Patients As Research Team Participants
One key to patient-centered research is engagement of patient and clinical stakeholders. Stakeholders are individuals with personal and or professional insight into the disease process or interventions being studied. This study involves stakeholders in all aspects of the research process in order to assure that the research design, implementation, and dissemination of the results are relevant to clinicians, patients, and caregivers dealing with the SCI on a day-to-day basis. We will assemble a team of people living with SCI to create a Patient Advisory Group, which will provide input regarding the following parameters: meaningfulness of research questions, important characteristics of study participants, comparators, major outcomes, monitor the study progress, ease of questionnaire administration, advocate change in study design where needed, and suggest implementation plans for dissemination of relevant findings.
Study Population And Recruitment
Inclusion and exclusion criteria are listed in Table . To meet eligibility criteria, a patient must have SCI and neurogenic lower urinary tract symptoms. Study inclusion is also limited to patients with acquired etiologies of SCI, such as trauma, tumor without current progressive malignancy, spinal cord stroke, vascular bleed such as an arterio-venous malformation, transverse myelitis without progression to multiple sclerosis, and post-surgical / procedural complications. Any level of SCI, including those with cauda equina, are eligible to participate in the study. Exclusion criteria are progressive spinal disorders , as well as congenital forms of SCI .
Table 1 Study inclusion and exclusion criteria for patients with spinal cord injury
Spinal Cord Injury And Bladder Health Top Tips
Our separate Living with a Urinary Catheter Hydration Guide has lots of helpful hydrating tips even for those without catheters.
Don’t Miss: Non Muscle Invasive Bladder Cancer Guidelines
Nursing Considerations For Bladder Augmentation
The success of this bladder management option hinges on both objective and subjective assessments of the individual’s and caretaker’s ability to provide the necessary follow-up care.
Preoperative. The individual and his or her family are assessed to make sure they understand the procedure and the changes in lifestyle that will be necessary. The family’s ability to accommodate these changes is critical if bladder management is going to succeed .
Perioperative. Prior to surgery, the individual will receive bowel cleansing, antibiotics, a low-residue diet, adequate hydration, and confirmation of the site , as determined by the surgeon and by institution procedure and policy. If the individual will have a stoma, a wound and continence therapist or other qualified health-care provider will mark the site, the location of which will depend on body physique , old abdominal scars, hand function, and usual beltline of clothing. The individual will be evaluated both lying down and sitting up in a chair self-care is easier when the individual can see the stoma.
Postoperative. The focus is on maintenance of homeostasis through adequate hydration and fluid elimination.
Assistance required. Adequate hand function and sufficient cognitive ability are needed to insert the catheter and irrigate the augmented bladder, or a caregiver must be available to do so.
Interference with social/sexual function. Body image issues may need to be addressed if an abdominal stoma is created.
Does The Level Of Injury On My Spine Affect What Problems I Experience
- Yes, however everyones bladder and sphincter act a little differently because the amount of nerve injury is a little different for each person even if you have the same level of injury as someone else.
- Keeping that in mind, the major areas to consider are:
- At or below the sacral micturition center
- Above the sacral micturition center
At or Below the Sacral Micturition Center:
- If the SCI damaged the spinal cord at or near the base of your spine, the sacral micturition center might be damaged.
- When this center is damaged, signals cant be sent to the bladder to tell the bladder to squeeze .
- It the damage is below your sacral micturition center then even though signals are sent towards the bladder, the nerves to the bladder are damaged so the signals do not reach the bladder and your bladder will not squeeze.
- Your bladder will then become very full .
- If you have a weak urinary sphincter, urine will probably overflow from your bladder without your control .
- If you have a strong urinary sphincter, urine may not be able to be released leading to a possible increase in bladder pressure and possible back-up of urine in your kidneys.
Above the Sacral Micturition Center:
Also Check: What Helps With Bladder Infection Pain
Spinal Cord Injury And Bladder Function
If your nerve signals from your spine to your bladder have been affected by your injury, then you may struggle regaining bladder control after a spinal cord injury. You might find it difficult to pass urine or to stop its flow. You may be using a catheter which can be helpful for urinary incontinence after a spinal cord injury, but it could mean you are not passing urine as frequently. When this happens, your kidneys can find it trickier to filter your blood as well as normal and that can make you ill.
