How Is Urinary Incontinence Treated
You and your doctor or nurse will work together to create a treatment plan. You may start with steps you can take at home. If these steps do not improve your symptoms, your doctor or nurse may recommend other treatments depending on whether you have stress incontinence or urge incontinence or both.
Be patient as you work with your doctor or nurse on a treatment plan. It may take a month or longer for different treatments to begin working.
Incontinence In Alzheimer’s Disease
People in the later stages of Alzheimers disease often have problems with urinary incontinence. This can be a result of not realizing they need to urinate, forgetting to go to the bathroom, or not being able to find the toilet. These tips may help:
- Avoid drinks like caffeinated coffee, tea, and sodas, which may increase urination. But dont limit water.
- Keep hallways clear and the bathroom clutter-free, with a light on at all times.
- Provide regular bathroom breaks.
- Use underwear that is easy to get on and off, and absorbent briefs or underwear for trips away from home.
Visit Alzheimers Disease: Common Medical Problems for more tips.
Treatment Options For Urge Incontinence
Treatments for this type of condition also should address the underlying cause, such as better diabetic control weight loss or altering the lifestyle with limitation of bladder irritants, such as caffeine and carbonated beverages.
Medications that relax bladder muscles are commonly used as first-line therapeutic options. The most commonly reported side effects include dry mouth, constipation and low blood pressure. Recently, bladder muscle Botox injections are being used in patients who have severe symptoms. Injections offer reasonable improvements in symptoms for six months with common side effects being related to urine retention or frequent urinary tract infections.
Sacral nerve root modulation â the surgical implantation of a device that helps modulate the neuronal circuitry to render the bladder more receptive to urine with decreased urgency symptoms â is a viable option for women with severe symptoms, especially those who do not respond to conventional first- and second-line treatments.
Although urine incontinence is common, it is not normal. Therefore, appropriate evaluation is necessary to determine the type and cause of this problem. Treatment options are available to help women optimize quality of life. Discussing the issue with a health care provider is the first and most important step to consider.
Watch this video to learn more about urinary incontinence treatments including sacral neuromodulation therapy:
Topics in this Post
Read Also: How To Get Rid Of Bladder Spasms
Bladder Leakage Or Urine Leakage Is Common If You Struggle With Bladder Leakage You Are Not Alone
- Bladder leakage does not discriminate and affects both men and women however, women are two times more likely to be affected.1
- Approximately 18 million women in the U.S. suffer from bladder leakage2
- Bladder leakage occurs in 25% of women over the age of 18.2
- 80% of those affected by bladder leakage can be cured or improved.3
- While older individuals are more likely to be affected by bladder leakage, it still occurs to younger women.4
How To Get Help For Female Urinary Incontinence
Still feeling unsure about your first step? Remember, incontinence doesnt have to stop you from enjoying daily life on your terms. Getting the right diagnosis and treatment can be a life changer.
If you think that you might have urinary incontinence, reach out to one of our primary care doctors. Well answer any questions you may have and guide you to treatment that will work for you. If specialty care is needed, well refer you to our team of compassionate urogynecology specialists.
You May Like: Unable To Control Bowels And Bladder
How Is Incontinence Treated
There are many different factors that your healthcare provider will consider when creating a treatment plan for your incontinence. The type of incontinence and the ways it affects your life are both big considerations. Your provider will also talk to you about the type of treatment you are most comfortable with. There are three main types of treatment you can explore for incontinence medications, lifestyle changes and surgery. Each option has pros and cons that your provider will discuss with you.
Medications to treat incontinence
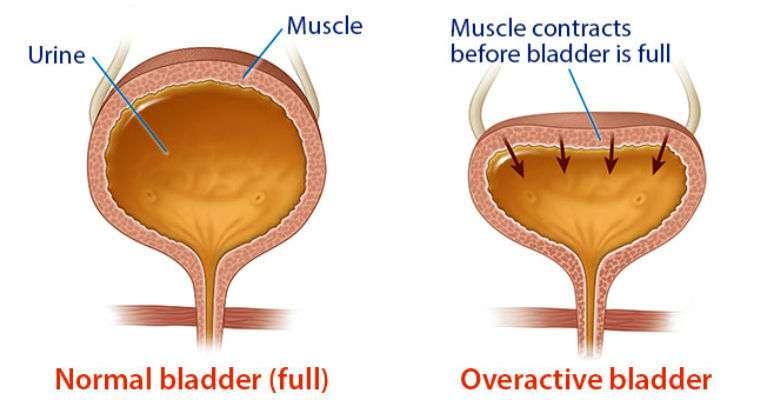
There are quite a few medications that can reduce leakage. Some of these drugs stabilize the muscle contractions that cause problems with an overactive bladder. Other medications actually do the opposite thing relaxing muscles to allow your bladder to empty completely. Hormone replacement therapies can often involving replacing estrogen thats decreased during menopause may also help restore normal bladder function.
