How Is Uterine Prolapse Treated
There are surgical and non-surgical options for treating uterine prolapse. Your healthcare provider will pick your treatment path based on the severity of your prolapse, your general health, age and whether or not you want children in the future. Treatment is generally effective for most women. Treatment options can include:
Non-surgical options
- Exercise: Special exercises, called Kegel exercises, can help strengthen the pelvic floor muscles. This may be the only treatment needed in mild cases of uterine prolapse. To do Kegel exercises, tighten your pelvic muscles as if you are trying to hold back urine. Hold the muscles tight for a few seconds and then release. Repeat 10 times. You may do these exercises anywhere and at any time .
- Vaginal pessary: A pessary is a rubber or plastic doughnut-shaped device that fits around or under the lower part of the uterus . This device helps prop up the uterus and hold it in place. A healthcare provider will fit and insert the pessary, which must be cleaned frequently and removed before sex.
Surgical options
What Is Uterine Prolapse Surgery
Uterine prolapse surgery includes various procedures to repair a prolapsed uterus that has slipped out of place. This condition results from damage to or weakening of muscles, ligaments and tissues that hold a womans uterus in place. Uterine prolapse is more common in women who have had children. It can cause protrusion of the uterus into the vagina, pain, urinary incontinence, and other problems.
Uterine prolapse surgery is a major surgery with serious risks and potential complications. You may have less invasive treatment options. Consider getting a second opinion about all of your treatment choices before having uterine prolapse surgery.
Types of uterine prolapse surgery
The types of uterine prolapse surgery include:
-
Ligament suspension lifts the uterus using a mesh material or stitches to attach the uterus or vaginal vault to a strong ligament in the pelvis to support them. This is called a sacrospinous ligament suspension or uterosacral ligament suspension. Sometimes your surgeon lifts the uterus by attaching it to a muscle. This is called an ileococcygeus suspension.
-
Uterine suspension lifts the uterus using a mesh material to attach the uterus to the pelvis. This is called a sacral colpohysteropexy. Another version of the surgery shortens stretched-out ligaments that support the uterus.
Other procedures that may be performed
Procedures can include:
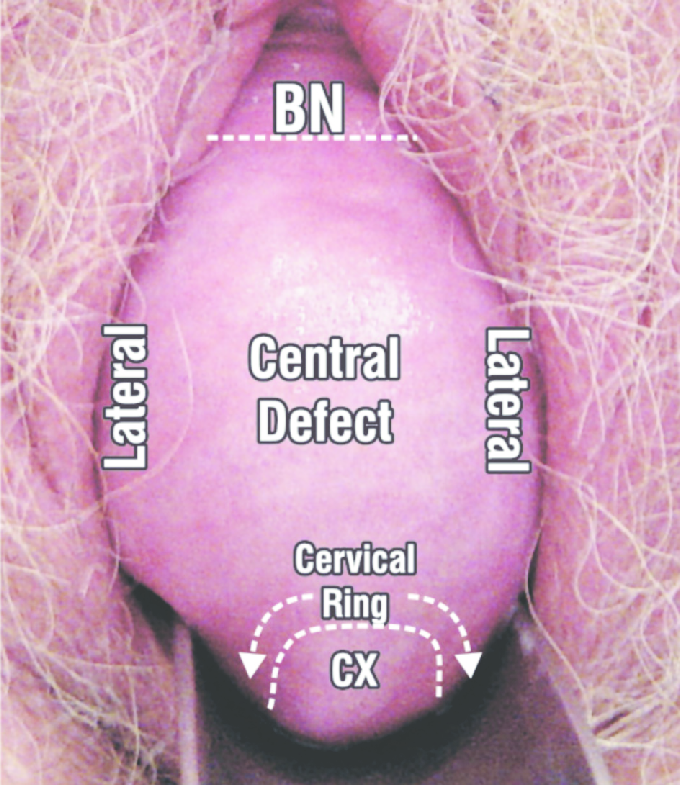
What Is A Pelvic Floor Repair
A pelvic floor repair is the most common surgery for prolapse. It is a broad term used to describe simple surgical repairs of the pelvic floor. More specifically, the term anterior repair refers to correction of the front wall of the vagina and posterior repair refers to correction of the back wall of the vagina. If the uterus is prolapsing, it may be removed . If you have already had a hysterectomy, then the top of the vagina can be lifted up and supported.
