the body are not able to hold the weight of the organs
What Can Be Expected After Treatment For A Cystocele
In mild cases, non-surgical treatments may be all that is needed to successfully deal with a cystocele.
When surgery is performed for more serious cases, some women will eventually need another surgery because the first surgery failed, the cystocele returned or another pelvic floor problem developed. Women who are older, who smoke, have diabetes, or who have had a hysterectomy, may be at higher risk for complications.
Read Also: Uti Bladder Infection Home Remedy
The Best Treatment For Prolapsed Bladder
Are you suffering from a prolapsed bladder? If so, Renew Wellness & Aesthetics can help you determine the best treatment for you. In addition, we offer a variety of sexual wellness services for both men and women.
If you have any questions for us, call 405-810-5944 or schedule a consultation online. We look forward to helping you get rejuvenated and feel your best!
GET STARTED
Stimulated Myoplasty For Bladder Emptying
Latissimus dorsi has also been used for myoplasty.Von Heyden etal. studied free latissimus dorsi muscle flaps for bladder myoplasty in dogs revascularization and electrical stimulation of the thoracodorsal nerve successfully induced pressures sufficient for partial evacuation of the bladder. The advantage of a singular nerve supply with ample geometry provided by the latissimus dorsi free flap led to the first clinical application in 1998 byStenzl etal. . Three patients with bladder acontractility were treated with latissimus dorsi myoplasty, and all three were able to void by abdominal straining. In a larger clinical study using the free transfer of the latissimus dorsi muscle to restore voluntary voiding, 14 of 20 patients were able to void spontaneously with postvoid residual volumes of less than 100mL .The largest latissimus dorsi detrusor myoplasty experience was reported byGakis etal.in 24 patients with detrusor underactivity requiring CIC and a mean followâup of 46 months. Latissimus dorsi detrusor myoplasty resulted in complete voluntary voiding in 71% of patients with a 91% reduction in UTIs. Three patients reduced the frequency of catheterization by 50%, and 4 patients had no improvement.
You May Like: Can You Treat A Bladder Infection Without Antibiotics
Warning Disclaimer Use For Publication
WARNING: Please DO NOT STOP MEDICATIONS without first consulting a physician since doing so could be hazardous to your health.
DISCLAIMER: All material available on eHealthMe.com is for informational purposes only, and is not a substitute for medical advice, diagnosis, or treatment provided by a qualified healthcare provider. All information is observation-only. Our phase IV clinical studies alone cannot establish cause-effect relationship. Different individuals may respond to medication in different ways. Every effort has been made to ensure that all information is accurate, up-to-date, and complete, but no guarantee is made to that effect. The use of the eHealthMe site and its content is at your own risk.
If you use this eHealthMe study on publication, please acknowledge it with a citation: study title, URL, accessed date.
Dont Miss: Unable To Control Bowels And Bladder
When Is Surgery Needed For A Prolapsed Bladder
Severe prolapsed bladders that cannot be managed with a pessary and/or behavioral therapy usually require surgery to correct them. There are several different types of surgery depending on the severity of the prolapse and whether or not other organs are affected.
- The bladder is repaired with an incision in the vaginal wall.
- The prolapsed area is closed and the wall is strengthened. This may be done primarily using one’s own tissues or through the use of grafts, which may be biologic or synthetic .
- If one has stress urinary incontinence, this is also corrected.
- Depending on the procedure, surgery can be performed while the woman is under general, regional, or local anesthesia. Most women are discharged home on the same day of surgery.
- Various materials have been used to strengthen pelvic weakness associated with prolapsed bladder. A surgeon should explain in detail the risks, benefits, and potential complications of these materials, and he or she should explain the procedure itself before proceeding with the surgery. Complications related to surgery may include bleeding, infection, pain, urinary incontinence, recurrent prolapse, trouble urinating, and injury to the bladder.
- The cost of surgical treatment will vary with the procedure performed, the length of hospitalization, and the presence/absence of other medical conditions.
- After surgery, most women can expect to return to a normal level of activity after 6 weeks.
Also Check: Muscle Relaxer For Bladder Spasm
Central Nervous System Complications Of Sjogrens Syndrome
In rare instances, patients living with Sjogrens syndrome additionally develop abnormalities within the central nervous system. There may be changes affecting solely the brain or the spinal cord, or both organs get damaged.
Focal deficit disorders are typical for this form of the disease. They may precipitate motor or sensory loss along with hemiparesis , aphasia , dysarthria and movement disorders. Seizures and cerebellar syndrome may occur as well.
Diffuse disorders develop in the form of encephalopathy and aseptic meningitis, dementia, impaired cognitive function or even psychiatric abnormalities.
When the spinal cord gets damaged, patients with Sjogrens syndrome may develop transverse or chronic progressive myelitis. They are also susceptible to neurogenic bladder or end up with Brown-Séquard syndrome or lower motor neuron disease.