In many cases, medications can work very well to return normal function to the bladder. Your provider will carefully select a medication that matches your specific needs. Often, your provider will start you on a low dose of the medication and then increase it slowly. This is done to try and reduce your risks of side effects and to keep track of how well the medication is working to treat your incontinence.
Common medications that can be used to treat incontinence include:
Lifestyle changes to manage incontinence
Causes Of Urge Incontinence
The urgent and frequent need to pass urine can be caused by a problem with the detrusor muscle in the wall of the bladder. The detrusor muscles relax to allow the bladder to fill with urine, then contract when you go to the toilet to let the urine out.
Sometimes the detrusor muscle contract too often, creating an urgent need to go to the toilet. This is known as having an ‘overactive bladder’. The reason your detrusor muscle contracts too often may not be clear, but possible causes include:
- drinking too much alcohol or caffeine
- poor fluid intake this can cause strong, concentrated urine to collect in your bladder, which can irritate your bladder and cause symptoms of overactivity
Stopping these medications, if advised to do so by a doctor, may help resolve your incontinence.
Also Check: What Can You Take For Bladder Pain
Fast Facts On Urinary Incontinence
- Urinary incontinence is more common in females than in males.
- There are a number of reasons why urinary incontinence can occur.
- Obesity and smoking are both risk factors for urinary incontinence.
Urinary incontinence is when a person cannot prevent urine from leaking out.
It can be due to stress factors, such as coughing, it can happen during and after pregnancy, and it is more common with conditions such as obesity.
The chances of it happening increase with age.
Bladder control and pelvic floor, or Kegel, exercises can help prevent or reduce it.
Treatment will depend on several factors, such as the type of incontinence, the patients age, general health, and their mental state.
A Good Alternative To Surgery
Bladder supports are often a good alternative to surgery. Theyre relatively comfortable and non-invasive, and you can wear them only when you need them.
A number of more active patients may use bladder supports because they just need something that will help when theyre being more physically active, says urologist Sandip Vasavada, MD.
Dr. Ferrando says theyre also a good option for women who simply want to avoid the possible risks or complications of surgery. So theyre not looking for surgery, they just want to manage it when theyre active, she says.
Also Check: How To Increase The Size Of Your Bladder
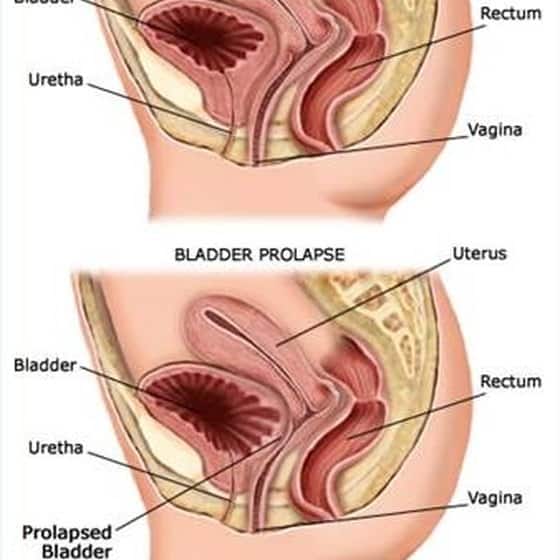
When Is Surgery Needed For A Prolapsed Bladder
Severe prolapsed bladders that cannot be managed with a pessary and/or behavioral therapy usually require surgery to correct them. There are several different types of surgery depending on the severity of the prolapse and whether or not other organs are affected.
- The bladder is repaired with an incision in the vaginal wall.
- The prolapsed area is closed and the wall is strengthened. This may be done primarily using one’s own tissues or through the use of grafts, which may be biologic or synthetic .
- If one has stress urinary incontinence, this is also corrected.
- Depending on the procedure, surgery can be performed while the woman is under general, regional, or local anesthesia. Most women are discharged home on the same day of surgery.