This can also trigger a set of symptoms that are part of a syndrome called autonomic dysreflexia. Signs of autonomic dysreflexia include becoming very sweaty, severe headaches and overall feeling very unwell, in which case you might need to stay in hospital. Catheters can also make it easier for bacteria to travel up your urinary system that cause urinary tract infections in persons with spinal cord injury. This is where you may feel ill or possibly need to visit hospital. While your medical team can support you with medications and catheters, you can also use the powerful tool of nutrition to help.
Nursing Considerations For Urethral Stents
The success of this bladder management option will depend upon the individual’s ability to alter care. A thorough objective and subjective assessment is essential prior to surgery.
Preoperative. The focus of care is on the individual’s physical and emotional well-being and on the person’s ability to alter care to facilitate the surgical intervention.
Postoperative. The focus of care is on preventing movement of the stent by altering the individual’s activities of daily living.
Assistance required. Assistance with transfers will be needed until the stent is adequately epithelized. Individuals with paraplegia should use a slide board to prevent extension of the pelvic area. Individuals with tetraplegia will need to use a mechanical lift until the endourethral stents are stabilized, in approximately 13 months.
Care of equipment, cosmesis, and interference with social/sexual functioning. See Nursing Considerations for Reflex Voiding.
Reversibility. The stent is removable, although the procedure can be difficult and result in urethral scarring and/or stricture. Permanent urinary incontinence will not occur, however, the external sphincter will be intact after the stent is removed, creating continence.
Adapted from Joseph, A.C., A. Hixon, J. Giroux, D. Briggs, M. Gardenhire, D. Diaz, and J. Wells. Nursing clinical practice guideline: neurogenic bladder management. Spinal Cord Injury Nursing 15 : 2156.
Recommended Reading: Loss Of Bladder Control When Running
After Spinal Cord Injury
The bladder, along with the rest of the body, undergoes dramatic changes. Since messages between the bladder and the brain cannot travel up and down the spinal cord, the voiding pattern described above is not possible. Depending on your type of spinal cord injury, your bladder may become either floppy or hyperactive .
Grading Of The Scientific Evidence
OBJECTIVE
The objective of this Metaworks, Inc., project was to provide methodologic support services for the development of clinical practice guidelines by the Consortium for Spinal Cord Medicine, sponsored by the Paralyzed Veterans of America. The main component of the project was to conduct a systematic review of the recent English language literature on bladder management of individuals with spinal cord injuries. The focus of the review was the evaluation of various types of bladder management methods, taking into consideration each one’s advantages/indications, disadvantages/contraindications, impact on prevention of upper tract and lower tract complications, and consequences on social life .
BACKGROUND
Bladder management is a crucial element in improved outcomes for individuals with spinal cord injury. The goal is to maintain and preserve a functional, infection-free genitourinary system by preventing upper and lower tract complications with a management system that is compatible with an injury-free lifestyle. The ultimate goal of therapy is to achieve and maintain adequate bladder drainage with low-pressure urine storage and voiding. There is no gold standard for methods of bladder management, so this review is intended to provide insight into each method and to help individuals with SCI choose the approach that will work best for them.
METHODOLOGY
LITERATURE SEARCH
STUDY SELECTION
Don’t Miss: Does Drinking Cranberry Juice Help A Bladder Infection
What Is Bladder Management
Bladder management is an ongoing set of treatments and practices that help keep your bladder and kidneys healthy and free from infection and other problems.
- Bladder management cannot fix or solve the problems caused by your SCI, but it can help you manage them to improve your health and quality of life. With appropriate management you can prevent incontinence and damage to the kidneys.
- You can work with your doctor to choose which bladder management option fits into your lifestyle and maintains bladder and kidney health.
Nursing Considerations For Transurethral Sphincterotomy
Individuals need to be aware that this irreversible surgical procedure will render them incontinent of urine, that urine will be contained in a bag on the outside of the body, and that erectile function may be affected. A thorough assessment for appropriateness of the procedure is essential.