Surgeons often carry out more than one of these repairs simultaneously.
You May Like: What Causes Bladder Control Problems
Will You Use Transvaginal Synthetic Mesh
The FDA has issued several documents on the use of reconstructive materials for pelvic floor surgery. The conclusions to date have been that transvaginal placement of these materials are of uncertain effectiveness and are associated with safety risks. In contrast, use of synthetic mesh for sacral colpopexy or for full-length retropubic or transobturator midurethral slings was considered safe and effective.
Make sure to ask your surgeon plans to use transvaginal mesh and in what way. This way you can weigh the benefits against the risks.
How Effective Is Vaginal Wall Repair Surgery
Vaginal wall repair surgery can stabilize the affected organs. This can reduce bladder and bowel problems, pain and feelings of pressure. After the procedure, about 80 to 90 out of 100 women no longer have problems such as urine leakage or pain during sex at least for a while. There is a lack of research on how well this surgery works compared to pelvic floor exercises and pessaries.
The previously prolapsed organs may slip down again following initially successful vaginal wall repair surgery. Studies have shown that this happens within three years in about 38 out of 100 women who have operations using their own tissue. Using a synthetic mesh reduces this risk.
Also Check: Doterra Oils For Bladder Infection
Women With Previous Hysterectomy
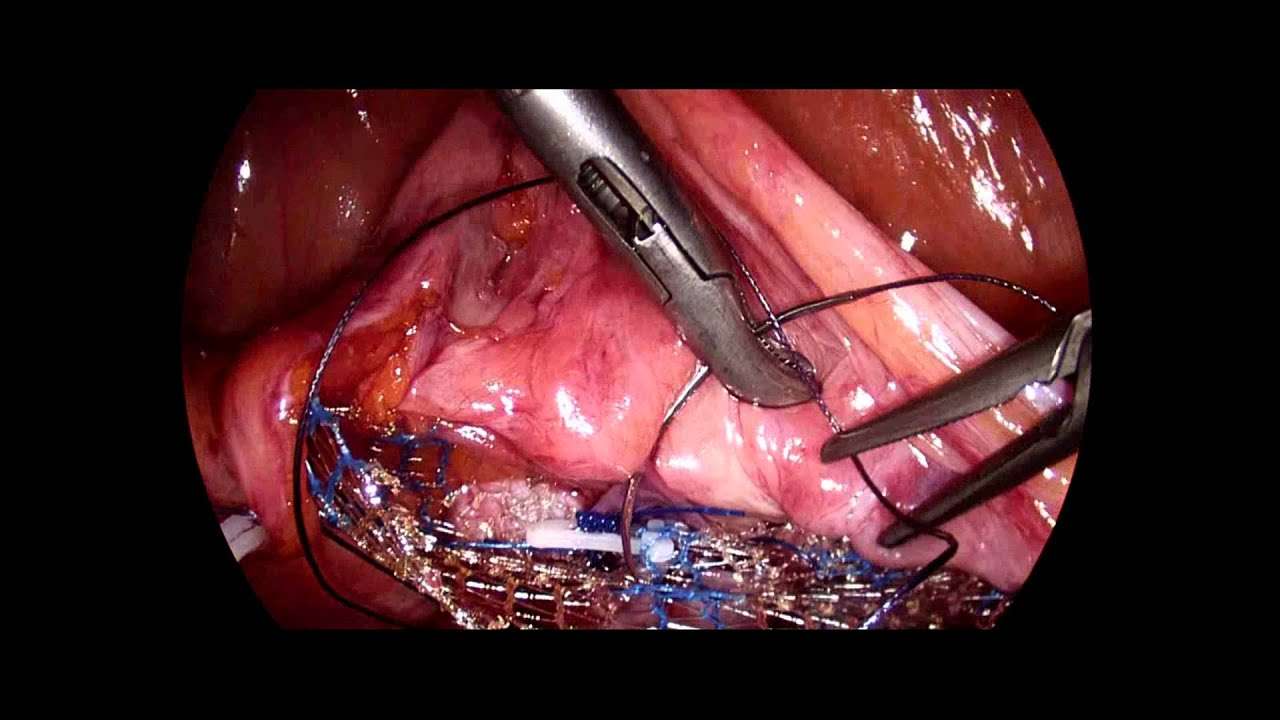
Laparoscopic Sacrocolpopexy
This is the most common operation performed with access from the abdomen for women who do not have the uterus and present with apical prolapse or prolapse of the top part of the vagina.