Psychological and behavioral changes that might occur along with the basic symptoms and signs of Sjogrens syndrome include a lack of concentration and attention, a subcortical dementia, hysteria, hypochondriasis, depression, dysphoria and sometimes anxiety or panic attacks.
Urinary Incontinence In Women
Up to a third of women in the United States suffer from urinary incontinence . About 33 million have overactive bladder, or OAB, which means they feel urgency, and/or frequency with or without urge incontinence.Research shows that while urinary incontinence risk can be linked to aging, it can also be associated with pregnancy, delivery, and the number of children you have. It doesnt matter whether you have a vaginal or C-section delivery, the risk is still the same. Studies also indicate that women can experience urinary incontinence after menopause due to the drop in estrogen, yet taking estrogen doesnt seem to help those who suffer from UI. As mentioned above, excess weight can also increase your risk of getting urinary incontinence.
There are different types of urinary incontinence. Figuring out what type you have will lead you to proper treatment.
Recommended Reading: Dr Chris Taylor Bladder Control
How Is Uterine Prolapse Diagnosed
If your healthcare provider thinks that you have a prolapsed uterus, he or she will probably do a physical exam to check your pelvis. If you also have urinary incontinence or a feel like you cant empty your bladder, your doctor may do a procedure called a cystoscopy to examine your bladder and urethra.
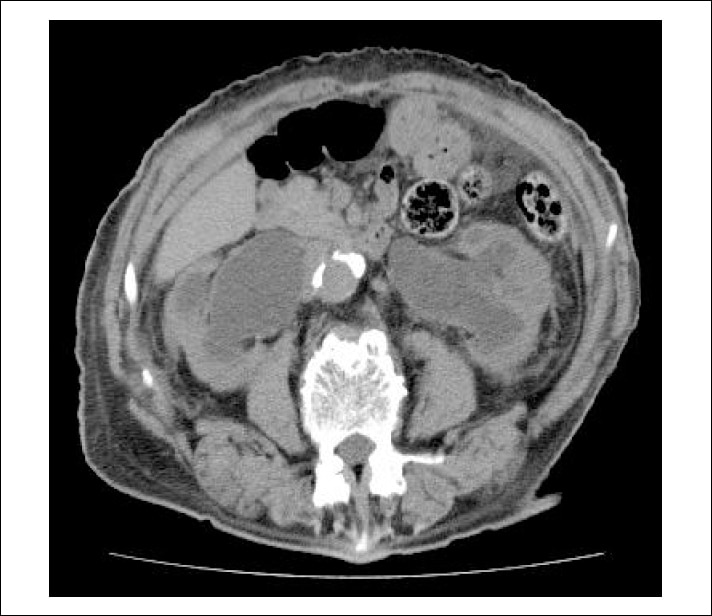
Your healthcare provider might also order an MRI . This procedure uses a magnet and radio waves to create images. This will allow your healthcare provider to get a good look at your kidneys and other pelvic organs.
The Physical Impact Of Incontinence
While many people see incontinence as embarrassing, until youve experienced it yourself you may not realize the true physical impact that it can have on your life.
Of course theres the obvious problem of having to change clothes or bedding often, or running to the bathroom, but incontinence can impact your physical health in other ways too. Many people with regular incontinence suffer from skin infections, due to over-exposure to moisture.
Additionally, many people report reducing their physical activity when they have incontinence. For those who were once active, activities such as running or other high impact exercises are often avoided or stopped completely as the practice may lead to unexpected and involuntary leakage of urine.
Finally, incontinence presents a much greater risk for falls and fractures, especially in older adults.
An elderly person who is focused on getting to the restroom quickly may become unaware of the potential hazards that lie in their path to get to the bathroom , or may become inattentive to controlling their posture or body movements, which increases the risk of falling.
You May Like: Does Diabetes Cause Bladder Problems
Treatment For Symptomatic Bladder Prolapse
If you have symptoms of bladder prolapse it is recommended that, as for people with no symptoms, you make the same lifestyle changes, do pelvic floor muscle training and treat any chronic cough. Make them part of your routine.
However, sometimes prolapse can be more severe and these measures may not be enough on their own to relieve symptoms.
For these cases, there can be two different approaches:
1. Non-surgical approach vaginal pessaries
Some women may prefer this option if they wish to avoid or delay surgery, and it may be the safest option for women who are unfit for surgery.You will need regular check-ups with your healthcare professional if you are using a vaginal pessary long-term.
2.Surgical approach
In some cases, when all other management options have failed to help with the symptoms, or when a woman does not want to use a pessary, surgery may be necessary. The type of surgery used will depend on your combination of prolapse and urinary tract symptoms. Your doctor will discuss the available surgical techniques with you.It is common to have a urinary catheter inserted during the operation to rest your bladder for a day after surgery, but this will depend on the procedure you have. Recovery from surgery takes about six weeks. You doctor will advise you about how to look after yourself during the recovery period, and a physiotherapist can recommend appropriate exercises.
Suggestions may include:
- resting each day.