Preoperative. The focus of care is on the individual’s physical and emotional well-being and on the person’s ability to alter care to facilitate the surgical intervention.
Postoperative. The focus of care is on maintaining homeostasis through adequate hydration and fluid elimination .
Care of equipment, assistance required, and cosmesis. See Nursing Considerations for Reflex Voiding.
Interference with social/sexual function. A decrease in erectile function and in the ability to be urine-free during sexual activities may be observed. Although the risk of impotence is reported in the literature , a lower pressure system and removal of the indwelling catheter may improve fertility.
Medications. Alpha-blockers may be given to open the bladder neck to facilitate emptying.
Reversibility. This procedure is permanent and cannot be reversed.
Adapted from Joseph, A.C., A. Hixon, J. Giroux, D. Briggs, M. Gardenhire, D. Diaz, and J. Wells. Nursing clinical practice guideline: neurogenic bladder management. Spinal Cord Injury Nursing 15 : 2156.
You May Like: Bladder Stone Removal In Dogs Cost
What Causes Loss Of Bladder Control After Spinal Cord Injury
The spinal cord transmits messages between the brain and body. However, after a spinal cord injury, messages may not be able to get past the site of injury, resulting in paralysis and loss of sensation below your level of injury.
Many people lose control of bladder functions after a spinal cord injury because the bladder muscles are innervated by some of the lowest nerve segments of the spinal cord. Damage to the spinal cord not only affects functions at the injury site but can also affect all functions below.
The reason why some spinal cord injury patients have normal bladder functions is because they have incomplete SCIs, which means some connections were not damaged by the injury. As a result, they may have some preserved motor control and sensation below their level of injury.
Next, well discuss different types of neurogenic bladder dysfunction that can result from spinal cord injury.
Blood Pressure Responses To Bladder Distention
In the interventional group, systolic blood pressure responses to bladder distention did not differ following ABRT-scES , nor were there significant changes at follow-up compared to baseline or post-training. Furthermore, the change in systolic blood pressure from pre-fill values to values captured at the point of maximum cystometric capacity during the study indicates that ABRT-scES did not attenuate bladder-distention associated increases in systolic blood pressure . However, concerning the usual care cohort, participants receiving ABRT-scES had significantly lower systolic blood pressure responses to bladder distention post-training compared to those in usual care . ABRT-scES sub-group training effects in relation to bladder outcomes were also evaluated. All pre-training bladder and blood pressure outcome measures between these two sub-groups were similar and there were no significant differences in these measures at pre-training, post-training, or follow-up.
Recommended Reading: Sea To Summit Water Bladder
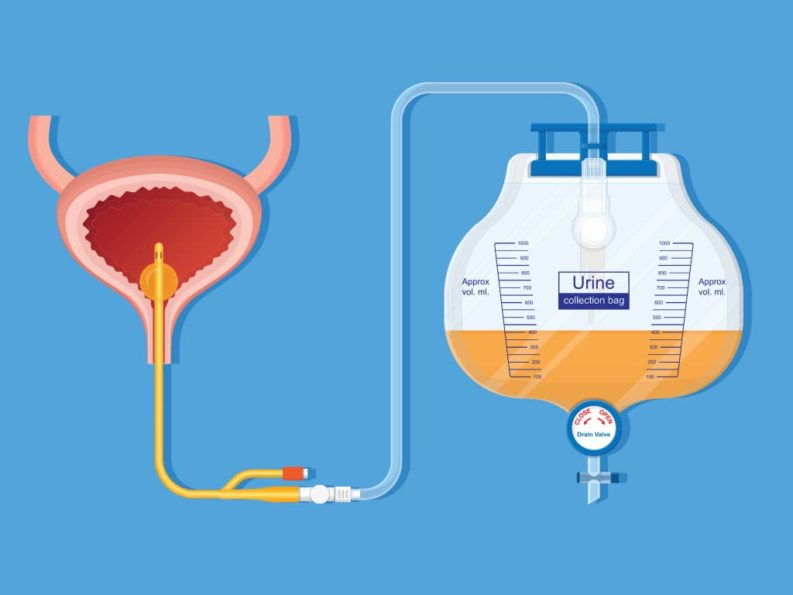
Nursing Considerations For Intermittent Catheterization
Individuals who choose intermittent catheterization for bladder management will need education on proper techniques and care as well as routine follow-up to detect potential complications. There are many variations on intermittent catheter technique and care. One example follows.