After entering the abdomen through small laparoscopic incisions and inserting a camera to be able to see inside the abdomen and pelvis, the surgeon dissects the vagina from the bladder anteriorly and the rectum posteriorly.
A graft fashioned in a Y shape is then sutured to the anterior and posterior aspects of the vagina.
The surgeon then opens the membrane that covers the sacral bone and exposed the promontory which is the uppermost part of the sacrum below the lumbar spine. The graft is the sutured to ligaments over the bone providing support and aiming to bring the top of the vagina to its natural elevated position.
Hysterectomy For Uterine Prolapse At A Glance
- A hysterectomy for uterine prolapse removes the uterus that has dropped into the vagina.
- When the symptoms of uterine prolapse become debilitating for a woman and nonsurgical treatments and surgical options to repair the uterus are not appropriate, we recommend hysterectomy.
- Hysterectomy can be performed through an abdominal incision via minimally invasive approaches , open surgery and vaginally. With vaginal surgery, there will be no abdominal incisions or scars.
- Risks of a hysterectomy include clots forming in the legs or lungs, blood loss, urinary retention, injury to adjacent organs, anesthesia complication and infections including urinary tract infections.
- A hysterectomy for uterine prolapse will leave a woman unable to carry a child and is only recommended for women who are beyond their childbearing years.
You May Like: Bcg Chemo For Bladder Cancer
How Effective Is Surgery For Uterine Prolapse
After sacrocolpopexy or sacrohysteropexy to correct uterine prolapse, about 90 out of 100 women no longer have problems such as urine leakage and pain during sex at least for some time.
But there is a risk of the womb dropping down again : In about 23 out of 100 women, it either drops down again or bulges out of the vagina within two years of the procedure.
Sacrocolpopexy and sacrohysteropexy surgery is performed through the abdominal wall, and a synthetic mesh is always used. Various other procedures are performed through the vagina for instance, sacrospinous fixation. In these procedures it is probably possible to operate without using synthetic mesh because compared to operations using the womans own tissue the use of mesh isnt more likely to prevent a prolapse recurrence. But recurrences are more likely after surgery that is performed through the vagina than after sacrocolpopexy and sacrohysteropexy.
Can Prolapse Cause Problems With Sex
Prolapse does not usually cause problems with sex. If prolapse results in bulging of the bladder or rectum into the vagina, the bulge can be easily pushed back into place before intercourse, and most women with prolapse say they don’t notice it during intercourse. Also, if you have a prolapse, you should know that intercourse will not cause any harm to whatever is bulging: your bladder, vagina, uterus or rectum.
Recommended Reading: Types Of Pessaries For Bladder Prolapse
What Is Pelvic Organ Prolapse Repair
Pelvic organ prolapse occurs when the pelvic organs push into the vaginal canal due to the weakening of pelvic muscles. These are repaired in several different ways, either conservatively, with non-surgical treatments or with surgery.
Women who experience urinary incontinence often have this procedure to treat symptoms caused by prolapse and stress incontinence, which is treated with a urethral sling.