- Various materials have been used to strengthen pelvic weakness associated with prolapsed bladder. A surgeon should explain in detail the risks, benefits, and potential complications of these materials, and he or she should explain the procedure itself before proceeding with the surgery. Complications related to surgery may include bleeding, infection, pain, urinary incontinence, recurrent prolapse, trouble urinating, and injury to the bladder.
- The cost of surgical treatment will vary with the procedure performed, the length of hospitalization, and the presence/absence of other medical conditions.
- After surgery, most women can expect to return to a normal level of activity after 6 weeks.
How Does The Bladder Work
To better understand bladder leakage, it helps to know how the urinary system works. Urinary function starts with your brain and spinal cord, which work together to direct the urinary system.
When your urinary system is functioning normally, you are able to control when to hold and release urine. When your bladder becomes full, it sends a signal to your brain, which in turn sends a message to the bladder to release urine into the urethra. The urethral sphincter muscle, which surrounds the urethra, opens and closes the bladder neck it will contract to temporarily hold urine, or release itself to let urine out of the urethra and your body.
There can be several reasons why your bladder stops functioning correctly. Your brain may no longer properly signal the bladder, the sphincters do not squeeze strongly enough, or both. Alternatively, there could be a problem with the bladder muscle itself or the nerves that control these muscles where the muscle either contracts too much, or not enough. 5
Also Check: How To Fix Bladder Incontinence
History And Physical Examination
A preliminary diagnosis of urinary incontinence can be made on the basis of a history, physical examination and a few simple office and laboratory tests. Initial therapy may be based on these findings. If complex conditions are present or if initial treatments are unsuccessful, definitive specialized studies are required. Because urinary incontinence is a common condition, patients being examined for another problem may mention episodes of urinary incontinence. For instance, patients presenting with cold symptoms may remark that every time they cough, they âleakâ urine. Rather than attempt a complete evaluation for urinary incontinence during that visit, the physician can ask a few simple screening questions.
Table 1 lists a few key questions that can provide information on the severity of urinary incontinence and help distinguish the major subtypes. If the patient answers affirmatively to these screening questions, a 24-hour âbladder diaryâ can be given to the patient to complete . The diary entries can then be reviewed at a subsequent office visit. An algorithm for the evaluation and treatment of urinary incontinence is provided in Figure 2.
How Is It Diagnosed
Your physical therapist will perform a thorough exam. Their goal is to identify the causes of your urinary incontinence. They will ask you to describe your symptoms and your daily experiences, and will assess:
- The muscles of your pelvis, hips, and lower back.
- Your coordination, strength, and flexibility.
- Whether you have pain in your pelvic floor muscles.
Your physical therapist also may refer you to a doctor for more tests to aid in diagnosis. These may include:
- Urodynamic testing .
- Ultrasound or MRI to show any pelvic floor muscle problems.
Read Also: Sea To Summit Water Bladder
Keeping A Bathroom Journal
You may be asked to keep a bathroom journal before or after your appointment. In your journal, youll log all your bathroom trips and bladder leakage or issues. It can also be helpful to record what you eat and drink in your bladder journal. This record will help your doctor get a more accurate idea of your symptoms and how often they occur. Keeping a journal can also determine what triggers your need to pee or any accidents.
Treatments To Improve Pelvic Floor Muscle Function
Your physical therapist will teach you how to find your pelvic floor muscles. They will design an exercise program based on your specific condition. The goal of these exercises is to help you improve your pelvic floor muscle function, to better control your bladder.
Your physical therapy treatment plan may include:
Pelvic floor exercises. Pelvic floor contractions involve squeezing the sphincter muscles while imagining that you are trying to stop urine flow. Both the contraction and full release of the muscles is the goal in training.
Exercises to improve muscle strength. Your physical therapist will teach you specific exercises to increase awareness and movement, to stretch and to strengthen your muscles. Improving pelvic floor muscle strength helps support proper bladder function.
Biofeedback. This treatment depends on your symptoms. Your physical therapist will discuss this option with you. If you are comfortable starting this treatment, your physical therapist will use an internal sensor to read and measure pelvic floor muscle activity. The pressure on the probe when you squeeze your muscles will display on a computer screen to show when you have contracted the right muscles. Biofeedback can guide you and help make you aware of the correct way to use your pelvic floor muscles.
Electrical stimulation. Your physical therapist may apply gentle electrical stimulation. This can help make you more aware of your muscle function.
Don’t Miss: Back Pain And Bladder Leakage
What Is Urinary Incontinence
Urinary incontinence is any undesired leakage of urine. A person with the condition also may have trouble starting the urine stream or holding urine. Urinary incontinence involves the muscles of the pelvic floor. These muscles attach to the bottom of the pelvic bones. They run from front to back and create the base of your core . They form a hammock structure that lifts and supports the internal organs. The pelvic floor muscles also:
- Control the sphincter muscles .