Catheter selection: The catheter should be easy to insert without trauma or curling in the urethra. If a latex allergy is present, nonlatex catheters must be used. A nonlatex product with straight tip is recommended.
Hand washing. Hands should be washed or aseptic towelettes used both before and after catheterization.
Technique. Follow the procedure recommended by the prescribing institution, health-care professional, national guideline, or health-care organization.
Catheter care. To control introduction of bacteria into the bladder, catheters must be washed after every use. Rinsing and allowing catheters to air-dry between each use was found to be the most effective means of keeping the bacteria count low on catheters . Catheters should be cleaned with mild soap and water, air-dried, and placed in a paper bag until ready to reuse. If recurrent urinary tract infections are a problem, latex catheters can be sterilized by heating them in a microwave oven .
Recurrent urinary tract infections. Symptoms of UTIs need to be investigated and documented as follows:
Fluids. Fluid consumption should be moderate and spaced throughout the day.
Cosmesis. No changes will be noted.
Management Of Neurogenic Bladder In Sci
A large portion of the survey focused on most common forms of NGB management in SCI and results are described below and depicted in Figs. Figs.33 and 4. Respondents chose between various catheterization methods which were defined in the survey as follows: clean intermittent catherization aseptic intermittent catheterization sterile intermittent catheterization no- touch technique intermittent catheterization indwelling catheter or reflex voiding with use of collection device.
Most common bladder management in outpatient care by continent.
A Females with hand dexterity. B Females without hand dexterity. C Males with hand dexterity. D Males without hand dexterity.
Read Also: Will Amoxicillin Treat A Bladder Infection
Reusable Catheters In Cic Patients
A follow-up question for outpatient healthcare professionals asked HCPs to indicate what percentage of their CIC patient population uses reusable catheters. This reuse practice appears to be more common in Africa, South America, and Asia with the majority of respondents indicating that 75%+ of their patients reuse catheters compared to providers in Australia, Europe, and North America who reported 010% of their CIC population used reusable catheters.
How A Spinal Cord Injury Can Affect The Bladder
The nerves that attach to the bladder arefound in the lower part of the spinal cord in an area called the sacralmicturition. If there is damage to the spine above this region, it can meanthat the nerves dont perform their function properly.
In normal circumstances, for example, if someonewanted to go to the toilet but had to wait, the brain will send a message to thebladder to hold on. If that message cant get through, however, they may not beable to control the flow of urine.
Without the input of the brain, the sacral micturition might send its own messages to the bladder and this can cause a variety problems. These include not only loss of control but may also, for example, prevent the kidneys from draining, potentially causing an infection.
The higher the level of spinal cord injury, the more likely the bladder will be affected. This is commonly called a neurogenic bladder, something which can manifest in a number of different ways.
Recommended Reading: How To Make My Bladder Stronger
Review Articletranslating Promising Strategies For Bowel And Bladder Management In Spinal Cord Injury
Educational resources and clinical care standards require updating.
-
Bowel physiology poorly understood limiting advancement.
-
Provision of sensory awareness to foster independence and health maintenance
-
Emerging neuromodulation techniques to regain functional control
-
Link between physical movement and system function unclear
Effective Bladder Management Following An Sci
Impaired bladder function as a result of paralysis can be challenging, but there are ways to effectively manage the situation.
The most common is intermittent catheterization which involves inserting a tube connected to a bag to collect urine. This is often used in conjunction with medication, for example with botox injections, to prevent the bladder from leaking when the catheter is not in use.
Indwelling catheterization is more permanent and involves inserting the catheter which is then held in place in the bladder by a small balloon. This can be achieved either through the urethra or directly into the bladder via a small incision below the navel.
Alternatives to catheters are Valsalva and Crede voiding techniques which are appropriate if there is an issue with getting the bladder to squeeze. They both involve manually pressing or massaging the bladder to empty it.
Don’t Miss: How To Expand Your Bladder