The type of surgical procedure conducted depends on the amount of prolapse and the location. Specific procedures include:
Risks Of A Hysterectomy For Uterine Prolapse
As with any surgery there are risks for a hysterectomy for uterine prolapse. Complications may include problems due to the anesthesia, clots forming in the legs or lungs, infection, blood loss, urinary tract infections, urinary retention and injury to adjacent organs.
A hysterectomy will leave a woman unable to carry a child, so this treatment is not recommended for anyone who wants to have children. However, it can be an effective treatment for relieving uterine prolapse symptoms troubling a woman.
Read Also: Overactive Bladder At Night Causes
What Is A Vaginal Mesh Suspension
In some women, the supporting ligaments of the vagina are so weakened or torn that they are beyond repair. For these women, an artificial material can be used to take the place of the weakened ligaments. There are a number of types of materials used to perform this operation, but the most common is a thin, plastic, non-reactive mesh. This mesh is flexible, much like cloth, and can be cut and tailored to fit each woman’s anatomy. The mesh is first sutured onto the top of the vagina as it sits inside the body. The vagina is pulled up to its normal position, and the other end of the mesh is sutured to the connective tissue around the sacral bone to hold the vagina in place. The mesh is very strong, and the operation has a high success rate. However, in rare cases, the body can have a reaction to the mesh since it is foreign material. For that reason, the procedure is reserved for women who have had a previous failed vaginal prolapse surgery and need repeat surgery.
This mesh operation is called a sacral colpopexy and is most often performed through an abdominal incision. However, recent innovations now allow this procedure to be performed laparoscopically by experienced laparoscopic surgeons. In some centers the addition of the Da Vinci Robot has assited with laparoscopic support surgery. As with other laparoscopic procedures, the hospital stay is shorter and the recovery faster.
Can Prolapse Be Treated With Surgery
While prolapse never leads to serious medical illness, it can make some women’s lives uncomfortable or even miserable. Surgical repair of prolapse can be performed through abdominal incisions, incisions high up inside the vagina or, more recently, through small incisions in the navel and lower abdomen through which a laparoscope and small instruments are placed. It is common for more than one supporting structure of the pelvis to develop weakness or tears, so it’s not uncommon to find more than one area is in need of repair. The surgical repair of prolapse is undergoing a re-evaluation. MRI has recently been used to better define the specific areas of damage to muscles and supporting tissues that often lead to prolapse and incontinence.
Also Check: Bladder Infection And Back Pain
Will Sex Be Better If You Have Surgery
To answer this, a recent American study questioned a group of women before and after surgery to repair a prolapse or incontinence. About half of these women were sexually active. Before surgery, 82% of the sexually active women reported being happy with their sex lives, and after surgery, 89% of the women felt happy with their sexual relationship.
However, a study brought out a number of interesting findings. For one, the frequency of intercourse did not change following surgery. And two, while only 8% of the women had pain with intercourse before surgery, 19% noted pain with intercourse after surgery. About one quarter of the women who had a repair of a bulging rectum developed pain with intercourse. About one third of the women who had repair of a rectocele and a bladder suspension had painful intercourse. Unfortunately, the researchers did not ask these women why they were more satisfied with their sex lives even though more of them had painful intercourse.
Another study performed in Sweden may shed some light. This study found that one third of women noted an increased interest in sex after incontinence surgery, and one half of their male partners were more interested in sex. It could be that knowing the repair for the prolapse or incontinence had been addressed was enough to make the couples feel better about sex.
Who Gets Uterine Prolapse
Uterine prolapse is most likely to happen in women who:
- Have had one or more vaginal deliveries.
- Are post-menopausal.
- Have family members who have had prolapse.
Menopause occurs when your ovaries stop producing the hormones that regulate your monthly menstrual cycle . When you havent had a period for 12 straight months, you are considered menopausal. One of the hormones that stops during menopause is estrogen. This particular hormone helps keep your pelvic muscles strong. Without it, you are at a higher risk of developing a prolapse.