- Support the low back.
- Stabilize the pelvic bones.
- Help with sexual function.
Women may be more likely than men to have urinary incontinence. However, men may underreport the condition.
Different types of urinary incontinence include stress, urge, mixed, and functional incontinence, as well as urinary frequency.
Behavioral And Lifestyle Changes For Bladder Leakage Treatment
Bladder leakage treatment is based on the underlying cause and type of urine incontinence. Both men and women may face similar challenges within the treatment plan that may include urgency suppression, bladder training, and lifestyle changes.
A treatment plan usually begins with behavioral and lifestyle changes such as exercises for leaky bladder. Medications may be required alongside behavioral tasks to reduce muscle spasms or health conditions such as prostate enlargement. In severe cases, surgical procedures may be necessary.
Also Check: What Are The Chances Of Surviving Bladder Cancer
Pads And Other Urinary Incontinence Products For Daily Leaking
A simple yet effective way to manage a leaky bladder is to wear a protective pad or liner during the day.
There are specific pads available for bladder leakage, which are different than the ones youd wear during menstruation. For example, Poise Ultra Thin pads have thin, protective layers that are made specifically to absorb urine.
Results are fairly immediate but these devices arent for everyone, specifically those with pelvic infection, vaginal ulcerations, allergy to product materials, or those who cannot commit to using them regularly.
Disposable inserts, which are like tampons, are another way to prevent leakage. Poise makes one called Impressa.
There are also reusable underpants that are similar to disposable pads, but you can wash and wear them multiple times.
How To Talk To Your Doctor About Bladder Leaks
How do you bring up urinary incontinence to your doctor? And what do you say? Hereâs a helpful guide to get the conversation going!
An easy way to begin the conversation is describing the bladder issues you are experiencing. For example, you could start by saying, âI pee a little when I laugh or cough,â or, âI wake up with wet sheets,â or even simply, âMy bladder leaks.â
Every healthcare professional will tell you that the more information, the better. A good diagnosis depends largely on the information you can give your doctor when you talk. The questions listed below can help facilitate a productive conversation about your sensitive bladder with your doctor that will allow you to start discussing next steps.
- When do you experience urinary losses?
- How often do you urinate each day?
- How often do you get up during the night to use the restroom?
- How much liquid do you drink daily?
- Do you experience unexpected leaks? Do you leak when you sneeze, cough or exercise?
- Do bladder leaks prevent you from participating at work or in your social life?
Your healthcare professional may also decide to perform a physical examination. They may be looking to inspect the way your abdomen contracts. They may also check the firmness of your pelvic floor when you cough.
Recommended Reading: How To Fix A Bladder Infection At Home
Prolapsed Bladder Care At Home
For mild-to-moderate cases of prolapsed bladder, the doctor may recommend activity modification such as avoiding heavy lifting or straining. The doctor may also recommend Kegel exercises. These are exercises used to tighten the muscles of the pelvic floor. Kegel exercises might be used to treat mild-to-moderate prolapses or to supplement other treatments for prolapses that are more serious.
Why Am I Leaking Urine All Of A Sudden What Causes Female Urinary Incontinence Can Uti Cause Urine Leakage
Sudden onset of incontinence, or urine leakage, should always warrant a trip to the doctor. There are several different causes of urine leakage and itâs important to identify prior to any treatment being initiated. The more common types of incontinence in women are stress urinary incontinence and urgency urinary incontinence.
Stress urinary incontinence is caused by a weakness in the sphincter muscle of the urethra , a highly mobile urethra, or both. A highly mobile urethra is seen when the pelvic floor tissues are weak and relaxed. Women will experience leakage of urine with activity, such as coughing, laughing, sneezing, and exercising. The most common risk factor for stress urinary incontinence is having a history of a vaginal childbirth, but it can occur in anyone due to other factors such as muscle strength and activity level. For example, women who do very heavy weightlifting may experience stress urinary incontinence while lifting heavy weights, but if they never did such activities, they might not experience incontinence.
Many people have mixed incontinence, with symptoms of both stress urinary incontinence and urgency urinary incontinence causing urine leakage. In this situation the urologist would typically address the type of incontinence that is most impacting your quality of life first, as the treatments are quite different.
Read Also: Bladder Cancer And Enlarged Prostate