Don’t Miss: Ways To Help Overactive Bladder
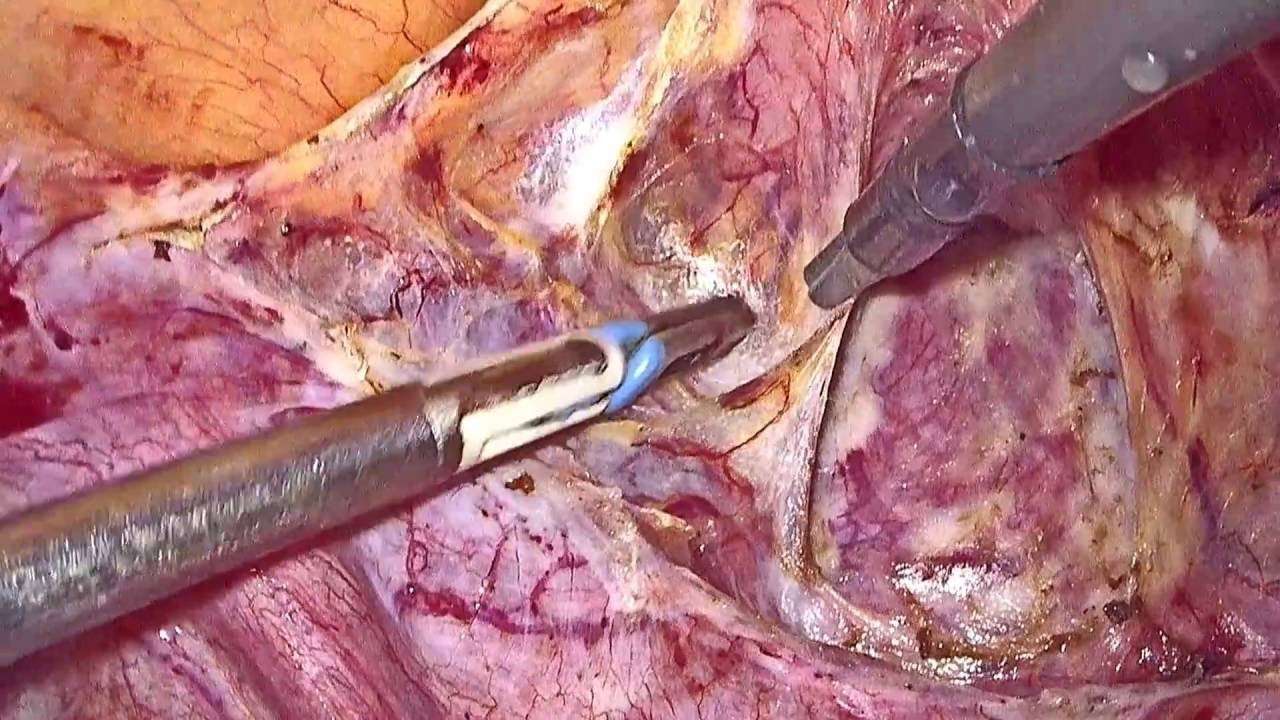
Laparoscopic Pelvic Organ Prolapse Surgery
Laparoscopic pelvic organ prolapse surgery is a minimally invasive procedure used to treat pelvic organ prolapse, a condition in which the pelvic organs drop down and press against the vagina, causing a bulge or protrusion.
Pelvic organ prolapse surgery is used to restore the normal structure and function of these pelvic organs, relieving symptoms that include pain, discomfort, pressure, and urinary and bowel dysfunction.
Laparoscopic pelvic organ prolapse surgery uses very small, specialized surgical instruments inserted through tiny incisions in the abdomen, allowing the surgeon to see and operate on the pelvic organs without having to use a long incision.
This minimally invasive approach offers several advantages over a vaginal approach or traditional open surgery, including:
- Shorter hospital stays
- Less pain
- Faster recovery and return to normal activities
- Fewer complications
- Better view of the pelvic organs and support defects during surgery
- Better suspension of the vagina, through greater visibility and access
- Lower risk of recurrence
Who Performs Uterine Prolapse Surgery
The following specialists perform uterine prolapse surgery:
-
Obstetrician-gynecologists specialize in womens health and .
-
Urologists specialize in diseases and conditions of the urinary tract and the male reproductive organs.
-
Female pelvic medicine and reconstructive surgeons are urologists or gynecologists who have completed specialized training in womens pelvic floor disorders.
Recommended Reading: Does Macrobid Treat Bladder Infection
Can Uterine Prolapse Be Prevented
You may not be able to prevent all cases of uterine prolapse, but there are ways to cut back on your risk of developing a prolapse. A few lifestyle tips that can reduce your risk of prolapse include:
- Maintaining a healthy body weight.
- Exercising regularly. In addition, do Kegel exercises to strengthen your pelvic floor muscles. Remember, check with your healthcare provider before starting any new exercise program.
- Eating a healthy diet. Talk to your healthcare provider or a nutritionist about the best diet for you.
- Stop smoking. This reduces the risk of developing a chronic cough, which can put extra strain on the pelvic muscles.
- Using proper lifting techniques.
What Happens During Vaginal Prolapse Surgery
Vaginal prolapse surgery is usually performed under general anaesthetic. In some cases, it can be performed as laparoscopic surgery. The length of the procedure will depend on the extent of your prolapse.
Your consultant will make incisions inside your vagina and strengthen the supporting tissues with stitches. They may make repairs to both the back and front vaginal walls. Additional supporting stitches may be needed at the top of your vagina or into your cervix. In some cases, surgical mesh may be used. Any wounds will be closed using dissolvable staples.
At the end of your procedure, they may insert a catheter into your bladder to drain urine and your vagina may be packed with material to prevent bleeding. These will be removed in 1-2 days.
You may need to stay in hospital for 3-5 days. Be sure and let a member of our healthcare team know if you are in any pain. You will be able to go home once you are able to move about confidently and you can pass urine with no problem.
Recommended Reading: Botox In Bladder For Incontinence
What Are My Other Surgical Options
Ask your physician if he or she is aware of new, minimally invasive procedures.
Women need to be their own best advocate, which is why getting a second opinion is always good practice. Since there are different surgical options for treating pelvic organ prolapse, getting a second opinion is a way you can ask questions about how the surgery will be performed, the recovery time, and possible complications.
When To Call A Professional
Prolapse of the pelvic organs is generally a nonthreatening problem. You should contact your physician for an evaluation if you are having bothersome symptoms, and you suspect you might have this problem. It is also important to report changes in urinary symptoms to your doctor, since urinary infections are a possible complication of prolapse.
Also Check: Pictures Of Bladder Cancer Tumors
Frequently Asked Questions Expand All
- What are the pelvic organs?
The pelvic organs include the vagina, uterus, bladder, urethra, and rectum. These organs are held in place by muscles of the pelvic floor. Layers of connective tissue also give support.
- What is pelvic organ prolapse?
Pelvic organ prolapse occurs when tissue and muscles can no longer support the pelvic organs and they drop down .
- What are the different types of pelvic organ prolapse?
There are several types of prolapse that have different names depending on the part of the body that has dropped.
-
Cystocele. The bladder drops into the vagina.
-
Enterocele. The small intestine bulges into the vagina.
-
Rectocele. The rectum bulges into the vagina.
-
Uterine Prolapse. The uterus drops into the vagina.
-
Vaginal Vault Prolapse. The top of the vagina loses its support and drops.
Symptoms of POP can come on gradually and may not be noticed at first. A health care professional may discover a prolapse during a physical exam. Women with symptoms experience the following:
Feeling of pelvic pressure or fullness
Bulge in the vagina
Leakage of urine
Difficulty completely emptying the bladder
Problems having a bowel movement
Lower back pain
Problems with inserting tampons or applicators
A major factor in this decision is the severity of your symptoms. The following factors also should be considered: